STD Window Periods: Why Testing Too Soon Can Give You a False Negative
Quick Answer: Testing too soon for gonorrhea, usually within 1 to 5 days of exposure, can lead to false negatives. Most tests are most accurate 7 to 14 days after contact.
This Isn’t Just You, It’s Science
Gonorrhea doesn’t show up on tests the minute it enters your body. Like all infections, it needs time to incubate and replicate enough to be detectable. That lag time is known as the window period, and testing during it can give you a false sense of security.
According to the CDC, gonorrhea symptoms may appear 2–7 days after exposure, but not always. And in many cases, people are asymptomatic but still contagious. That means even if you feel fine, or your test was negative, the infection could still be developing in the background.
Malik, 23, found out the hard way.
“I hooked up on a Saturday, felt itchy by Tuesday, tested that Thursday, and it came back clean. I thought I was in the clear… until I retested the next week and it was full-blown gonorrhea.”
People are also reading: My STD Symptoms Vanished. Was I Cured, Or Just Lucky?
How the Gonorrhea Test Actually Works
Most modern tests for gonorrhea use something called NAAT, nucleic acid amplification testing. It’s like a high-powered genetic microscope that looks for the DNA of Neisseria gonorrhoeae, the bacteria that causes the infection. NAATs are extremely accurate, but only when there’s enough bacterial material to find.
And if you test before the bacteria has multiplied to detectable levels? Even the most sensitive test might come up empty.
Figure 1. Gonorrhea test types and their timing. Testing too early may yield a negative even if infection is present.
If your exposure was recent, especially within the last five days, it’s often recommended to wait and retest after the 7–14 day window for best accuracy.
“I Got a False Negative. Then I Gave It to My Partner.”
Sofia, 26, took a rapid test at home four days after a condom slipped during sex with a new partner. “I was nervous, but the test came back negative, so I relaxed,” she said. “We kept having sex, no symptoms, no worries. Until he started burning when he peed and got tested. Boom: positive for gonorrhea.”
Her retest, taken 12 days after the original exposure, was also positive.
“I felt awful. I thought I’d done the responsible thing. I didn’t realize testing too soon could miss it.”
Now, she tells friends to test and retest.
“One negative isn’t always the final answer. Especially if your gut says something’s off.”
So, When Should You Retest?
If your first test was negative but it’s only been a few days since the exposure, or if you’re suddenly dealing with symptoms, retesting is not overkill. It’s smart. Think of the first test as a snapshot. Sometimes it’s clear. Sometimes it’s blurry. Retesting sharpens the picture.
The best window to retest for gonorrhea is typically 7 to 14 days after exposure. That’s when most NAAT tests hit peak accuracy. If you still have symptoms after a negative test, or if you tested within the first 5 days, a follow-up test could catch what the first one missed.
If you're using an at-home test, choose one that aligns with the exposure date. Some people even buy two, testing once early and again a week later, to reduce the mental load of waiting. It’s not overthinking. It’s taking care of yourself and your partners.
This Combo STD Kit covers gonorrhea and six other common STDs, and includes clear instructions on when and how to test based on exposure type.
Symptoms After a Negative Test? Here’s What’s Going On
If you’re itching, burning, spotting, or dealing with discharge, but your test was negative, it’s tempting to write it off as something else. A reaction. A yeast infection. Maybe stress. But here’s the thing: gonorrhea symptoms can absolutely show up even if your test says “nope.”
Symptoms that don’t match your test = retest.
And remember, some symptoms are subtle. For people with penises, it might just be a weird tingle when peeing. For those with vaginas, it might be unusual discharge or pelvic discomfort. And for oral or anal infections, you may have no symptoms at all, but still be contagious.
If you feel like your body is waving a red flag, listen to it. You’re not being dramatic. You’re being tuned in.

