Quick Answer: Pelvic pain can be caused by an STD, an ovarian cyst, pelvic inflammatory disease, ovulation, a UTI, or other conditions. The timing, type of pain, and accompanying symptoms help narrow it down, but testing is often the only way to rule out infection.
This Isn’t Just “Cramps”, Why Pelvic Pain Feels So Scary
Pelvic pain is uniquely unsettling because it sits at the crossroads of reproduction, sex, and infection. It can signal something minor, like ovulation, or something urgent, like pelvic inflammatory disease caused by untreated chlamydia or gonorrhea. The range is wide, and your body doesn’t exactly label the source for you.
One patient once described it like this: “It felt like a stitch in my side, but lower. I kept thinking, what did I do?” That question is common. Pain in this region is often wrapped in guilt, especially after unprotected sex, even though biology doesn’t operate on morality.
Before we spiral, let’s slow this down and separate three big categories: infection-related pain, structural pain like ovarian cysts, and everything else that can mimic both.
STD-Related Pelvic Pain: What It Actually Feels Like
Not every STD causes pelvic pain. But some absolutely can, especially when they travel upward from the cervix into the uterus and fallopian tubes. That condition is called pelvic inflammatory disease, often shortened to PID.
Here’s where it gets complicated: early chlamydia and gonorrhea are frequently silent. You can have no discharge, no odor, no itching, and still develop deep, aching pelvic pain weeks later. According to the Centers for Disease Control and Prevention, many PID cases begin without dramatic warning signs.
The pain from infection tends to feel like a dull, persistent ache in the lower abdomen. It may worsen during sex, especially deep penetration. It can be accompanied by fever, unusual bleeding, or pain during urination. Sometimes it builds gradually; sometimes it hits suddenly enough to make you double over.
Imagine this: You had sex two weeks ago. Everything seemed fine. Then you start noticing a heavy pressure low in your pelvis. Not sharp like a stab, but constant. You feel off. Maybe slightly feverish. That timeline, exposure followed by delayed discomfort, raises more suspicion for infection than for a cyst that forms independently of sexual contact.

People are also reading: Exposed to HIV? Here’s How PEP Can Stop It Cold
Ovarian Cysts: The Quiet, Common Culprit
Now let’s talk about ovarian cysts. Most people with ovaries will develop small cysts at some point. Many are completely normal, forming during ovulation and disappearing without you ever knowing they existed.
When cysts cause pain, it often feels one-sided. A sharp pain in the left or right lower abdomen. Sometimes it comes in waves. If a cyst ruptures, the pain can be sudden and intense, like someone flipped a switch.
Unlike infection-related pain, cyst pain is not linked to sexual exposure. It often lines up with your menstrual cycle. You might notice it mid-cycle, around ovulation, or just before your period. There is usually no fever. Discharge doesn’t typically change.
A 26-year-old once said, “I was convinced it was an STD because it hurt after sex. But the ultrasound showed a cyst. I had no idea they could hurt that much.” That confusion is common because sex can jostle an already irritated ovary, making a cyst suddenly noticeable.
Side-by-Side Comparison: Infection vs Cyst
This table doesn’t replace testing or imaging, but it gives you a directional clue. Timing and accompanying symptoms matter more than intensity alone.
Other Causes That Mimic Both
Pelvic pain doesn’t read textbooks. It overlaps wildly. A urinary tract infection can create lower abdominal pressure that feels internal and alarming. Endometriosis can cause deep, cyclical pain that worsens during sex. Constipation can radiate discomfort into the pelvis. Even stress can tighten pelvic floor muscles and create real, tangible pain.
There’s also ectopic pregnancy, which is rare but serious. If pelvic pain is paired with missed period, dizziness, or shoulder pain, that is an emergency scenario. Severe pain with fainting or heavy bleeding always warrants urgent care.
One college student once came in terrified it was PID. It turned out to be severe constipation from dehydration during finals week. Bodies are complicated. Assumptions are dangerous.
