HIV Rapid Test Errors and Faint Lines: How to Know What’s Real
Quick Answer: If you can’t take PrEP due to allergy, side effects, or access issues, HIV prevention is still possible through consistent condom use, timely HIV testing, emergency PEP, and strategic risk reduction. You are not unprotected, you just need a different plan.
Who This Is For: The People Left Out of the PrEP Conversation
If you're reading this, chances are you're one of the millions who don’t fit the PrEP mold. Maybe you're allergic to one of its ingredients. Maybe your doctor warned you about kidney issues. Maybe the nausea and headaches didn’t feel worth it. Or maybe you simply don’t trust what daily meds might do to your body. All of those reasons are valid, and you’re not alone.
Let’s name the real barriers: racism in healthcare. Transphobia in clinics. A lack of queer-competent providers. Long waits for appointments. Side effects that aren’t taken seriously. Insurance denials. And yes, fear. Fear of judgment. Fear of being labeled. Fear of “doing it wrong.”
This article is for people who deserve HIV protection, even when PrEP isn’t an option. We’ll walk you through every prevention strategy available, who it's best for, and how to build a plan that’s yours. You won’t find scare tactics here, just honest answers, hard data, and care-centered options that meet you where you are.

People are also reading: The Numbers Don’t Lie Why Non-Sex Workers Often Have Higher Undiagnosed STD Rates
Wait, What Exactly Is PrEP and Why Doesn’t It Work for Everyone?
Let’s clarify. PrEP (pre-exposure prophylaxis) is a daily pill or long-acting shot that helps prevent HIV. Most people are prescribed Truvada or Descovy, which are combinations of antiretroviral medications. Taken correctly, PrEP reduces the risk of getting HIV from sex by about 99% according to the CDC.
But not everyone can, or should, take it. Common medical reasons people stop or avoid PrEP include:
Figure 1. Common reasons people discontinue or avoid PrEP.
These are not fringe cases. A 2022 survey by JAMA Network found that up to 1 in 5 people prescribed PrEP discontinue within six months, and many never start due to fear of side effects or affordability concerns.
If PrEP Isn’t for You, What’s Left? Actually, A Lot
Too often, we treat PrEP like it’s the only gate to safety. That’s a myth, and a harmful one. HIV prevention is a toolkit, not a single pill. If PrEP doesn’t fit your body or your life, these other options might:
Figure 2. Real-world HIV prevention tools for people who can’t take PrEP.
None of these require daily medication. Most are accessible regardless of income or insurance. And when used together, their protection can be powerful.
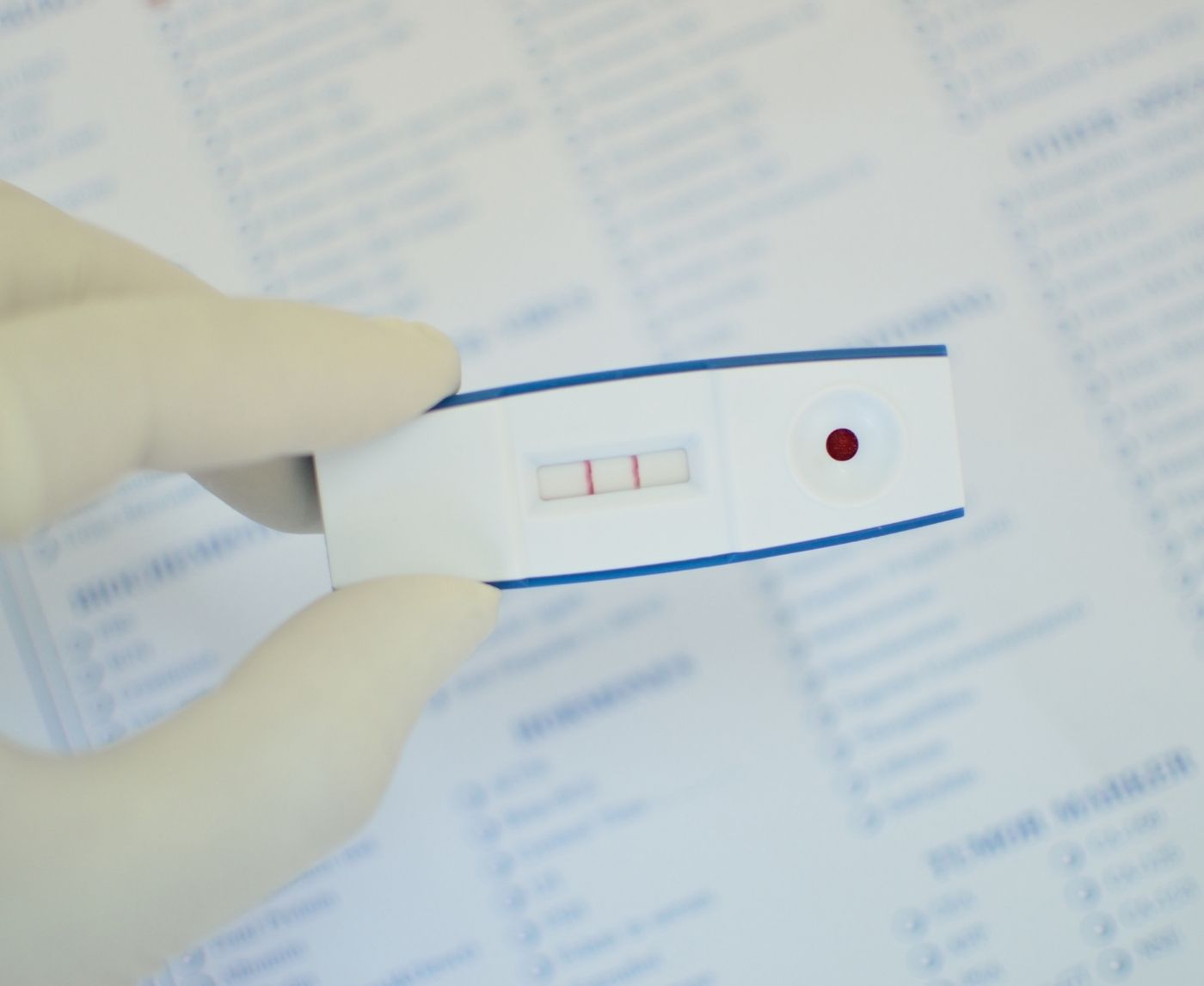
This at-home combo test kit can help you stay on top of your HIV and STD status discreetly, because testing isn’t just for fear, it’s for peace of mind.
