How Long Should You Wait to Retest for STDs After Antibiotics?
Quick Answer: STD testing is not routinely offered to divorced or older women unless you specifically request it, even if you’re sexually active again. Many STDs show no symptoms, so proactive screening is essential after new partners or divorce.
When Silence Is a Symptom Too
Doctors don’t always mean harm when they skip STD screening. Sometimes it’s unconscious bias: they assume you’re not at risk. Other times it’s time pressure, awkwardness, or even outdated guidelines. But the result is the same, divorced women get left behind in conversations about sexual health.
A CDC report shows that STD rates have been rising fastest among adults over 40, especially women who reenter dating after long-term relationships. Yet clinicians often reserve routine screening recommendations for those under 25 or individuals perceived as “high risk.”
That perception leaves women like Caroline, and maybe you, out of the equation entirely. And since many STDs don’t show immediate symptoms, it’s easy to miss the danger until it becomes painful, spreads to partners, or leads to long-term health consequences like pelvic inflammatory disease or infertility.

People are also reading: I Might Have Been Exposed to Hep B. What Now?
Why Doctors Don't Bring It Up
Let’s break it down: why would a trained medical professional avoid asking you about your sex life or offering a test?
Several reasons come up again and again:
Figure 1. Why STD testing is skipped for divorced women, despite rising risk.
The Rise in STDs Among Divorced and Midlife Women
The National Institutes of Health and Planned Parenthood have found that more women over 35 are getting STDs, especially HPV, trichomoniasis, and chlamydia, after a new relationship or divorce. This is a quiet epidemic. It's even worse that people are embarrassed to ask for a test.
People who start dating again often get HPV, for example. It's not about being promiscuous; it's about not being immune to new partners. Even if you only have one partner and are careful, you could still be at risk for herpes and chlamydia without knowing it.
The Journal of Women's Health published a study in 2022 that showed that women over 40 were much less likely to have been tested for STDs in the past year, even if they had new or more than one sexual partner.
“My Doctor Said I Didn’t Need to Worry”
Lauren, 45, started seeing someone she met through a mutual friend. It had been five years since her divorce, and she was finally ready to be intimate again. She asked her doctor during a routine check-up if she should be screened “just in case.”
“She literally told me, ‘You’re not 22 anymore, you’re fine unless something hurts.’ I almost believed her. But something in my gut told me to get tested anyway.”
Lauren ordered a discreet at-home STD combo test. Her results? Positive for chlamydia.
“I was floored. I hadn’t had symptoms, nothing. If I’d listened to her, I would’ve just passed it to him or ended up with something worse.”
She got treatment fast. And more importantly, she got clarity. Testing isn’t just about risk, it’s about respect for yourself and your partners.
Want Peace of Mind? You’ll Probably Have to Ask for It
Here’s the truth most clinics won’t say out loud: unless you’re under 25, pregnant, or showing very specific symptoms, your provider likely won’t offer a routine STD screening panel. That means it’s on you to ask. Directly.
And no, it’s not awkward. It’s proactive. You can say:
“I’ve recently become sexually active again and I’d like a full STI screening, even if I don’t have symptoms.”
