How Accurate Is a Syphilis Rapid Test?
Quick Answer: Bethenny Frankel developed a facial bacterial infection from hotel linens, not an STD, but the case sparked confusion online. At-home testing helps rule out infections when symptoms are unclear, especially if you're dealing with unexplained rashes, irritation, or recent exposure.
Who This Guide Is For (And Why It Matters)
If you’ve ever woken up with a rash after sleeping somewhere new, an Airbnb, a friend’s house, a hotel, you’ve probably had the same questions: Is it just irritation? Is it something worse? Could it be contagious? And do I need to test?
This article is for people caught in that blur of symptoms and uncertainty. For the woman back from a solo beach weekend now Googling “STD or razor burn on face.” For the guy who shared a towel at a gym. For anyone who’s felt itchy, unsure, and a little afraid to ask. At-home testing isn’t just about sex. It’s about peace of mind, without shame, clinic visits, or guesswork.
We’ll break down what counts as a test, how timing affects results, the difference between bacterial infections and STDs, and how to choose the right at-home test if you need one. We’ll also explore the science behind Bethenny Frankel’s hotel encounter and why it matters more than just gossip headlines.

People are also reading: Do I Have to Get Tested If I Have No Symptoms but My Partner Did?
What Actually Counts as an STD Test?
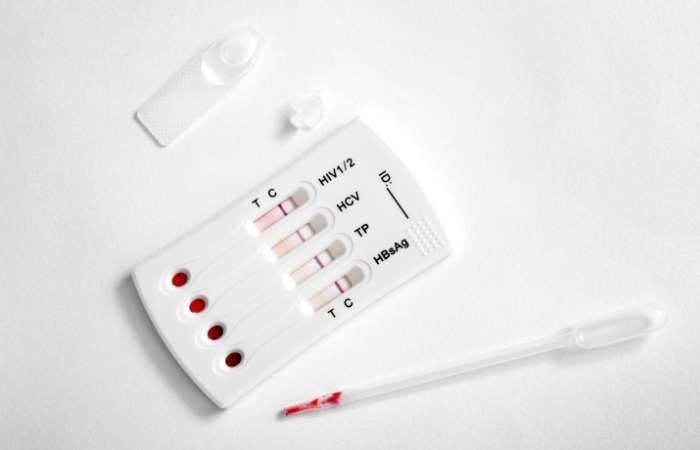
When we say “STD test,” we’re usually talking about lab-grade diagnostics that detect bacteria, viruses, or parasites transmitted through sexual contact. The most common are NAATs (nucleic acid amplification tests), which look for the genetic material of organisms like chlamydia and gonorrhea using a urine sample or swab. Others involve bloodwork, especially for HIV, syphilis, and hepatitis B.
At-home STD tests fall into two broad categories: rapid self-tests you can read in minutes, and mail-in kits that go to certified labs. Both can detect common STDs with high accuracy, especially when used during the right “window period” after exposure. Some also detect bacterial infections that might show similar symptoms but aren’t sexually transmitted. You can explore those options at STD Test Kits. If you're unsure where to start, this all-in-one test kit checks for multiple STDs discreetly and quickly.
As Frankel’s story shows, it’s not always obvious what kind of infection you’re dealing with. That’s why understanding test types, and what they detect, is key.
Window Periods: What to Know for Each STD
A “window period” is the time between infection and when a test can reliably detect it. Testing too early may give a false negative. This is especially important with STDs, where symptoms may appear long after exposure, or not at all.
Figure 1. STD window period by test type. Testing too early can miss infections, so knowing these timelines helps you choose the right moment for accurate results.
At-Home vs. Lab vs. Clinic: Which Test Makes Sense?
Let’s say you wake up with a rash after a hotel stay, like Bethenny Frankel did. Or maybe you notice a burning sensation after a recent hookup, but you're not sure it’s serious. Do you wait it out? Go to urgent care? Panic-Google symptoms?
That’s where knowing your options matters. At-home rapid tests can give you answers in 15–20 minutes for things like chlamydia, syphilis, and HIV. Mail-in kits offer slightly higher accuracy and wider screening options. In-clinic testing, while thorough, may require appointments, time off, and awkward conversations, barriers that push many people toward avoidant behaviors or self-diagnosis online.
