How Long Can Chlamydia Stay in Your Body Without Symptoms?
Quick Answer: Partner notification after an STD diagnosis prevents repeat infections by ensuring both people get treated. Without it, one partner’s untreated infection can silently re-infect the other, creating a cycle of risk.
Why Repeat Infections Happen More Often Than You Think
A lot of people think that the problem is over once they take antibiotics or finish treatment. In reality, the infection is still there if a partner never gets treated. It just comes back after having sex without protection. This isn't uncommon, according to public health data. The CDC says that getting chlamydia again is common, especially in young adults. They think that 10 to 20 percent of people who get treated will get it again within the first year. Gonorrhea behaves in a similar way, with high rates of recurrence when partners don't get treatment. These aren't just numbers; they're real people stuck in a frustrating loop that feels like déjà vu in a doctor's office.
Picture a young couple in their twenties. One partner gets treated for gonorrhea but never has the conversation. They reunite, convinced the storm has passed. A few weeks later, symptoms flare again: burning urination, unusual discharge, confusion about why antibiotics “didn’t work.” The truth is the medication did its job, once. Reinfection from an untreated partner restarted the process. This cycle can last for months if no one interrupts it with honesty.

People are also reading: Think It’s Just a Skin Thing? Syphilis Rashes Are Trickier Than You Think
Symptoms That Pull People Back to the Clinic
Reinfection doesn’t always look different from the first round. Burning, discharge, testicular pain, pelvic cramps, the same distressing signs appear again, leaving patients convinced their treatment failed. Some shrug it off as “a stubborn bug,” while others fear antibiotic resistance. In reality, the problem is often more ordinary: one partner never got treated in the first place. For men, repeated bouts of gonorrhea or chlamydia increase the risk of epididymitis and possible infertility. For women, repeat infections raise the risk of pelvic inflammatory disease, a condition that can scar the fallopian tubes and make pregnancy difficult. The symptoms may fade with each new round of antibiotics, but the underlying damage accumulates silently.
One woman, interviewed in a fertility clinic, described her regret: “We just kept passing it back and forth. I thought the cramps were just bad periods. By the time we figured it out, my tubes were scarred.” Her story is a reminder that the body doesn’t forgive endless cycles. Partner notification isn’t just about courtesy, it is a medical intervention that changes long-term outcomes.
The Science of Reinfection
To understand why partner notification matters, it helps to see how reinfection works at the cellular level. Antibiotics clear bacteria like chlamydia trachomatis or neisseria gonorrhoeae from the body. But if a partner remains untreated, the bacteria survive in their system. When sexual contact resumes, the bacteria find a new host all over again. Reinfections aren’t weaker or milder; they carry the same risks and sometimes hit harder because the immune system is already inflamed.
Medical research substantiates that each reinfection increases the likelihood of complications. One untreated case of chlamydia may not cause visible scars, but getting it again and again makes you twice or three times more likely to be infertile. Reinfection is a big reason why gonorrhea bacteria become resistant to antibiotics. This is because the bacteria keep coming into contact with the drugs and develop ways to protect themselves. This means that silence isn't just bad for one couple; it also makes public health problems worse.
Table 1. Reinfection rates and risks for common STDs, highlighting why partner notification is essential to break the cycle.
Case Study: The Relapse No One Explained
Nia, 26, had been treated for chlamydia twice in the same year. Each time, the antibiotics worked, but the infection returned. She remembers crying in her car after the second diagnosis:
“I thought something was wrong with me. The doctor finally asked if my boyfriend had been treated too. That’s when I realized he hadn’t even been tested.”
Once both partners were treated together, the infections stopped. Her story mirrors thousands of similar cases where reinfection wasn’t a failure of medicine but a failure of communication.
The Stigma That Keeps People Quiet
If reinfection is so common, why don’t people just tell their partners? The answer lies in shame. Many describe feeling dirty, guilty, or terrified of being judged. That silence comes at a cost. A man in his thirties admitted, “I was more afraid of her reaction than of the infection itself.” He never disclosed his diagnosis, and months later, his partner tested positive for the same STD. Both ended up in a loop of treatment, confusion, and anger that could have been avoided with one awkward but lifesaving conversation.