When Pelvic Pain Is a Red Flag
Most pelvic pain is not life-threatening. But some combinations deserve immediate attention. Fever over 101°F with worsening lower abdominal pain should not be ignored. Sudden, severe stabbing pain with lightheadedness could indicate cyst rupture or internal bleeding. Persistent pain lasting more than a few days without improvement needs evaluation.
It’s not dramatic to seek care. It’s protective. There is no prize for enduring preventable complications.
If none of these apply, you still deserve clarity. Just not panic.
What About Pelvic Pain After Sex?
This is one of the most searched phrases: pelvic pain after sex. It triggers immediate fear. But context matters.
If pain starts immediately during or after deep penetration and fades within hours, it could be positional pressure, a sensitive cervix, or a cyst being bumped. If pain develops days later and lingers, especially with discharge or fever, infection moves higher on the list.
A person once told me, “I kept replaying the night in my head like I’d made some reckless mistake.” That mental spiral is common. But pelvic pain after sex does not automatically mean you have an STD. It means your body is asking for attention and information.
Testing: The Only Way to Rule Out Infection
Here’s the grounded truth: symptoms overlap. You cannot reliably distinguish an STD from a cyst based on sensation alone. Testing provides clarity.
If you’ve had new or unprotected sexual contact in the past two weeks and pelvic pain develops, screening for chlamydia and gonorrhea is reasonable. After 7 to 14 days of exposure, most tests get more accurate. Testing too soon can give you false hope.
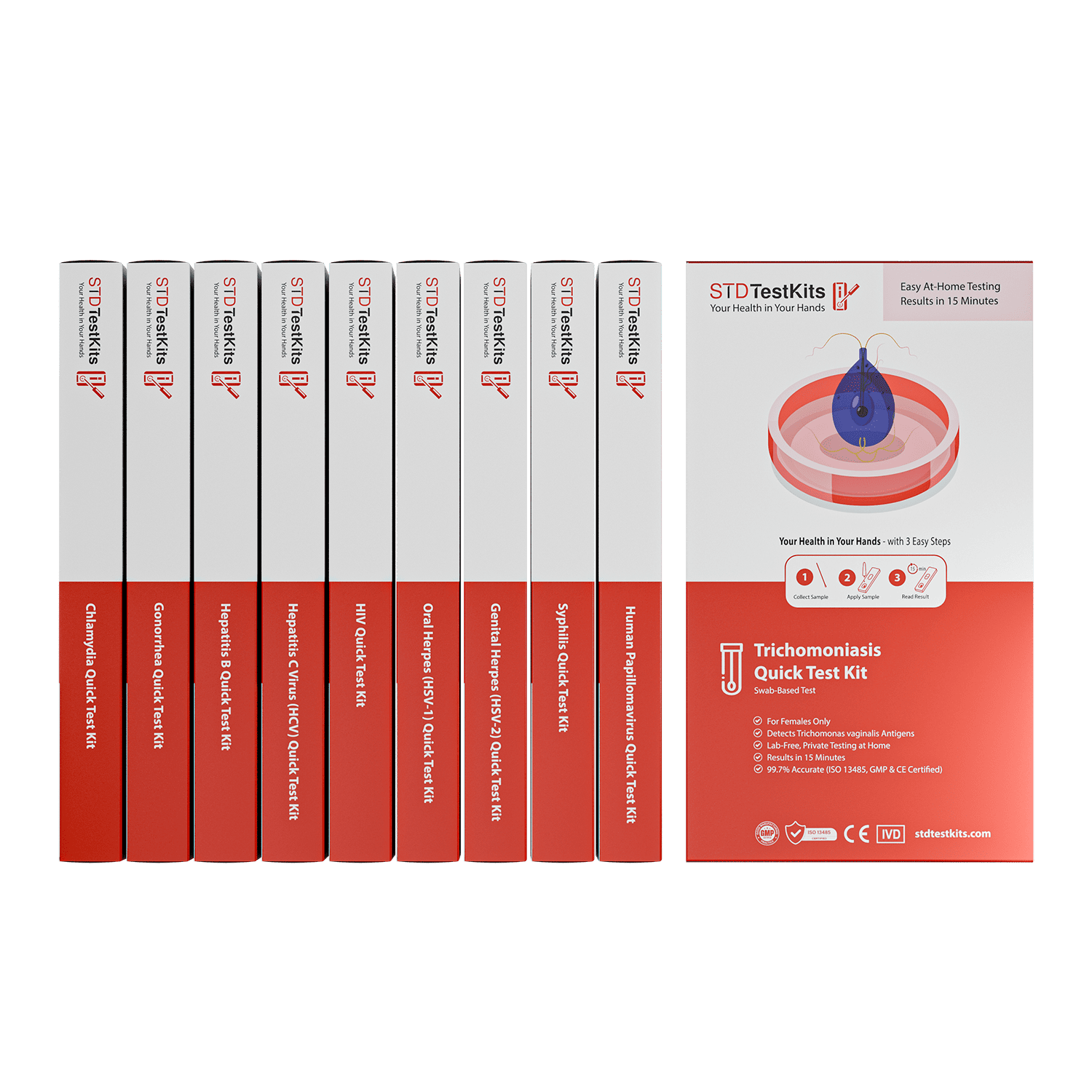
STD Rapid Test Kits can help you find private options if privacy or access is important to you. Some people prefer the control of testing at home rather than sitting in a waiting room replaying worst-case scenarios.
