The Most Common STDs People Don’t Realize They Have
Quick Answer: In men, STDs often show up as visible discharge, pain while peeing, or genital sores, but many are completely silent. Even without symptoms, you can still pass the infection to partners and risk long-term health effects if left untreated. Testing is the only way to be sure.
Not All Symptoms Scream: What STDs Look Like in Men
If you have a penis, the common belief is that you’ll “know” if you have an STD. Burning when you pee? Obvious. Discharge? Clear signal. But many men experience little or no symptoms, especially with viral STDs like HPV or early-stage syphilis. Others confuse signs with irritation from new lube, friction burns, or even ingrown hairs.
Scene snapshot: Devon, 32, thought the red bump near his shaft was a razor nick. It didn’t hurt, didn’t spread, and disappeared in a few days. Three months later, after his girlfriend tested positive for herpes, he realized that bump had been a primary outbreak.
Here are the most common STDs and how they tend to manifest in men:
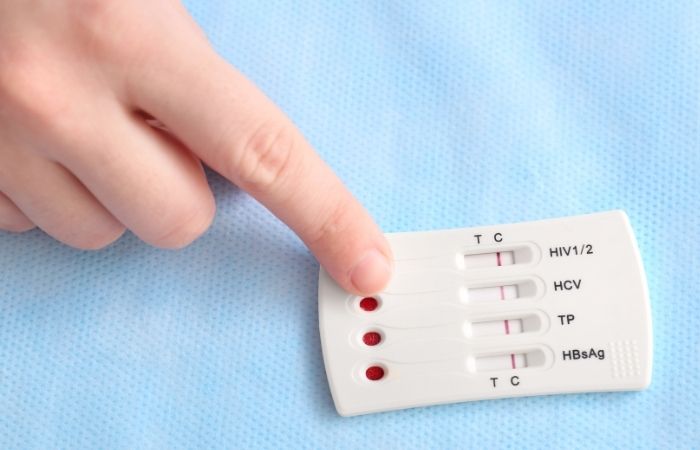
Figure 1. How common STDs show, or don’t, in men.
Even when symptoms do appear, they might be so mild you brush them off. That’s why STDs don’t just spread through recklessness. They spread through false reassurance.
The Early Warning Signs Men Often Miss
STD symptoms don’t always hit like a freight train. Sometimes they show up as a whisper, easily misread, easily ignored. These early symptoms are red flags men often dismiss until the infection has already progressed:
- Mild discomfort when urinating (often blamed on dehydration or a rough night out)
- Tingling or itching in or around the genitals without visible sores
- Single red bump or ulcer that doesn’t hurt
- Cloudy or off-smelling urine
- Stinging during ejaculation
Case example: Omar, 24, had slight tingling and dry skin near his foreskin but no pain. He assumed it was a detergent reaction. Six weeks later, after his ex reached out about a positive chlamydia test, he got tested, his was positive too.
Bottom line? If something feels off, even if it’s minor, don't wait to test. Many male infections are silent or subtle, and by the time symptoms become obvious, complications may have already started.
You can check your status at home with a Combo STD Test Kit. It’s discreet, fast, and helps you catch what your body might be hiding.
Why Timing Screws Men Over: Symptoms vs Incubation
Let’s say you had a sketchy hookup last weekend. You’re freaking out, Googling symptoms on day three, wondering if that mild stinging is something or nothing. Here’s the thing: most STDs don’t show up right away. There’s a lag between exposure, infection, and symptoms, and it’s not the same for every STD.
Even worse? Some infections never show symptoms at all. That’s where timing messes with your head, and your test results.
Figure 2. Common STD incubation vs symptom and testing windows in men.
This table shows why testing “just to be safe” a day after sex doesn’t help. You might test negative simply because it’s too soon, even if you’re infected. That’s called a false negative, and it gives you false confidence. The best strategy? Wait for the ideal window, or plan for a retest later if you test early.
It’s Not Always About Penetration: How Men Catch STDs Without Realizing
One of the biggest myths out there is that if you didn’t “go all the way,” you’re in the clear. Not true. STDs don’t care about what you call sex. If there was skin contact, fluid exchange, or oral activity, you’re at risk.