Emergency Option: PEP Isn’t PrEP, But It Can Be a Lifesaver
Here’s the scenario: The condom broke. You weren’t on PrEP. And now you’re panicking at 3 a.m., Googling “What to do after HIV exposure.” That’s exactly when PEP, Post-Exposure Prophylaxis, becomes your emergency parachute.
PEP is a 28-day course of HIV medication that can stop infection if started within 72 hours of possible exposure. The earlier, the better, starting within the first 24 hours offers the highest protection. According to the CDC, PEP is up to 80% effective when taken correctly and promptly.
Unlike PrEP, PEP is short-term. It’s used after a risk event, like unprotected sex with someone of unknown status, sexual assault, or a condom failure, not before. It’s also more intense on your body, with a slightly higher chance of side effects like fatigue or nausea. But for many people, it’s a critical tool when PrEP isn’t available, or wasn’t used in time.
If you need PEP, head to the nearest emergency room or urgent care. Don’t wait for a Monday clinic. Time matters.
“I Got Exposed, And I Wasn’t on PrEP”
Janelle, 27, is a Black bisexual woman who stopped taking PrEP after repeated migraines and stomach pain. “It just wasn’t worth how sick I felt,” she said. A few months later, she hooked up with someone at a music festival. They used a condom, but it slipped. She didn’t panic right away, but after a friend mentioned HIV, she started spiraling.
“I remember Googling ‘how long do you have to get PEP’ while crying in my tent,” she recalled. “I didn’t know where the nearest clinic was or if they’d even believe me.”
Janelle ended up calling a telehealth service that referred her to a local urgent care. She started PEP 36 hours after the incident, took every pill despite the fatigue, and tested negative at 4 weeks and 12 weeks.
“It scared the hell out of me,” she said, “but it also made me realize I needed a prevention plan that fit my body, not someone else’s rules.”
Her new routine includes condoms, testing every three months, and knowing where the nearest PEP provider is, just in case.
How Often Should You Test for HIV Without PrEP?
If you’re sexually active and not on PrEP, routine HIV testing becomes your most important safety net. But how often is “routine”?
General guidance from the CDC recommends at least one HIV test per year for anyone sexually active. But if you’re having sex with multiple partners, using condoms inconsistently, or have recently had an STD, testing every 3–6 months is smarter.
That doesn’t mean you need a full lab workup every time. At-home rapid tests (like finger prick or oral swab kits) can provide reliable answers quickly. And if you’re not sure what to test for, our homepage breaks down test kit options by risk level and type of exposure.
Here’s a helpful timeline:
Figure 3. HIV testing frequency guide based on personal risk.