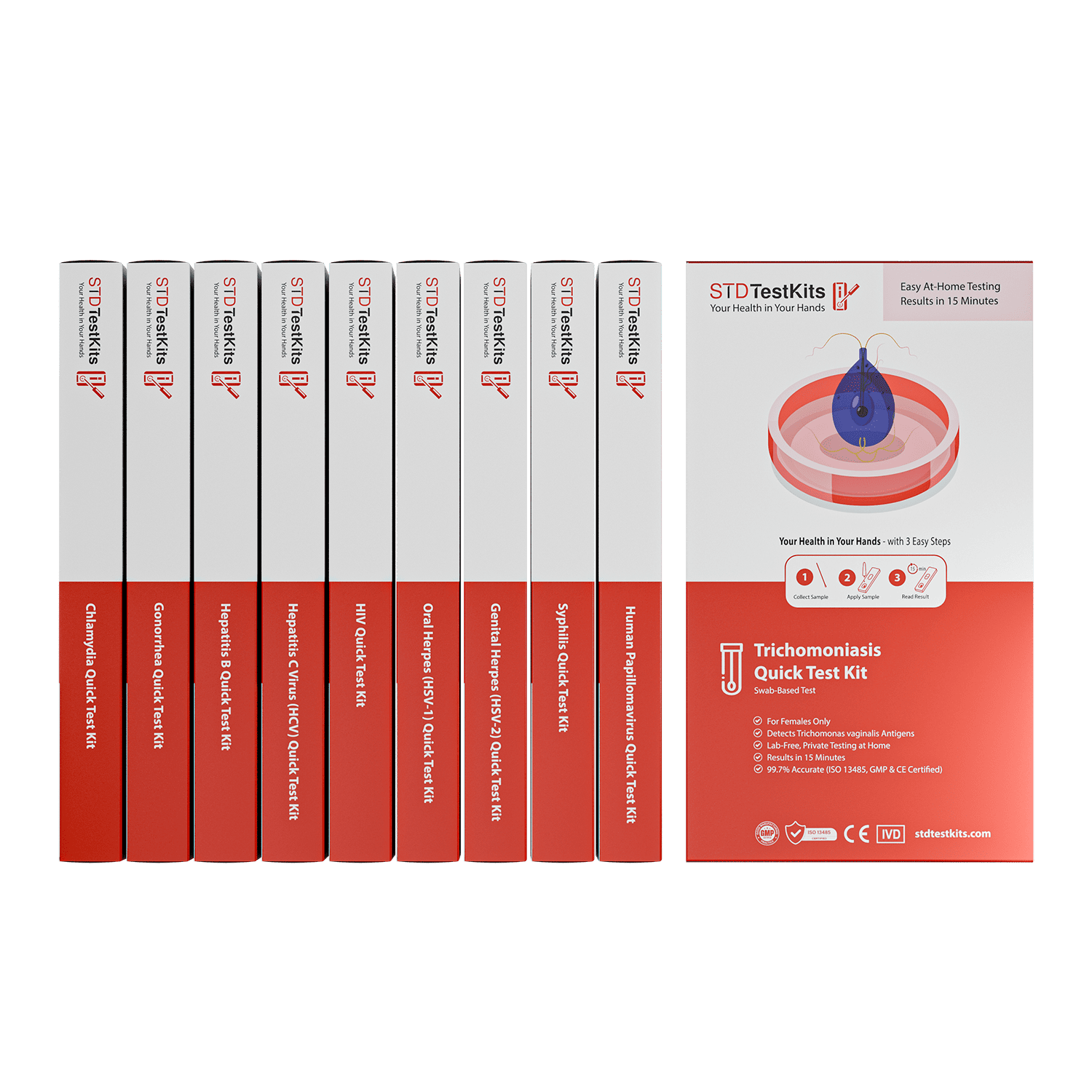
Or you can skip the clinic altogether. At-home test kits offer the same lab-grade reliability, mailed to you in discreet packaging. Results take minutes, not weeks.
If your head keeps spinning, peace of mind is one test away.
At-Home vs. In-Clinic Testing: What Actually Works?
For many divorced women, the idea of walking into a clinic and asking for an STD test feels mortifying. You’re already navigating grief, identity shifts, and maybe a new partner, do you really need fluorescent lighting and judgmental intake forms too?
The good news? You have options. At-home testing is now accurate, accessible, and fast. And it’s not just for twenty-somethings on TikTok. Here’s how the main testing routes compare.
Figure 2. Choosing the right STD testing method based on privacy, speed, and comfort.
Retesting After Divorce: It’s Not Just a One-Time Thing
So you got tested after your first post-divorce hookup. That’s more than most people do, and it’s a smart first step. But here’s what no one really tells you, especially not in that 15-minute doctor’s appointment or on the apps where everyone swears they’re “clean”: one test doesn’t mean you’re covered forever. If you're dating again, having more than one new partner, or even staying with one partner whose status is unknown, retesting isn’t just optional. It’s essential.
Every STD has what’s called a “window period.” That’s the stretch of time between when you’re exposed and when a test can actually detect the infection. It's not immediate. You might feel totally fine, or mildly off, but if you test too early, your results could come back negative even if your body is already infected. That false reassurance? It’s a dangerous kind of silence. It delays treatment, spreads infection to partners, and chips away at your confidence in knowing your body.