Figure 2. Comparing testing methods based on use case, privacy, and detection accuracy.
If your symptoms are mild, testing from home may give you fast reassurance. But if a rash spreads, you’re immunocompromised, or your symptoms include fever or pus, a doctor’s visit is essential. Frankel’s case reminds us: not every skin issue is minor, and not every infection is visible right away.
Is It a Rash or an Infection? Here's How to Tell
Frankel’s red, inflamed face was misinterpreted online as “facial chlamydia”, a term that doesn’t exist medically. But that confusion is real: many STDs cause rashes, bumps, or inflammation, and people often don’t know where the line is between irritation and infection.
Here’s what you need to know. Bacterial skin infections like impetigo or folliculitis (which Frankel may have had) usually come from contact, dirty towels, shared razors, or friction. They can look angry but don’t always signal systemic illness. STDs, by contrast, often cause ulcers, discolored patches, discharge, or internal symptoms, especially when transmitted orally or genitally. In rare cases, infections like syphilis can cause skin lesions that mimic other conditions.
Testing is the only way to tell for sure. Especially if:
- Symptoms persist or worsen after 3–5 days
- You had recent unprotected sex, even oral
- You’ve developed new symptoms beyond the skin
Peace of mind isn’t just emotional, it’s clinical. Testing stops the spiral of “what ifs” and lets you move from fear to facts.
When to Test After a Suspicious Symptom
Imagine this: you return from a ski weekend. A few days later, your chin feels raw. You think it’s windburn, until small red bumps form. Was it the hotel towel? The beard trimmer? The hookup with your ex? You panic, test right away, and get a negative. But you’re still worried.
This is where timing matters. Most bacterial STDs take several days to show up on tests. Testing too early may produce false negatives. A good rule of thumb is to test at least 7 days after potential exposure, but the most accurate results usually come after 14.
Retesting is common and smart. In fact, many at-home test kits come with multiple tests for this reason. If you’re unsure when you were exposed, or if symptoms appear later, take another test after two weeks.
When Should You Retest (Or Not)?
Let’s say your initial test was negative, but the rash hasn’t gone away. Or maybe your partner recently tested positive and now you’re wondering if your results missed something. Do you retest? Or wait it out?
Here’s how to know:
If your symptoms are improving and no new exposure has occurred, retesting may not be necessary. But if symptoms worsen, or your risk changes (like a new partner or symptoms in someone you’ve slept with), a follow-up test is wise. Many experts recommend retesting for chlamydia, gonorrhea, or trichomoniasis at the 30-day mark if you were exposed recently or had symptoms that didn’t resolve.
And if you were treated for an infection, don't test again too soon. For bacterial STDs, fragments can linger and create false positives for a few weeks. Most guidelines suggest waiting 3–4 weeks post-treatment to avoid confusion.
Retesting isn't about paranoia, it's about confirming healing and protecting partners. If you're navigating this alone, STD Test Kits offers discreet support with clear instructions and no judgment.
Privacy, Discretion, and the Shame Factor
Frankel’s story resonated in part because she was willing to say what most people hide: she had a gross, painful skin issue, and she didn’t know what it was. That kind of honesty matters. For many people, especially those dealing with possible STDs, shame keeps them from testing or even talking to someone.
At-home testing helps break that cycle. Kits arrive in discreet packaging, with no sexual health labels or pharmacy pickups. You control the timeline. You decide who sees the results. And you get answers fast, often within minutes for rapid tests, or 2–3 days for lab-based kits.
For people in rural areas, LGBTQ+ communities, abusive relationships, or high-profile careers, that discretion can mean everything. And in 2026, there's no reason to trade health for privacy. You can have both.
What If You Do Test Positive?
Most people assume the worst. That a positive STD test means your life just changed. That you’re “unclean,” or your partner will leave, or your future relationships are doomed. None of that is true. Most bacterial STDs are easily treatable with antibiotics. Even viral ones, like herpes or HIV, are manageable with medication and long-term care plans.
First, confirm your result. If you tested with a rapid at-home kit, follow up with a lab or mail-in confirmatory test. Then, if positive, contact a healthcare provider for treatment. You may also want to notify recent partners, anonymously if needed.