Stigma works like a lock on the truth. It convinces people that silence will preserve dignity, when in reality it protects the infection. Public health campaigns stress that testing and disclosure are not admissions of recklessness, they are acts of care. Until this reframing becomes cultural norm, reinfection will remain a hidden epidemic fueled not by biology alone, but by fear of rejection.
What Happens When Only One Partner Gets Treated
Medical charts reveal a simple pattern: solo treatment is almost always followed by recurrence. Treating one partner without addressing the other is like patching one side of a leaking boat. You can bail water for a while, but the flooding never stops. Doctors and clinics constantly emphasize this: both partners must be treated, ideally at the same time, to close the reinfection loop.
Consider James, 24, who went to urgent care after noticing painful urination. He was given antibiotics for gonorrhea and left thinking the ordeal was over. Two months later, the same symptoms returned. The nurse asked, “Did your girlfriend get treated?” His silence said everything. By failing to include his partner, James had unknowingly invited the bacteria back. For him, the lesson was brutal but unforgettable: STD treatment is never a solo mission.
The Data Behind Partner Notification Programs
Public health organizations have tried a lot of different ways to get people to tell their partners, such as making direct phone calls and using anonymous text services. It's clear from the evidence that partner notification works. A review by the World Health Organization found that when clinics gave patients tools to tell their partners, the number of people who got reinfected went down a lot. Even simple things, like giving patients a list of partner treatment prescriptions, cut the number of relapses by almost half. It shows that antibiotics aren't the only thing that affects how infections turn out.
Anonymous notification services add an extra level of safety. They let someone send a message without giving away who they are, which lowers fear while making sure partners know to test. Research from urban clinics in the U.S. and U.K. shows that these tools help partners get treatment more often, which stops cycles that would otherwise last for months. The lesson is clear: when systems make it easier to share information, rates of reinfection go down.
Table 2. Effectiveness of different partner notification methods in lowering reinfection rates.
Case Study: The Text That Saved a Relationship
Lina, 21, panicked when she saw the words “positive for chlamydia” on her clinic report. For hours she rehearsed how to tell her boyfriend. Finally, she used an anonymous notification service that sent him a text. The next day he messaged her with relief, not anger:
“Thanks for letting me know. I’ll get treated too.”
They both completed antibiotics and later reflected that the honesty strengthened their trust. What started as fear ended as proof that communication could heal more than the infection.
Why Partner Notification Protects More Than Just Two People
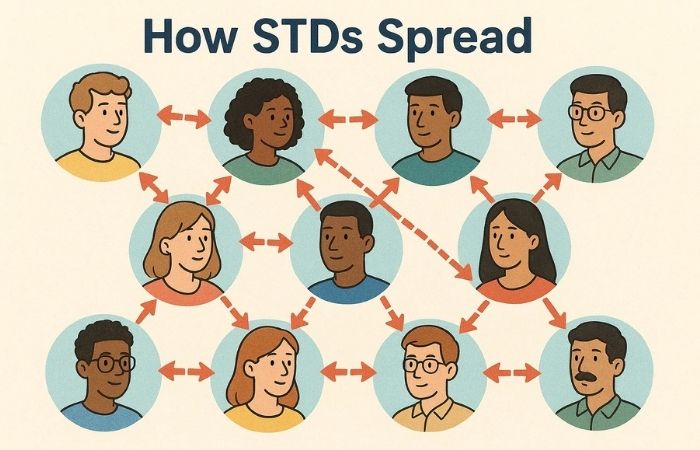
Every STD transmission is part of a chain. Failing to notify a partner doesn’t just risk your own reinfection, it risks spreading infection further into the community. Epidemiologists compare it to dominoes: one untreated case can topple into many. Reinfections keep bacteria circulating, giving them more opportunities to evolve resistance to treatment. Partner notification, then, isn’t just personal. It’s a public health defense against drug-resistant strains of gonorrhea and persistent waves of chlamydia.
