STD Window Periods: Why Testing Too Soon Can Give You a False Negative
Quick Answer: According to WHO’s latest surveillance data, drug-resistant gonorrhoea is spreading globally. At-home STD testing allows earlier detection, reduces transmission, and helps identify resistant strains sooner, especially when clinic access is limited or delayed.
Who This Guide Is For (And Why It Matters)
This guide is for you if you've ever been too embarrassed, scared, or unsure to get tested. You deserve to know what's going on with your body, whether you live in a small town with no sexual health clinic, are trying to figure out a situationship in a new city, or are just too scared to walk into a waiting room. Gonorrhea that doesn't respond to drugs doesn't care who you are. It affects straight couples, queer communities, travelers, sex workers, and anyone who is trying to be intimate without all the information.
Because resistance is rising all over the world, timing, testing, and getting the right results are more important than ever. The WHO's data may seem far away or like something that only scientists care about, but it really does affect your health, your relationships, and your ability to make smart choices. This article will explain what gonorrhea testing really means, when to get tested, how drug resistance affects treatment, and why home testing is such an important part of public health.

People are also reading: STI Rates Drop in 2024, But Newborn Syphilis Surges: What This Means for Home Testing
What Actually Counts as an STD Test?
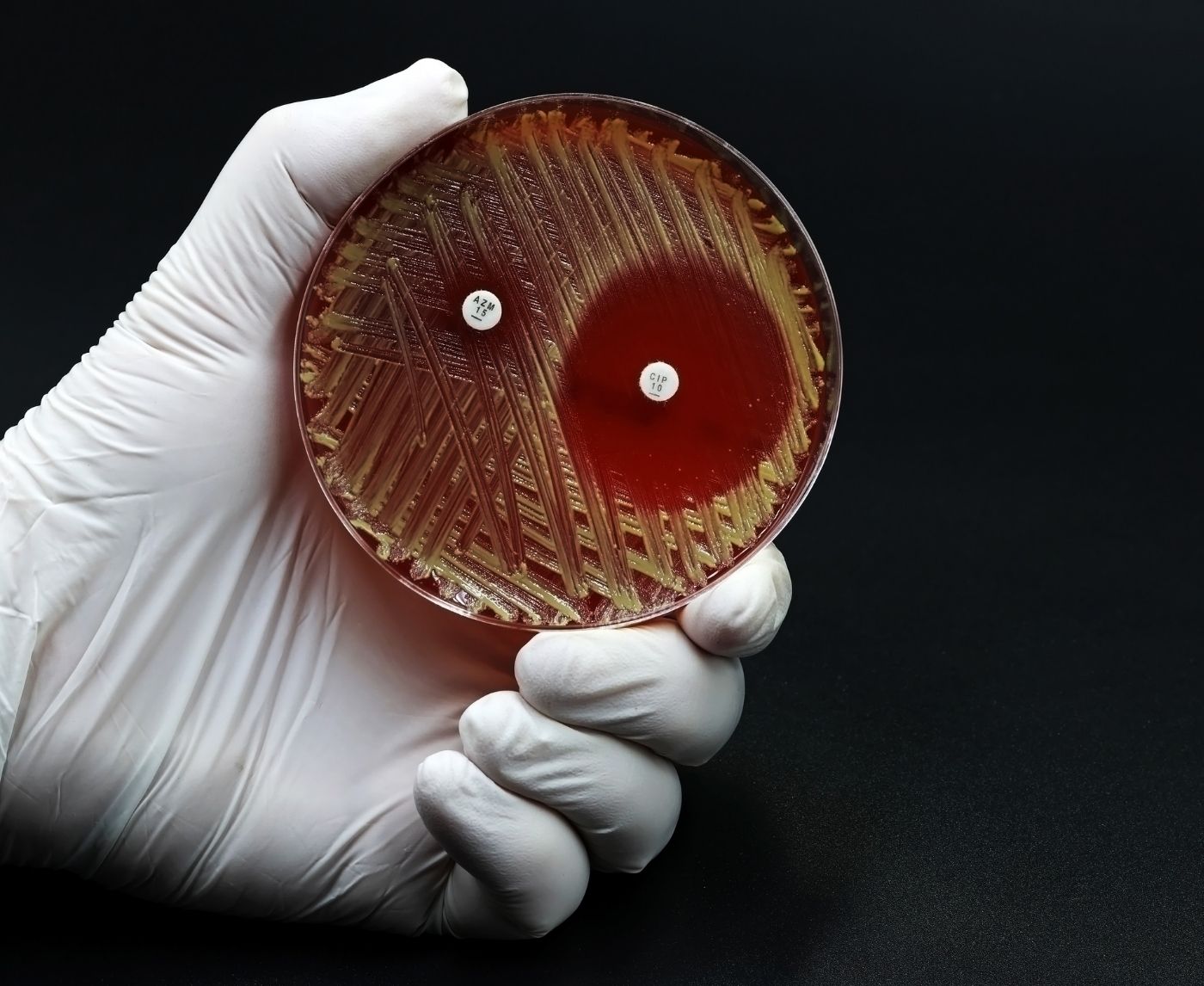
A real STD test for gonorrhea usually uses one of two technologies: the nucleic acid amplification test (NAAT), which looks for the bacteria's genetic material, or the rapid antigen test, which looks for certain proteins. NAAT is the best test because it is very sensitive, accurate, and is used in most clinical and mail-in lab settings. Rapid tests at home use lateral flow strips like those used in pregnancy tests and give results in about 15 minutes.
Sample types vary. Some tests require urine, others need a swab from the vagina, throat, or rectum. Blood tests are not typically used for gonorrhoea. According to the CDC's guidelines, choosing the right sample site depends on your sexual activity, not just symptoms. This matters because gonorrhoea can infect the throat or rectum with no noticeable signs at all.
At-home options now include both mail-in lab kits and rapid-result kits you use in your own bathroom. You can order discreet kits directly from STD Test Kits, no prescription, no waiting rooms. This Gonorrhoea Test Kit gives you control and clarity without delay.