If your test is negative and pain persists, imaging like an ultrasound can evaluate for cysts. Infection and cysts are not mutually exclusive, but they are evaluated differently.
Timeline Matters More Than Intensity
Think of pelvic pain like a story unfolding over time. Day one after sex with sudden sharp pain? Less likely infection. Two weeks later with gradual worsening? More suspicious.
Below is a simplified timeline comparison to help contextualize symptoms.
Patterns don’t diagnose you. They guide your next move.
When It’s Not an STD or a Cyst, The Overlooked Causes
Let’s zoom out for a second. Not every ache in your pelvis traces back to infection or ovaries. Sometimes the answer is less dramatic, but no less real.
Urinary tract infections can create a heavy, internal pressure that feels deeper than bladder-level discomfort. You might notice burning with urination or a constant urge to pee, but sometimes pelvic fullness shows up first. The line between bladder pain and reproductive pain is thinner than people think.
Endometriosis tells a different story. The pain is often cyclical, intensifying before or during a period. It can feel sharp, pulling, or deeply throbbing. It may radiate into the lower back. Sex can worsen it, which often causes unnecessary panic about infection.
Then there’s pelvic floor dysfunction. Stress, trauma, or chronic tension can cause the muscles in the pelvic region to tighten involuntarily. That tension creates aching, pressure, and even pain during sex. One patient once said, “I thought I had something contagious. It turned out I was clenching all the time without realizing it.” Bodies carry stress in surprising places.
Digestive issues also overlap. Constipation can create cramping low in the abdomen that mimics gynecologic pain. Gas can create sharp stabs that feel one-sided. It’s not glamorous, but it’s common.
The Emotional Spiral: Why We Jump to STDs First
Here’s something I see constantly. Someone has sex. Days later, they feel pelvic pain. The mind connects those dots instantly. It must be an STD. That leap feels logical because the timeline lines up emotionally, even if medically it doesn’t.
Shame fuels that spiral. We tend to assume pain is punishment. It isn’t. Biology does not assign moral weight to your sex life.
A 31-year-old once told me, “I kept thinking, this is what I get.” She had an ovarian cyst. No infection. No STI. Just a functional cyst that resolved on its own. The anxiety was louder than the diagnosis.
This is why testing can be psychologically powerful. Even when results are negative, clarity interrupts the fear loop.

People are also reading: That Rash Isn’t Random: STD vs COVID Skin Symptoms Explained
If It Is an STD: What That Actually Means
If pelvic pain turns out to be related to chlamydia or gonorrhea, the bigger concern is not the discomfort itself but the inflammation it can cause when untreated. Pelvic inflammatory disease can affect fertility if ignored for too long. That sounds scary, but early detection dramatically reduces long-term complications.
The key word there is early. Most infections are treatable with antibiotics. Treatment is straightforward. The sooner you address it, the simpler it is.
If you’re unsure and want privacy, a discreet option like the Combo STD Home Test Kit can screen for common infections from home. That doesn’t replace emergency care when needed, but it can provide clarity when symptoms are mild and anxiety is high.