Let’s break it down. Chlamydia, one of the most common STDs, can sometimes be detected within a week, but the sweet spot for accuracy is 14 days or more. HIV testing is trickier: the rapid tests you can do at home or in clinics look for antibodies and antigens that don’t always show up right away. Most guidelines suggest testing again at the six-week mark to be sure. And herpes? That one’s the long game. Antibody-based tests often don’t show a positive result until four to six weeks after exposure, sometimes longer if your immune system’s slow to respond.
This doesn’t mean you need to test every weekend like you’re clocking in at work. But if you’ve had unprotected sex, changed partners, or felt something that just seems… off, it’s worth retesting. Even if the first test said negative. Even if your partner “swears they’re clean.” Even if it’s been months and you’re asymptomatic. Because that second test? That one might catch what the first one missed. That one might save you from needing more intense treatment, or from passing something on unknowingly.
Think of it like this: you wouldn’t check the locks once and assume your home is safe forever. You check them again when something changes. A new neighbor. A strange noise. A storm rolling in. Your body deserves that same attention. That same care. Testing again isn’t paranoia, it’s respect. For your health. For your peace of mind. For the next person you let in, emotionally or physically.
There’s no shame in checking twice. There’s only power in knowing, and acting before something small becomes something serious. You don’t need permission. You don’t need symptoms. You just need the will to prioritize yourself.
Confused? Here’s When to Retest (And Why)
Imagine this: You went on two dates with someone new. You used protection, but something still feels off, maybe a change in discharge or an odd pelvic twinge. You test negative at 10 days. Relief.
But three weeks later, your partner admits they’d just gotten out of another relationship too. Now what?
Here’s a simple decision timeline for retesting:
Figure 3. When to consider retesting after exposure or treatment.
Your Privacy, Your Power: Why At-Home Testing Works for Divorced Women
There’s something uniquely vulnerable about going back to your OB-GYN after divorce and saying: “I need an STD test.” But you shouldn’t have to justify it, or feel embarrassed.
At-home testing puts control back in your hands. You choose when, where, and what to test for. You don’t need to navigate work schedules, co-parenting calendars, or clinic wait times. Your results are yours alone.
Discreet packaging means no one at the mailbox, or inside your home, needs to know what you’re doing. And results come fast, so you're not stuck in limbo.
This is about reclaiming health on your own terms. Divorce changed a lot. Your sexual health should not be one more thing you lose control over.

People are also reading: I Thought I Got Tested for Everything, Turns Out I Didn’t
“I Thought STDs Were a Young Person Problem”
Vanessa, 50, had been monogamous her entire adult life. After divorcing her husband of 27 years, she felt “too old to worry about STDs” and assumed condoms weren’t necessary with someone she trusted. After six months of dating a new partner, she started experiencing lower abdominal cramps and occasional spotting.
“I thought it was menopause. But it felt weirdly… off. I asked my doctor if it could be an infection and she said it was probably just hormonal.”
It wasn’t. A routine pelvic exam during a Pap smear finally revealed an untreated case of gonorrhea that had caused early signs of pelvic inflammatory disease (PID).
“I couldn’t believe it. I never imagined this could happen to me. I didn’t even know gonorrhea could be silent.”
It can. And it often is, especially in women over 40, where symptoms can be subtle, mistaken for hormonal shifts, or ignored entirely.
STD testing isn’t about being reckless. It’s about being real.
How to Talk to Your Doctor (Even When They Don’t Ask)
If you're seeing a provider you trust, that’s great. But trust doesn’t mean silence. Here’s how to bring it up, without shame, apology, or awkwardness:
“I’ve recently started dating again and I’d like to be screened for STIs, can we include a full panel today?”
If they deflect or downplay your request, that’s a red flag. You can say:
“I understand the guidelines, but I’d feel more comfortable knowing. I’d really like to move forward with testing.”
Combo STD Test Kit covers the most common infections, and puts control back in your hands.
What If the Results Come Back Positive?
Take a breath. Positive results are scary, yes, but they are not the end. Most STDs are treatable, and all are manageable. What matters most is catching them early and notifying any recent partners.