Window Periods: What to Know for Each STD
Even the most accurate test depends on when you take it. The “window period” is the time between potential exposure and when a test can reliably detect infection. Testing too early can give false reassurance, especially when dealing with something as slippery as drug-resistant gonorrhoea. Symptoms, if they appear, often start within days. But even without symptoms, the bacteria may still spread and evolve into harder-to-treat forms.
Figure 1. Typical window periods and peak testing accuracy for common STDs. Testing earlier may miss infections and allow drug-resistant strains to spread unknowingly.
Rapid Test vs Lab Test: Pros, Cons, and Tradeoffs
Think about this: you're going on a long weekend trip with someone you've never met before. You don't have time for a clinic appointment, and you don't want to wait days for the lab results. That's when a quick test at home comes in handy. You get your result in 10 to 15 minutes, and you don't have to tell your provider or insurance company about it.
Now picture this: you had a high-risk encounter and need to be absolutely sure. You want the most sensitive test available, even if it means mailing a sample and waiting two or three days. That’s where mail-in lab kits shine. And if you’re already showing symptoms, or have had a treatment failure, a clinic NAAT is the gold standard for diagnosis and antibiotic guidance, especially as resistance rises.
Figure 2. Comparing STD testing methods by speed, privacy, and diagnostic strength. Each plays a role in containing drug-resistant gonorrhoea.
When to Test After Exposure
Let’s say you had a condom break two nights ago, or a partner you trusted just told you they tested positive for gonorrhoea. The urge to know right now is real, and understandable. But if you test too early, especially with a rapid test, the infection might not show up yet. Testing within 2 to 5 days of exposure may not catch it. That doesn’t mean you’re in the clear, it just means your body may not have built up enough of the infection to be detected.
If you’re between 7 and 13 days after exposure, testing becomes more reliable. This is the sweet spot for most gonorrhoea tests, especially NAATs and some rapid kits. Still, for peace of mind and peak accuracy, retesting after day 14 is ideal. That second test helps rule out false negatives and catch delayed infections, particularly critical now that antibiotic-resistant strains are becoming more common.