The responsibility can feel heavy, but reframing it as protection shifts the weight. Telling a partner is not only about preventing awkward symptoms next month, it’s about contributing to a healthier sexual network for everyone. Silence leaves cracks where infections grow stronger. Words, though difficult, close those cracks.
People are also reading: What Syphilis Looks Like in Newborns (And Why It’s Often Missed)
Breaking the Cycle With Joint Treatment
The most effective way to prevent repeat infections is simple: both partners get treated at the same time. Doctors call this “expedited partner therapy” when a patient leaves the clinic with medication for their partner as well. It skips the delay of waiting for the other person to make an appointment, which is often where reinfections creep in. This approach may feel transactional, but in practice it’s lifesaving. It treats the relationship as one unit of care rather than two individuals pretending their health is separate.
Caleb, 27, described the moment he handed his girlfriend the second prescription:
“It was awkward, but we both laughed and took our pills together at the kitchen table. It felt like teamwork instead of blame.”
That shift in perspective is the power of partner notification, turning what could be a wedge into an act of mutual protection.
Sex Positivity as a Prevention Tool
Shame feeds silence, but framing sex in a positive way breaks it down. Instead of seeing an STD as proof of bad decisions, it sees getting one as a normal part of sexual activity. Testing is like brushing your teeth or getting a flu shot; it's part of keeping up with things. Partner notification changes from a way to confess to a way to show you care. When couples talk about their problems without judging each other, reinfection stops happening.
This change in thinking is important for younger adults who are starting new relationships and for older couples who are trying to be intimate again. Public health campaigns that focus on empowerment rather than guilt consistently achieve elevated rates of disclosure. It's not just semantics to say "protect your partner" instead of "admit your mistake." It's the difference between doing something and not doing anything.
Data on Reinfection and Fertility
Reinfection is far worse than being forced to have awkward conversations and go back to the clinic. Women infected with chlamydia more than once are between three and four times at risk of getting pelvic inflammatory disease, researchers have established. Men infected with gonorrhea more than once have a high risk of getting epididymitis, which ruins sperm transport. Reinfections are not merely annoyances, but they build up and are long-term threats to reproductive health.
Clinic data bears this out. One study, which concluded in 2022, determined that 11% of female causes of infertility under 30 were a result of untreated chlamydia or gonorrhea more than once. In males, repeat infections leading to scarring were responsible for about 7% of obstructive infertility cases. These percentages demonstrate what happens when there is no partnership notification: not merely temporary woe, but futures altered throughsilence.
Table 3. How repeated reinfections raise fertility risks in men and women, showing why disclosure is more than a conversation, it’s prevention.
Case Study: The Relationship That Almost Ended
Kendra, 30, tested positive for trichomoniasis and felt torn about telling her new partner. She delayed the conversation for weeks, terrified he’d think less of her. By the time she told him, he had already reinfected her.
“We almost broke up over it,” she recalled. “I thought he’d blame me, but he was just frustrated that we hadn’t solved it together.”
After simultaneous treatment, the infections stopped, and so did the tension. Their story shows how delayed disclosure can harm both health and relationships, while openness often repairs both.
Shifting From Blame to Prevention
At its core, partner notification is about shifting the narrative. Instead of focusing on who brought the infection into the relationship, it focuses on how to stop it from staying there. This shift turns fear into action. It empowers both partners to see treatment as a shared investment in their health and their future. Blame fuels silence, and silence fuels reinfection. Prevention thrives on honesty, and honesty thrives on compassion.
The cycle of repeat infections isn’t inevitable. It breaks the moment someone decides their health, and their partner’s, is worth more than their fear. That decision transforms one of the most uncomfortable conversations into one of the most powerful tools in sexual health.
FAQs
1. Why should I tell my partner if I already took the medicine?
Because you’re not sleeping with bacteria in a vacuum. If your partner never gets treated, the infection is just waiting to crawl back into your life the next time you hook up. It’s like cleaning half a kitchen and then wondering why the ants keep coming back.