Frankel didn’t have an STD, but she had something contagious. Her decision to speak out helped others realize that symptoms don’t always mean shame, and testing doesn’t mean you’ve done something wrong. It means you're taking care of yourself.
If you're ready to take that next step, order a rapid chlamydia test or combo test kit to get clear answers from home.
People are also reading: Scared to Have Sex Again After an STD?
FAQs
1. Can you really get an STD from a towel?
You probably won't get a bacterial skin infection, but it is possible, especially if the towel was wet, used more than once, or not washed well. You can't get chlamydia or gonorrhea by sharing towels; you have to be close to someone and exchange fluids. If something doesn't feel right after a trip or a hookup, though, trust your gut and get tested.
2. What’s the deal with “facial chlamydia”? Is that even a thing?
Nope, not in the way TikTok makes it sound. While chlamydia can infect the eyes (ocular chlamydia) or throat after oral sex, there’s no medical condition called “facial chlamydia.” Most face rashes come from contact irritants, bacteria, or allergies, not STDs.
3. I thought my rash was from a razor. Now I’m not so sure. Should I test?
If it’s spreading, blistering, or sticking around longer than your typical post-shave irritation, yes, testing can help rule things out. Plenty of people confuse early STD symptoms with razor burn, yeast infections, or heat rashes. When in doubt, don’t spiral, just test from home and move on.
4. I hooked up last week and now my chin’s breaking out. Coincidence?
Maybe. Or maybe not. Some STDs, like herpes, can show up as bumps or sores near the mouth a few days after exposure. Other infections might not show symptoms at all. The only way to know? Test, and repeat if symptoms change or worsen.
5. Are at-home STD tests as good as clinic tests?
Many are. Rapid kits from verified brands offer accuracy above 95% for common STDs when used correctly and at the right time. Lab-based mail-in tests are even more sensitive. Think of them as the Uber of diagnostics: same destination, different vibe.
6. What if I test negative but still feel weird?
Retest after a week or two. Some infections take time to show up. And remember, not all weirdness is STD-related. You could be dealing with contact dermatitis, a fungal rash, or even stress-induced flare-ups. If testing’s clear but your body isn’t happy, a visit to a doctor is still worth it.
7. I’m embarrassed. Do I have to tell my partner if I test positive?
It's tough, but yes. Not because you’re in trouble, but because it’s how we protect each other. The good news: many services offer anonymous partner notification. You don’t have to do it face to face. You just have to care enough to share.
8. How soon after a new partner should I test?
Ideally, wait 7–14 days post-exposure for the most accurate results. But if symptoms appear sooner, don’t wait, test now, and plan to retest later. Testing is like brushing your teeth: it’s not a reaction, it’s a routine.
9. Does a rash always mean something serious?
Not at all. Our skin reacts to a million things, friction, sweat, detergent, hormones, anxiety. But if your rash came out of nowhere, looks unfamiliar, or arrived after a new sexual encounter, testing helps you know what’s what. It’s not overkill. It’s ownership.
10. Why do people wait so long to get tested?
Fear, mostly. Or shame. Or they don’t know what’s normal. We get it. That’s why at-home kits matter, they let you skip the awkward parts and just take care of yourself. Quietly. Confidently. On your own terms.
You Deserve Answers, Not Assumptions
Bethenny Frankel’s vacation rash was dramatic, public, and misinterpreted, but it also sparked something important: a conversation about how infections happen, how we respond, and what tools we have to feel safe. You don’t need to be a celebrity to take your symptoms seriously. And you don’t need a doctor’s permission to start getting answers.
At-home testing gives you clarity, autonomy, and dignity. Whether it’s a strange rash, a nagging itch, or just a gut feeling that something’s off, testing is care. And care is powerful.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources. Every external link in this article was checked to ensure it leads to a reputable destination and opens in a new tab, so you can verify claims without losing your place.
Sources
1. Bethenny Frankel’s Facial Infection Blamed on Hotel Towels
2. Mayo Clinic: Folliculitis Symptoms and Causes
4. Laundry and Bedding Infection Control – CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: J. Kendall-Rose, NP-C | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.