People are also reading: Syphilis Exposure Timeline: What Happens in the First 30 Days
Let’s Be Clear: You Didn’t Screw This Up
False negatives are common, and not because people are careless. They happen because most of us don’t know the fine print on STD test timing. No one teaches this in school. And when you’re scared or ashamed or just trying to be “responsible,” early testing feels like the right thing to do.
It still is. But it’s just the first step.
Testing too soon doesn’t make you dumb. It makes you normal. So if you tested early and something still feels off, it’s not a failure to test again. It’s courage. It’s care. It’s doing what’s right for your health and for anyone else involved.
If you’re ready to stop wondering and start knowing, order a discreet at-home STD test kit today and time it based on your last exposure. You’ve got options. You’ve got time. And you’ve got backup.
False Negatives by the Numbers
Let’s put some data behind the worry. While NAAT tests for gonorrhea are extremely accurate overall, their reliability depends on timing. Testing during the window period, even just a couple days too early, can mean the infection is missed completely.
Here’s what that looks like in real-world terms:
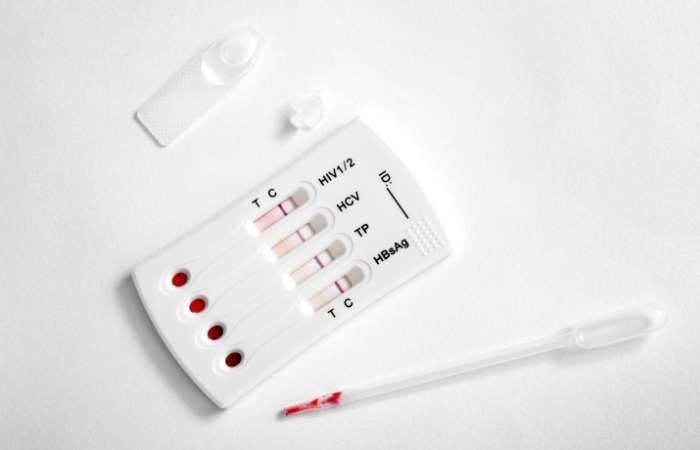
Figure 2. Estimated false negative risk by testing window. Early testing carries the highest chance of missed infection.
If you're reading this and realizing your first test fell in the "too soon" zone, take that as a cue, not a mistake. It means you’re paying attention.
Still Hooking Up? Here’s How to Stay Protected While You Wait
If you're still sexually active while waiting to retest, or between potential exposures, here's how to lower the risk of spreading (or picking up) gonorrhea, especially if you're not sure where you stand yet:
- Use condoms consistently, and put them on before any genital contact, not halfway through.
- Avoid oral and anal without protection. Gonorrhea doesn’t just stay below the belt.
- Get partners tested too. Suggest it as mutual care, not blame.
- Skip sex entirely if you have symptoms, burning, discharge, sore throat, or anything weird.
Testing isn’t just about you. It’s about protecting the people you care about, even the ones you just met last weekend.
“My Partner Had Gonorrhea, But My Test Was Negative”
Ray, 32, got the heads-up from an ex who tested positive for gonorrhea. He’d already taken a test the week before, negative.
“I almost didn’t believe her. I felt fine, and my results were clear.”
But something didn’t sit right. He retested nine days after their last hookup. This time: positive.
“If I hadn’t gone back, I could’ve infected someone else thinking I was clean,” he said. “I’m so glad I listened to that tiny voice in the back of my mind.”
Gonorrhea doesn’t always speak loudly at first. But when it does? You want to be ready to hear it, and act fast.
Negative Test, But Something Still Feels Off? Here’s What It Might Mean
You peed in the cup. You did the swab. The test came back negative. And yet, your body’s still whispering, “Something’s wrong.” Whether it's a tingle, an ache, or a discharge situation that wasn't there last week, you're not overthinking. You're just catching something your test might have missed.
This is one of the most confusing (and panic-inducing) parts of STD testing: getting a negative result, but still feeling off. Here's how that disconnect happens, and what it might mean depending on where you are in the timeline.