There is no shame in testing. It’s not an admission of recklessness. It’s a form of self-respect.
If It’s an Ovarian Cyst: What Usually Happens
Most ovarian cysts resolve without intervention. Functional cysts, the kind tied to ovulation, often shrink on their own within a cycle or two. Pain can be managed with rest, hydration, and over-the-counter anti-inflammatory medication if medically appropriate.
Occasionally, cysts grow larger and require monitoring. Rarely, they twist the ovary, a condition called torsion, which causes sudden, severe pain and requires urgent treatment. That scenario is uncommon but important to recognize.
One woman described her rupture like this: “It felt like something popped. I had to sit down immediately.” That kind of sharp, acute onset differs from the creeping discomfort of infection.
Ultrasound is typically the tool used to confirm a cyst. Testing alone cannot detect one.
When to Test, When to Image, When to Wait
Here’s the grounded, practical roadmap.
If you’ve had recent unprotected sex and pelvic pain develops within one to three weeks, testing for chlamydia and gonorrhea is reasonable. Most nucleic acid tests are reliable about 7 to 14 days after exposure. Testing earlier can produce false negatives, which creates false reassurance.
If pain is clearly one-sided and tied to your cycle, imaging may be more informative than infection screening. If pain is mild, without fever, and improves within 48 hours, observation can be appropriate.
If pain worsens, persists beyond a few days, or pairs with fever, dizziness, or unusual bleeding, medical evaluation should not be delayed.
Clarity is a sequence. You don’t have to solve everything in one hour. You take the next logical step.
The “Negative Test but Still in Pain” Scenario
This situation rattles people. You test for STDs. Results are negative. The pain remains. Now what?
First, breathe. A negative test significantly lowers the probability of infection, especially if taken at the appropriate window period. It doesn’t mean the pain is imaginary. It means the cause likely lies elsewhere.
This is often when cysts, endometriosis, gastrointestinal causes, or pelvic floor issues surface. It’s not a failure of testing. It’s refinement of diagnosis.
A patient once said, “I almost wished it had been positive because at least then I’d have an answer.” That’s the psychology of uncertainty. But answers can take a couple of steps. That doesn’t mean you’re lost.
Pelvic Pain With No Discharge, Should You Worry?
Many people assume that STDs always come with dramatic discharge. That’s not true. Chlamydia in particular is often silent. Pelvic inflammatory disease can develop without obvious external signs.
At the same time, cysts rarely change discharge. Hormonal shifts can slightly alter it. UTIs may cause urinary symptoms without vaginal changes.
So the absence of discharge does not rule out infection, but it also does not confirm it. This is why relying solely on one symptom leads to confusion. Patterns matter. Testing clarifies.
What To Do Tonight If You’re in Pain
If you’re reading this while holding your abdomen, here’s the immediate framework. Check your temperature. Notice whether the pain is one-sided or central. Reflect on recent sexual exposure. Pay attention to dizziness or faintness.
If symptoms are mild and stable, schedule testing or evaluation within the next few days. If symptoms are escalating or severe, seek urgent care. There is no bravery in ignoring worsening pain.
Most pelvic pain resolves with either time, antibiotics, or simple supportive care. Catastrophic outcomes are rare, especially when people act promptly.
FAQs
1. Can an STD really cause pelvic pain even if I don’t have discharge?
Yes. And that’s what makes it tricky. Chlamydia in particular is famous for being quiet at first. You might feel completely normal until inflammation travels upward and suddenly there’s this deep, aching pressure that won’t go away. No dramatic discharge. No flashing neon sign. Just a body whisper that slowly turns into a nudge. That’s why timing and testing matter more than one single symptom.
2. If it’s a cyst, why did it hurt right after sex?
Sex can jostle things. Deep penetration can press against an ovary that already has a small cyst forming, and suddenly you feel it. That doesn’t mean sex caused the cyst. It means it revealed it. Think of it like bumping a bruise you didn’t know you had. The bruise wasn’t new, the awareness was.