Case in point: A reader we’ll call Alex tested negative five days after a risky hookup in a new city. But symptoms showed up ten days later, burning urination, discharge, a sharp ache in his groin. A clinic NAAT confirmed a gonorrhoea infection, and follow-up resistance testing showed it was non-responsive to ciprofloxacin. If Alex hadn’t retested, he might’ve unknowingly exposed another partner, or been given the wrong antibiotics.
If you’re unsure when to test, or you just want to rule things out without judgment, this discreet at-home combo test kit gives you answers on your timeline. Whether it’s for prevention, confirmation, or follow-up, timing matters, and so does action.
Do You Need to Retest? Here’s How to Know
If you’ve already been treated for gonorrhoea, or thought you had it under control, retesting might feel redundant. But here’s the deal: drug-resistant strains are rewriting the rules. A single round of antibiotics that worked last year might not work this year. WHO’s report shows growing resistance to cefixime, ceftriaxone, and even older meds like azithromycin. In other words, what once counted as “treated” may now require a second check.
Let’s look at retest windows:
If you were treated in a clinic, retest at 14 to 30 days post-treatment to confirm clearance. If you self-tested and treated without confirmation, wait 30 to 45 days and retest, especially if you didn’t get symptoms in the first place. If you keep having new partners or any high-risk exposures, monthly testing may be the most responsible path forward.
Marisol, 32, got treated for gonorrhoea in early 2024 while backpacking through Southeast Asia. She took a single dose of cefixime, but her symptoms didn’t fully go away. When she returned home weeks later, a second test showed persistent infection, this time resistant to two first-line drugs. It wasn’t until she saw an infectious disease specialist that her treatment plan finally worked. Her takeaway? Always confirm the infection is gone. Never assume one dose is enough.
Privacy, Shipping, and Discreet Support
Waiting in a clinic, making awkward phone calls, or hoping the pharmacist doesn’t judge you, these used to be part of the STD testing process. Not anymore. With the rise of discreet at-home kits, you don’t need to broadcast your concern to the world just to get checked. Gonorrhoea may be getting bolder, but your right to privacy hasn’t changed.
When you order a test from a site like STD Test Kits, the packaging is plain and it gets to you quickly. Most kits get shipped out within one business day and come in plain boxes or envelopes with no logos or red flags. This makes it easier for people who share a home with roommates, family, or other people to take care of their health without drawing attention to themselves.
You can also choose the pace and process that works best for you because there are both quick tests and mail-in kits. Are you going on a trip? Bring a quick test with you just in case. Taking a break from a long-distance relationship? Before reconnecting, get tested. Living off the grid? That's fine. Just send your sample when you get back to town. Support doesn't stop after the test, though. If you're not sure what to do next, you can find online guides, tools for interpreting results, and customer service.
What If You Test Positive?
Let’s get this straight: a positive test isn’t the end of the world. It’s the beginning of a plan. And with resistant strains on the rise, knowing you’re positive gives you a crucial head start in finding the right treatment and stopping the spread.
The WHO report shows rising resistance to the most common antibiotics, especially ciprofloxacin (up to 95% resistance in some regions). If you test positive, confirm it with a clinical NAAT or a follow-up test through a licensed telehealth service. That way, a doctor can guide your treatment and, if needed, run resistance profiling. You may not need a whole team, just the right next step.
Consider this moment: Jordan, 26, tested positive on an at-home kit after a recent trip. Instead of spiraling, he used a telehealth service to get a same-day prescription. When symptoms didn’t fully clear, he returned for follow-up and was switched to a different antibiotic. The final test? Clean. And his partner? Tested and treated, too. Transparency, not panic, made all the difference.
If you test positive, take a breath. Then take the next step. Partner notification can be handled anonymously in many regions, and treatment is still available, even for resistant strains. But you can’t start until you know.
People are also reading: What the GLASS Tables Actually Mean for Your STD Risk
Why Surveillance Programs Matter (And Why You’ve Never Heard of EGASP)
Most people don’t realize there’s a global system tracking antibiotic-resistant gonorrhoea. It’s called EGASP, the Enhanced Gonococcal Antimicrobial Surveillance Programme, and it’s run by WHO. That’s the same program behind the latest data showing rising resistance rates in countries like Cambodia, Viet Nam, and India. EGASP quietly collects samples from patients around the world, tests them in labs, and watches for patterns in which antibiotics are failing.