Common overlooked scenarios:
- Receiving oral sex – Can transmit gonorrhea, herpes, syphilis, and even chlamydia
- Rubbing genitals (“dry humping” skin-to-skin) – Can transmit HPV or herpes
- Sharing toys or lube – Especially with improper cleaning
- Anal play – Without proper barrier protection or testing
Alex, 21, caught oral gonorrhea from receiving unprotected oral sex at a party. He didn’t have any symptoms, but the infection was later picked up on a throat swab after his regular test came back negative.
Testing sites often overlook non-genital exposure unless you ask. If you're engaging in oral or anal play, ask for extragenital testing, or choose a home kit that includes throat or rectal swabs where appropriate.
Masculinity, Silence, and Why Men Wait Too Long
Let’s talk about ego. Shame. That quiet fear that going to get tested makes you look weak, irresponsible, or “like you’ve done something wrong.” These ideas keep men from acting, even when their bodies are waving red flags.
Data check: According to the CDC, men, especially straight-identifying men, are significantly less likely to get regular STD testing unless symptomatic. And even then, many wait weeks to see a provider.
Why?
- Fear of judgment from partners or doctors
- Assumption that “no symptoms = no problem”
- Belief that STDs only happen to “other kinds of guys”
We get it. But here’s the truth: getting tested isn’t weakness. It’s leadership. It's protection. It’s ownership. And it's how you protect the people you sleep with, no matter how casual or committed the connection.
If walking into a clinic feels impossible, use an at-home STD test kit. Same accuracy. No side-eye. Full control.
People are also reading: The Most Dangerous Sex Act for STDs (And How to Stay Safe)
What Happens If You Don’t Treat It?
Let’s be blunt: untreated STDs don’t just “go away.” And in men, the consequences are real, especially if you assume silence means safety. Some complications show up fast, others take years. All of them can wreck your health.
Figure 3. What STDs do in male bodies if you delay or skip treatment.
Here’s the twist: even if you feel fine now, damage may be happening under the surface. That’s especially true for infections in the urethra, testicles, and prostate, areas where pain is easy to miss or mask. And if you’re sexually active with more than one partner, that untreated STD isn’t just your problem. It becomes theirs too.
Think of testing as damage control. The earlier you know, the easier it is to fix. You don’t need to be perfect, you just need to be proactive.
What It Looks Like on Skin: Why STDs Are Misdiagnosed in Men
Most guys look for red flags like “STD rash” or “genital sores” on Google Images, but that’s where things get tricky. Skin-based symptoms like herpes, syphilis, or even HPV can show up differently based on your skin tone, hair type, and where the outbreak happens.
Figure 4. Why STD symptoms on skin may look different depending on skin tone.
This matters. Because if you’re only looking for what shows up on pale skin, or waiting for something dramatic, you may overlook signs on your own body. Even providers sometimes miss these cues, especially for Black, brown, and Indigenous patients. Knowing what to look for, and where to look, is key.
Here’s a tip: don’t just check the tip. Look along the shaft, under the foreskin (if applicable), around the base, testicles, and even the perineum (space between testicles and anus). Use a mirror, a flashlight, whatever it takes. Or better: use a test kit to get real answers, not guesses.
“I Waited Too Long” , One Guy’s Turning Point
This section includes fictionalized perspectives meant for educational illustration. They are not direct patient accounts.
Darren, 29, had a history of casual flings but never really worried about STDs. He used condoms “most of the time” and figured that was enough. One month, he noticed a bit of discharge, chalked it up to friction. Then came the groin pain. When he finally tested (six weeks later), he was positive for both chlamydia and gonorrhea. He also had mild epididymitis, inflammation of the testicle tubes. He recovered, but his doctor warned that future fertility could be affected.
“I wasn’t scared of STDs,” Darren said. “I was scared of knowing. That was my biggest mistake.”
It’s a story we’ve heard before. Not because men don’t care, but because they were never taught to take this seriously unless something felt broken. But infections don’t always break you right away. They chip away quietly. Until one day, they don’t.
Reinfection, Retesting, and Moving Forward
Let’s say you got tested. You got treated. You’re in the clear. Now what?
The reality is: many STDs come back. Not because treatment didn’t work, but because one partner didn’t get treated, or you jumped back into sex too soon. That’s called reinfection, and it’s extremely common in male-female and male-male partnerships alike.