If you test positive at home, follow-up options include:
- Scheduling a confirmatory test with a provider
- Accessing telehealth treatment pathways
- Getting antibiotics (if bacterial) or antiviral management (for viral STDs)
More importantly, it’s an opportunity to reset, your boundaries, your communication, your next steps. You are not dirty. You are not reckless. You are responsible for taking care of yourself, and that’s powerful.
FAQs
1. Do I really need an STD test if I’ve only had sex with one new person?
Yep. It only takes one. Even if it felt “safe,” even if it was someone you trusted. STDs don’t care about how many people you’ve been with, they care about whether exposure happened. Think of testing as a routine part of being sexually active again, not a judgment on your choices.
2. Why didn’t my doctor offer testing when I asked about discharge or itching?
Because a lot of providers assume midlife women aren’t at risk, or they blame symptoms on hormones, dryness, or menopause. Unless you specifically say, “I want a full STI panel,” it often gets missed. It’s not fair, but it happens constantly.
3. Is it weird to ask for an STD test if I don’t have any symptoms?
Not at all. Most STDs show zero symptoms for weeks or months, especially in women. That’s why testing without symptoms is actually the smart move, not the awkward one.
4. What’s the best time to test after sleeping with someone new?
Give it at least 10 to 14 days for most infections like chlamydia or gonorrhea. If you’re really worried, test once now and again at 6 weeks. That’s the most accurate strategy, and it keeps your peace of mind intact.
5. What if I’m using condoms, do I still need to test?
Condoms are great, but they're not perfect. Herpes and HPV are two STDs that can spread through skin contact, even if everything else is covered. Testing is about making sure you are fully covered, both emotionally and medically.
6. Can I really do this from home without a doctor?
Yes, you absolutely can. At-home tests are discreet, fast, and FDA-cleared. You collect a simple sample (swab, urine, or fingerstick), and results come straight to you. No judgment. No clinic chairs. Just answers.
7. Is it too late to test if I had unprotected sex months ago?
Nope. You can still test, and you absolutely should. Some infections, like syphilis or HIV, can hang out in your system quietly for a long time. Testing now could be the thing that keeps it from turning into something worse later.
8. What do I say to my doctor if they brush off my concern?
Try this: “I’d really feel better getting a full STI screening. I’ve had a new partner and I just want to be thorough.” If they still deflect? That’s not a “you” problem, it’s a provider problem. You deserve better care (and you can always go the at-home route).
9. Will anyone else see my results if I test at home?
Nope. Your results are yours. At-home kits ship in plain packaging, don’t show up on insurance, and don’t go in your medical record unless you choose to share them. Your body, your data, your timeline.
10. What happens if I test positive?
First: breathe. Most STDs are treatable. You’ll get a clear path forward, whether that’s antibiotics, follow-up care, or support resources. Testing positive isn’t a moral failure. It’s just a medical fact, and one you can take care of quickly when you know what you’re dealing with.
You Deserve Answers, Not Assumptions
Dating again after divorce isn’t just about opening your heart, it’s about protecting your health. But don’t wait for your doctor to raise the topic. Ask. Test. Take control.
You’re not irresponsible for wanting clarity. You’re empowered. Whether you’ve had one partner or five, whether it’s been five weeks or five years, your sexual health matters.
Order your at-home combo STD test kit today. It’s fast, private, and gives you back what silence never will: peace of mind.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources. Every external link in this article was checked to ensure it leads to a reputable destination and opens in a new tab, so you can verify claims without losing your place.
Sources
1. CDC Screening Recommendations for STIs – US Centers for Disease Control and Prevention
2. USPSTF Recommendation: Screening for Chlamydia & Gonorrhea (2021)
3. “Screening Recommended for Chlamydia, Gonorrhea” – AAFP Summary of USPSTF Update
4. Reproductive & Sexual Health Checklist for People in Their 40s – Hey Jane
5. Sexually Transmitted Infections in the Elderly Review | PMC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who focuses on preventing, diagnosing, and treating STIs. He combines clinical accuracy with a straightforward, sex-positive attitude and is dedicated to making his work available to more people in both cities and rural areas.
Reviewed by: Dr. L. Andrews, MPH | Last medically reviewed: September 2025
This article is for informational purposes and does not replace medical advice.