3. I had unprotected sex last week and now I have pelvic pain. Is that too soon for an STD?
It depends. Some infections can begin causing symptoms within a week, but many take 7 to 14 days before tests reliably detect them. If it’s been only a few days, intense sudden pain is more likely something mechanical or cyst-related. If it’s been about two weeks and the pain is lingering or worsening, that’s when infection climbs higher on the list. Your calendar actually matters here.
4. How do I know if this is serious or if I’m just anxious?
Anxiety makes pain louder, but it doesn’t invent it. Check the basics. Do you have a fever? Are you dizzy? Is the pain sharp and unbearable, or uncomfortable but stable? If your body feels dramatically worse over hours, get care. If it’s steady and mild, you likely have time to test or schedule an appointment without panic. Urgency shows itself. Catastrophe rarely whispers politely.
5. What does pelvic inflammatory disease actually feel like?
Most people describe it as a heavy, central ache. Not a quick stab. Not a fleeting cramp. More like a persistent pressure low in the abdomen that doesn’t quite let up. Sex can make it worse. You might feel slightly feverish or just “off.” It’s less cinematic than Google makes it sound, and more nagging than explosive.
6. Can ovarian cyst pain move from one side to the other?
Usually it stays on one side, because it’s tied to one ovary. But bodies shift. Gas moves. Muscles tighten. So sometimes what starts as right-sided discomfort can feel more diffuse later. What’s more telling is whether it lines up with your cycle. Mid-cycle, one-sided pain that fades within a day or two often points toward ovulation or a small functional cyst.
7. I tested negative for STDs but the pain hasn’t stopped. Did I test wrong?
Not necessarily. If you tested within the correct window period, a negative result is meaningful. It doesn’t invalidate your pain. It just shifts the investigation. This is when cysts, endometriosis, digestive issues, or pelvic floor tension deserve attention. A negative STD test is a narrowing of the field, not the end of the road.
8. Can stress actually cause pelvic pain, or is that just something doctors say?
Stress absolutely affects the pelvic floor. When you’re anxious, your muscles tighten. Most people don’t realize they’re clenching their jaw and their pelvis at the same time. Chronic tension in those muscles can create aching, pressure, and even pain during sex. That doesn’t mean it’s “in your head.” It means your nervous system and your body are talking loudly to each other.
9. Should I test first or get an ultrasound first?
If there’s recent sexual exposure and you’re within that 7–14 day window, testing is usually the simplest first step. It’s noninvasive and gives fast clarity. If the pain is clearly one-sided and cycle-related, imaging might be more revealing. Sometimes it’s not either-or. It’s step one, then step two. Diagnosis is a sequence, not a single dramatic reveal.
10. Why does pelvic pain always feel so scary?
Because it lives in a vulnerable place. It touches sex, fertility, intimacy, and identity. Pain there can feel personal. But most pelvic pain ends with an answer that is manageable, treatable, or temporary. The fear is often louder than the outcome. And the more information you gather, the quieter that fear gets.
You Deserve Answers, Not Assumptions
Pelvic pain is not a verdict. It’s a signal. Sometimes that signal points to infection. Sometimes to a cyst. Sometimes to something entirely different. The goal is not to panic but to respond intelligently.
If there’s any chance recent sexual exposure could be involved, testing provides clarity. You can explore discreet options through STD Rapid Test Kits and take the next step from home if that feels safer. Knowledge lowers anxiety. Action restores control.
You don’t have to sit alone in the spiral. You just have to take the next right step.
How We Sourced This Article: This guide was built using current clinical guidelines from the Centers for Disease Control and Prevention, peer-reviewed research on pelvic inflammatory disease and ovarian cyst management, and patient-centered reporting on lived experiences of pelvic pain.
Sources
1. CDC – Pelvic Inflammatory Disease Treatment Guidelines
3. Mayo Clinic – Ovarian Cysts
5. WHO – Sexually Transmitted Infections Fact Sheet
6. NIH – Pelvic Inflammatory Disease Overview
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access to accurate sexual health information.
Reviewed by: A. Martinez, MD, OB-GYN | Last medically reviewed: February 2026
This article is only meant to give you information and should not be used as medical advice.