Here’s how to stay ahead:
- Wait 7 full days after finishing treatment before any sexual activity
- Make sure partners are treated at the same time
- Retest 3 months later to confirm clearance
- Use protection with new partners, even oral sex
If it’s been a few months since your last test, or you’re entering a new relationship, now’s a good time to reset. You don’t need fear. You need facts. And you can get them without leaving home.
Order your discreet STD test kit for men today and get answers in minutes. Quiet infections deserve loud attention
FAQs
1. Do I really need to get tested if I feel fine?
Short answer? Yes. Long answer? Hell yes. STDs don’t always come with fireworks. Some of the most common ones in men, like chlamydia and HPV, barely make a peep. You could be walking around with an infection and never know it. That’s not shameful, it’s common. But it’s also a reason to test, not a reason to wait.
2. How soon after sex should I test?
Depends on the STD. Gonorrhea can show up fast (within a week), while syphilis and HIV can take longer. There’s no one-size-fits-all answer, but if you’re worried, test at 2 weeks, then again around 3 months for full peace of mind. Think of it as checking the receipts on your health.
3. Is every bump on my junk an STD?
Not always. Razor burn, pimples, and ingrowns happen. But if it’s painful, leaks, spreads, or just doesn’t look like the usual irritation, get it checked. One guy’s “probably nothing” was another guy’s herpes diagnosis. Better to know than Google in circles.
4. My pee burns. Should I panic?
Not panic, but definitely take it seriously. Burning when you pee is a common red flag for chlamydia and gonorrhea. It could be something else, like a UTI, but you won’t know unless you test. Bottom line: pain isn’t normal. Don’t normalize it.
5. Can I catch an STD from oral?
Yup. Giving or receiving. STDs like gonorrhea, syphilis, and herpes love a good oral exchange. And most people don’t think to use protection for oral, so it spreads easily. If it went in your mouth (or theirs), consider your risk real.
6. Do condoms mean I’m 100% protected?
Not quite. Condoms are awesome at blocking fluid-based STDs like HIV and chlamydia. But skin-to-skin infections like herpes and HPV can still sneak through. Think of condoms as seatbelts, not armor. Essential, but not invincible.
7. Will I get judged at a clinic?
No. And if you do, that’s a bad clinic. But if just the thought of walking in gives you the ick, you’ve got options. Order a home test kit. Same accuracy, zero awkward waiting room energy.
8. Can STDs mess with fertility?
Definitely. Untreated infections like chlamydia or gonorrhea can cause inflammation in your testicles or urethra that messes with sperm delivery. No symptoms doesn’t mean no damage. This is one of those “later regret” situations you can skip with a 10-minute test.
9. Should I get throat or rectal testing?
If you’re doing anything oral or backdoor, yes. Infections can live in those places without symptoms. Most clinics don’t test there by default, so you need to ask. Or grab a test kit that lets you swab where you need to, without explaining your sex life to a stranger.
10. What’s the best test if I just want to check everything?
Go for the 8-in-1 test kit. Covers all the big ones. Comes discreet. You test on your own time, wherever you're comfortable. No clinic, no hassle, no drama.
Get Ahead of the Symptoms, Or the Silence
STDs don’t always look the same in men. Sometimes they’re loud: painful pee, sores, discharge. Other times they’re quiet, and that silence can wreck your body, your relationships, and your peace of mind.
Whether you’re feeling off or just want to be sure, don’t leave it up to chance. Order your test kit today and take control without waiting on symptoms to show up. Being proactive isn’t just responsible, it’s smart.
You can’t control who gave you what. But you can control what you do next.
How We Sourced This
Around fifteen reputable medical and public health sources informed this article, including data from the CDC, WHO, Mayo Clinic, and peer-reviewed studies on STI presentation in male patients. Below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. About Sexually Transmitted Infections (STIs) | CDC
2. Sexually Transmitted Disease (STD) Symptoms | Mayo Clinic
4. Pictures & Facts About STDs | WebMD
5. About Mycoplasma genitalium (Mgen) | CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to prevent, diagnose, and treat STIs. He combines clinical accuracy with a straightforward, sex-positive approach and is dedicated to making his work available to readers in both cities and rural areas.
Reviewed by: K. Simmons, MPH | Last medically reviewed: November 2025