If you’re unsure where you land, start by testing now. Then retest every 3–6 months depending on how your sex life evolves. And don’t let a negative result give you a false sense of security, combine testing with real prevention strategies.
Is It Risky to Be Off PrEP If You’re Sexually Active?
Here’s the honest answer: It depends on what you’re doing, how often, and with whom. Risk isn’t static, and not everyone needs the same tools.
Being off PrEP doesn’t mean you’re automatically “unsafe.” If you’re using condoms correctly, your partners are undetectable (i.e., living with HIV but on treatment), or you’re in a mutually monogamous relationship, you’re likely at low risk. But “low risk” isn’t the same as “no risk.”
On the flip side, if you’re having sex with new or anonymous partners, skipping condoms, or sharing needles, your risk rises significantly. In those cases, PrEP is ideal, but not mandatory. A mix of frequent testing, condom use, partner communication, and emergency PEP access can still offer strong protection.
Think of prevention like a seatbelt system. PrEP is just one part. If you can't use it, wear your other belts tight. Stay tested. Stay informed. And never hesitate to ask for help.
What About Natural HIV Prevention? Let’s Get Real
Search “natural HIV prevention” on TikTok or YouTube and you’ll get everything from garlic smoothies to herbal teas that promise immunity. Let’s be clear: no herb, vitamin, or “immune booster” can prevent HIV transmission. That’s not opinion, it’s science.
We get why people turn to “natural” options. When you’ve been hurt by medical systems, when pills cause side effects, when you don’t trust Big Pharma, it’s tempting to look elsewhere. But HIV is a virus that needs real intervention. Ignoring that fact can leave you exposed, even if your intentions are protective.
That said, you don’t need to abandon holistic care. Eating well, managing stress, supporting your immune system, these all help your body stay strong. But they are not substitutes for condoms, testing, or post-exposure treatments. Real prevention combines emotional safety with physical protection.
Looking for “natural” prevention isn’t silly, it’s human. Just make sure the tools you choose actually work.

People are also reading: The Forgotten STD: Why No One Talks About Donovanosis (Until It’s Too Late)
Partner Status Matters, But It’s Not Always Simple
Many people who stop or skip PrEP are in committed relationships. “I trust my partner,” they say. And that trust might be well placed. If your partner is HIV-negative or living with HIV but undetectable (thanks to treatment), the risk of transmission can be virtually zero.
This is known as U=U: Undetectable = Untransmittable. According to the CDC and dozens of global studies, people with HIV who maintain an undetectable viral load through treatment cannot transmit the virus to their sexual partners.
Still, it takes communication, regular testing, and sometimes negotiation. Here’s a breakdown:
Figure 4. HIV transmission risk based on partner status and viral load.
Your relationship status isn’t a diagnosis. But it is a factor. If PrEP isn’t an option, talk openly with your partner(s) about testing, treatment, and risk tolerance. The more you know, the more empowered you’ll be.
Mental Health and Medical Mistrust: The Hidden Reasons People Avoid PrEP
It’s not always about side effects or allergies. For many, the fear around PrEP is psychological. Daily medication can feel like a reminder of trauma, a symbol of illness, or a loss of control. Others associate it with stigma, especially in communities where even talking about HIV is taboo.
Medical mistrust runs deep, particularly among Black, brown, queer, and trans communities. And that mistrust is earned, from the Tuskegee study to present-day clinic discrimination, the history is real. So if you feel hesitant, skeptical, or just emotionally overwhelmed by the idea of PrEP, you're not broken. You're responding to a system that hasn't always had your back.
The good news? You have options. Prevention doesn't have to come in a pill. It can come in knowledge, in routine, in care. Choosing condoms, knowing your testing schedule, keeping PEP access on your radar, all of that is prevention. And it's valid.
What matters most is that your prevention plan feels safe emotionally, not just physically.
Privacy, Protection, and Power: How At-Home Care Changes the Game
If you’re not on PrEP, you might feel exposed. But what if you could take control of your health without anyone knowing? That’s where at-home testing and discreet support come in.
At-home HIV and STD test kits allow you to check your status privately, on your own schedule, without navigating a clinic or explaining yourself to a stranger. Our kits arrive in plain packaging, no logos, no stigma, no awkward pharmacy pickups.
Results are fast (as little as 15 minutes for rapid kits), and you can test for HIV alone or choose a combo panel for multiple STDs. If you test positive, we provide guidance on what to do next, including confirmation and treatment options. You're never left guessing.
When PrEP isn’t right for you, at-home testing gives you back a sense of power. It says: I care. I’m responsible. I’m in charge.