Think of it as a giant early warning system. When resistance to a drug hits a tipping point, EGASP alerts clinicians and governments so treatment guidelines can be updated. Without it, many doctors would still be prescribing antibiotics that no longer work. And if you’re wondering how this connects to you: the strain of gonorrhoea you carry, or the one you could catch next, might already be part of this global trend. Testing, especially at scale, feeds the data pipeline that helps stop the spread of super strains.
In 2024, only 12 countries submitted full data to EGASP, and gaps remain, especially for women and people with rectal or throat infections. But expansion is underway, and your individual test could one day be part of the solution. Especially if you use a test provider that collaborates with public health bodies or supports anonymized tracking.
Where Resistance Is Spreading Fastest
Not all resistance rates are the same across the globe. In fact, some countries are now considered “hot zones” for drug-resistant gonorrhoea. If you’ve traveled recently, or hooked up with someone who has, it’s worth understanding the map before you dismiss your symptoms or skip testing altogether.
Figure 3. Selected countries reporting elevated levels of drug-resistant gonorrhoea. Rates are from WHO EGASP 2024 data.
Why does this matter? Because someone can bring a resistant strain home without knowing they’re carrying it. And you can catch it during what feels like a low-risk hookup. Resistance doesn’t always mean severity, but it does mean standard treatment might not work. The only way to stay ahead is to test, know your results, and share them, safely, with any partners who need to know.
The DoxyPEP Debate: Prevention or Pandora’s Box?
If you’ve heard of DoxyPEP, doxycycline taken after sex to prevent STIs, you’re not alone. It’s been making headlines as a possible tool for high-risk groups, especially men who have sex with men. But when it comes to gonorrhoea, the science is messy and the risks are real.
Early studies showed promise, suggesting that DoxyPEP could reduce bacterial STIs, including gonorrhoea. But WHO and other experts are now urging caution. That’s because overuse of doxycycline could drive even more resistance, making the very bacteria we’re trying to prevent even harder to treat. In fact, resistance to tetracyclines (the class that includes doxycycline) is already widespread in gonorrhoea strains worldwide.
Clinical trials are ongoing, and guidelines are evolving. But here’s what’s clear: DoxyPEP is not a replacement for testing. It’s not for casual use. And if used wrong, it could make the resistance problem worse. If your partner is on DoxyPEP or you’ve considered it yourself, make sure you’re also testing regularly, especially after high-risk encounters. And consider using tests that target multiple STIs, not just one.
What the Future Looks Like, and Why Testing Still Wins
WHO is putting money into new treatments like zoliflodacin and gepotidacin, which are two experimental drugs that are meant to fight gonorrhea that doesn't respond to other drugs. They are still in the testing phase, but the first results are good. At the same time, genomics-based surveillance is being expanded, with almost 3,000 bacterial samples sequenced in 2024 to help scientists learn more about how resistance spreads and changes.
That’s the big picture. But on the personal level, what matters most is action. Test early. Test again if symptoms change. Don’t assume a one-night stand is too “casual” to matter. And don’t count on antibiotics to fix what you haven’t confirmed. Testing is care. Testing is power. And at-home options make it easier than ever to take that step, whether you’re traveling, closeted, uninsured, or just not ready to talk to a doctor.
If you’re still wondering whether it’s “worth it,” this is your sign. Order a discreet combo STD kit today, and find out what your body’s been trying to tell you.
FAQs
1. Can drug-resistant gonorrhoea go away on its own?
It won’t. Even if the symptoms fade or vanish, the bacteria can keep spreading under the radar, sometimes into your bloodstream, joints, or reproductive organs. We’ve heard people say, “I felt better after a week, so I assumed it cleared.” It didn’t. If it’s resistant, it’s not just stubborn, it’s dangerous. Get tested. Get treated right.