2. What if they flip out when I tell them?
Some people do get defensive. Others surprise you by saying, “Thanks for being straight with me.” One guy told me he dreaded telling his girlfriend, only to hear her say she was relieved he’d taken it seriously. Honesty might sting for a minute, but it beats the weeks of burning pee that come with reinfection.
3. Can I really get the same STD twice?
Over and over again, yes. Chlamydia and gonorrhea don’t hand out immunity badges. Think of it like catching the same cold from the same roommate who never covers their mouth. Until both of you deal with it, it just keeps circling back.
4. Do I have to sit down face-to-face to tell them?
Nope. If talking makes your stomach turn, you’ve got options. Clinics and online services let you send anonymous texts or emails that basically say, “Someone you slept with tested positive, get checked.” It’s not Shakespeare, but it gets the job done and protects you both.
5. How soon should I tell them?
Waiting never makes it easier. I’ve heard people stall for weeks, hoping symptoms disappear or courage magically arrives. Meanwhile the infection just keeps working. A blunt text tonight saves you both the hassle of antibiotics next month.
6. Does partner notification actually save fertility?
Yes. Each reinfection piles on damage your body doesn’t fully repair. Women risk scarring in their fallopian tubes; men risk epididymitis that can block sperm. Protecting your ability to have kids someday can literally come down to sending a message today.
7. What if my symptoms already went away, doesn’t that mean I’m fine?
Not at all. Symptoms fading usually just means the antibiotics are doing their thing. If your partner hasn’t been treated, they can hand it right back to you. Feeling “better” doesn’t mean the cycle is broken.
8. What if my partner refuses to get tested or treated?
Then you’ve got a bigger decision than just health, you’ve got a trust problem. If they won’t take steps to protect both of you, continuing sex with them means volunteering for round two (or three, or four). Boundaries aren’t just emotional here; they’re medical survival strategies.
9. Can I get reinfected even if we used condoms?
Condoms cut the risk way down, but they’re not a magic shield. If your partner still has the infection, there are ways it can slip past, especially with oral sex or skin-to-skin contact outside the condom zone. Condoms plus partner treatment is the real winning combo.
10. What if I don’t know how to start the conversation?
Keep it simple. You don’t need a speech. Something as short as, “I tested positive and you should get checked,” works. One woman told me she literally read the clinic’s info sheet out loud to her boyfriend because she froze up. Awkward? Yes. Effective? Absolutely.
Why Telling Protects More Than You
Reinfections are rarely about bad medicine, they’re about missed conversations. Partner notification is uncomfortable, yes, but it turns one diagnosis into the end of a problem instead of the beginning of a cycle. It protects your body, your partner’s health, and sometimes even your ability to have kids in the future. It also chips away at the stigma that keeps so many people quiet. When honesty becomes normal, reinfections become rare.
If you’ve been diagnosed, don’t leave your health hanging in silence. A discreet at-home STD combo test kit can help you and your partner take the next step together. Testing side by side isn’t awkward, it’s partnership in action.
How We Sourced This: Around fifteen authoritative sources informed this article, including guidance from the CDC, WHO, and peer-reviewed journals. We also drew on patient narratives and clinic studies about reinfection patterns to make the science relatable. Below we highlight six of the most relevant and reader-friendly sources that shaped our reporting.
Sources
1. WHO – Sexually Transmitted Infections Fact Sheet
2. Mayo Clinic – Gonorrhea Overview
3. Planned Parenthood – Chlamydia Overview
4. Partner notification , A systematic review | PMC
5. Partner notification for sexually transmitted infections in developing countries | BMC Public Health
6. Digital Interventions for STI and HIV Partner Notification | BMJ STI
About the Author
Dr. F. David, MD is a board-certified specialist in communicable diseases with a special interest in STI treatment, prevention, and diagnosis. He approaches medicine with medical rigor tempered by a no-nonsense, sex-positive outlook, and is committed to putting the book out there for people both on- and off-the-grid.
Reviewed by: Dr. R. Lopez, MPH | Last medically reviewed: September 2025
This article is for informational purposes and does not replace medical advice.