And sometimes, that’s the most powerful prevention tool of all.
FAQs
1. Can someone actually be allergic to PrEP?
Yep, and it’s more common than most doctors admit. Some people break out in rashes, get itchy all over, or feel weirdly swollen. Others don’t have full-blown allergies but still react badly to the meds. If your body is freaking out after starting PrEP, it’s not all in your head. Talk to your provider about stopping or switching. Don’t push through something that feels wrong.
2. What if I’m scared to take PrEP because of side effects?
That fear is valid. Nausea, headaches, weird dreams, those are all real things people report, especially in the first few weeks. Some bodies adjust. Others don’t. If the idea of feeling worse every day for protection makes your stomach churn, you’re not alone. There are other ways to stay safe that don’t involve forcing your body to adapt to something it clearly doesn’t like.
3. Can I still be protected without PrEP?
Totally. PrEP is powerful, but it’s not the only shield. Condoms still work. PEP works in emergencies. Regular testing keeps you informed. If your partner is on HIV treatment and undetectable, that’s protection too. You can mix and match these tools based on your life, your body, and your comfort. Don’t let anyone tell you “PrEP or nothing.” That’s a false choice.
4. How do I know if I need PEP instead?
Think of PEP as the fire extinguisher, something you grab after something risky happens. Condom broke? Had unprotected sex and not sure of the partner’s status? You’ve got 72 hours (ideally less) to start the meds. You’ll take them for 28 days. It’s not fun, but it can stop HIV before it starts. Don’t wait to see if you “feel fine.” Go. Now.
5. Are at-home HIV tests actually reliable?
Yes, and they’ve come a long way. Some tests use blood from a finger prick (more accurate), while others use saliva. Either way, if you follow the instructions and test at the right time after exposure, you’ll get a solid answer. Plus, no waiting rooms, no weird questions, no lab coat judgment. Just you, your space, and results you can trust.
6. I had sex without protection. No PrEP. What now?
First, take a breath. You’re not the first, and you won’t be the last. If it’s been less than 72 hours, go find PEP. If it’s too late for that, plan to test in about 2–4 weeks, then again at 12 weeks to confirm. In the meantime, stay hydrated, don’t spiral into shame, and make a plan that includes care, not punishment.
7. How often should I test if I’m not on PrEP?
Depends on your sex life. If you’ve got a consistent partner and use protection? Once a year is probably fine. If you’re dating, hooking up, or just being beautifully human with multiple partners, every 3 to 6 months is smarter. Testing isn’t just about panic after a scare, it’s about knowing your baseline and protecting your peace.
8. Can I just use condoms instead of PrEP?
Without a doubt! When utilized properly and with regularity (yes, we're looking at those spontaneous nights out), condoms serve as a powerful tool in the fight against HIV and the majority of sexually transmitted diseases.
9. My partner is HIV-positive but undetectable. Am I still at risk?
Nope, not if they’re truly undetectable. The science is rock-solid here: if someone living with HIV is taking their meds and their viral load is undetectable, they cannot transmit HIV. It’s called U=U, Undetectable equals Untransmittable. Still, regular check-ins and testing for both of you keep that trust strong.
10. Does insurance cover all this stuff, like PEP or home tests?
Usually, yes. Most insurance plans cover PEP, HIV testing, and even some at-home kits. But if you’re uninsured, don’t panic. Community clinics, Planned Parenthood, LGBTQ+ health centers, and sexual health nonprofits often have free or low-cost options. You deserve care, with or without a policy number.
You Deserve Options, Not Ultimatums
Too often, the message is: take PrEP or risk it. But that’s not real life. People react to medications. People lose coverage. People have complicated health histories. And people deserve prevention tools that fit into their actual lives, not just clinical guidelines.
This at-home combo test kit lets you check your HIV and STD status without judgment, stress, or delay. It's not just about avoiding infection, it’s about claiming your power, your autonomy, your health.
You are not reckless for needing another option. You’re human. And there’s a path forward built just for you.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted five of the most relevant and reader-friendly sources.
Sources
2. The Basics of HIV Prevention | HIVinfo (NIH)
3. HIV: PrEP and PEP | MedlinePlus
4. Long-Acting HIV Prevention Tools | HIV.gov
5. What You Should Know About HIV Prevention | ViiV Healthcare
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to stop, find, and treat STIs. He has a no-nonsense, sex-positive approach and is dedicated to making his work available to readers in both urban and off-grid settings.
Reviewed by: M. Reyes, NP, AAHIVS | Last medically reviewed: September 2025
This article is for informational purposes and does not replace medical advice.