2. How serious is antibiotic resistance in gonorrhoea?
Picture this: the main drug we’ve relied on for years, ceftriaxone, is now failing in up to 1 in 20 cases globally. That might sound small, but in some countries it’s much worse. Ciprofloxacin? Basically useless now in most regions. We’re not in panic mode, but we’re past the “ignore it and hope” phase. Testing early gives doctors options before resistance shuts the door.
3. I tested negative, but I still feel off. What gives?
You might’ve tested too early. The bacteria needs time to build up to detectable levels, especially in rapid tests. Or you may have another infection entirely (hello, chlamydia, trichomoniasis, or even a UTI). If your gut says something’s wrong, listen to it. Retest. Consider a combo kit. Better to be annoyingly cautious than unknowingly contagious.
4. Does at-home testing catch throat or butt infections?
Most over-the-counter kits are made for urine or genital swabs. But gonorrhoea is an overachiever, it loves the throat and rectum, especially in people having oral or anal sex. If you’ve gone there (no shame), talk to a provider or use a kit that supports extra swab sites. Silent throat infections are one of the biggest drivers of resistance, and they’re sneaky.
5. There was a faint line on my rapid test. Is that a positive?
Probably, yes. Faint doesn’t mean fake, it could mean you caught the infection early, which is actually a win. Read the kit instructions like your health depends on it (because it kinda does). And if you’re unsure, retest or go the lab route. No shame in a second opinion when the stakes are this high.
6. How do I bring up testing with someone I just started seeing?
Try this: “Hey, I just took a test because I want us both to feel safe. Want to do it together?” Make it a care move, not an accusation. Trust us, confidence is hot, and health literacy is sexier than any pickup line. If they push back, that’s your red flag, not a green light.
7. I got treated, but the symptoms came back. Am I reinfected?
Maybe. Or maybe the strain wasn’t fully knocked out, especially if it’s resistant. One round of antibiotics doesn’t always do the trick anymore. This is why follow-up testing matters. Don’t just Google and guess. Get checked again. You’re not “being dramatic”, you’re being smart.
8. Is this only a problem for gay men or people with lots of partners?
Not even close. While resistance trends are high in certain groups, we’ve seen cases in married folks, teens, travelers, and people who swear they’re “low risk.” Gonorrhoea doesn’t care who you are, it only needs one window. If you’re sexually active, this affects you.
9. I had a hookup abroad. Should I be worried?
Depends where, and depends what you did. WHO flagged countries like Viet Nam, Cambodia, and the Philippines as hotspots for resistant strains. If you had unprotected sex or symptoms popped up after travel, test. Don’t wait for guilt to kick in. This isn’t about judgment, it’s about getting ahead of something that spreads fast and hits harder when ignored.
10. Is there any way to prevent drug-resistant gonorrhoea?
You can’t prevent the bacteria from evolving, but you can stop it from spreading. Test regularly. Use protection. Don’t hoard or misuse antibiotics. And if you do test positive, tell your partners. Quiet infections breed tough bacteria, and testing breaks the chain. One swab can stop a dozen future cases. That’s power.
Before You Panic, Here’s What to Do Next
Super strains sound scary. Headlines don’t always tell the full story. But here’s what matters: gonorrhoea is still treatable, especially when caught early. The more we test, the more we know. And the faster we adapt, the better we protect each other.
If something feels off, or even if it doesn’t, don’t wait. Drug-resistant STDs don’t always shout. Sometimes, they whisper. And that whisper could be your only warning. This discreet combo test kit checks for the most common STDs quickly and privately, so you don’t have to second-guess your status.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. More Countries Report Rising Levels of Drug-Resistant Gonorrhoea – WHO (2025)
2. Drug‑Resistant Gonorrhea — CDC
3. Gonorrhoea (Neisseria gonorrhoeae infection) — WHO Fact Sheet
4. Update to CDC’s Treatment Guidelines for Gonococcal Infections — MMWR 2020
5. Management of Neisseria gonorrhoeae in the United States — Clinical Microbiology Review 2022
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: L. Jennings, MPH | Last medically reviewed: November 2025
This article is for informational purposes and does not replace medical advice.