Figure 3. Common post-test symptoms and what they could indicate depending on timing and test type.
This is why timing matters so much. A false negative gonorrhea test doesn’t mean you’re in the clear. It means your body and the test were just out of sync. And when they finally line up? That’s when you get the real answer.
FAQs
1. Can you really test too early for gonorrhea?
100% yes. Gonorrhea doesn't clock in and announce itself right away. It needs time to multiply before a test can catch it, usually around 7 days. If you tested 2–3 days after a hookup? That’s like asking a plant to grow before you’ve even watered the soil.
2. I tested negative but I’ve got symptoms. What gives?
That test might’ve just been early, or the bacteria was hanging out below detection levels. If you’re feeling that infamous burn, weird discharge, or anything that makes your pants feel haunted, don’t shrug it off. Retest. Your body knows things before your test does.
3. How long does it actually take for gonorrhea to show up on a test?
Most experts recommend waiting at least 7 days after exposure for accurate results. Some people may test positive earlier (around day 4 or 5), but sooner than that? You're mostly rolling the dice.
4. Can you have gonorrhea and not know it?
Oh, absolutely. Many people walk around with gonorrhea and zero symptoms, especially if it’s in the throat or rectum. That’s why regular testing matters, not just post-drama panic testing.
5. Is one test enough?
Not always. Especially if you tested early, or you’ve had new partners. Think of that first test like a smoke alarm, it’s helpful, but it might not catch a slow-burning fire. If something feels off, test again.
6. Can I still pass it on if I tested negative?
If your test was too early? Yep. You could be contagious and not even know it. That's why it's smart to use protection and have those “hey-let’s-both-get-tested” convos early and often.
7. What does ‘false negative’ actually mean?
It means the test said “you’re good” but the bacteria was still lurking. It’s not a fail on your part. It’s just that tests aren’t fortune tellers, they need something to detect. No bacteria = no red flag = false sense of safety.
8. How do I know when to test again?
If it’s been less than 7 days since your exposure and your test was negative, wait a week and test again. If you're panicking in the meantime, that’s normal. But facts beat fear, and timing matters.
9. Can I use an at-home test for this?
Absolutely. This combo test kit checks for gonorrhea and six other STDs. It’s private, fast, and way less stressful than playing phone tag with your clinic.
10. What if I already tested early and now I’m spiraling?
Take a breath. You didn’t mess up, you acted fast, and that’s good. Just back it up with a second test at the right time. And if you’re feeling anxious? That’s not weakness. That’s awareness.
You’re Not Paranoid. You’re Paying Attention.
False negatives are more common than people think, not because the tests are bad, but because timing is everything. Testing too soon for gonorrhea can leave you falsely reassured, still contagious, and wondering what went wrong.
If you’re reading this, you’re already doing better than most. You’re checking the facts. You’re double-checking your body. And that’s exactly what smart, careful, sexually active people do.
Ready to retest or get a clearer answer? Order your confidential home STD test kit here. No clinics. No judgment. Just facts, results, and peace of mind, on your schedule.
How We Sourced This Article: We combined clinical data from leading health agencies with real user experiences and case studies to break down a common but rarely explained issue: false negative gonorrhea tests. About 15 high-quality references informed this article. Here are six of the most relevant:
Sources
1. Healthline – Gonorrhea: Symptoms, Diagnosis, and Prevention
2. WHO – Sexually Transmitted Infections Fact Sheet
3. Planned Parenthood – Gonorrhea Overview
4. How Long Does It Take for Gonorrhea to Show Up? | Healthline
5. Gonococcal Infections Among Adolescents and Adults | CDC
6. Gonorrhea Testing: Types, Accuracy, Timing, and Necessity | STD Center NY
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to stop, diagnose, and treat STIs. He combines clinical accuracy with a straightforward, sex-positive attitude and is dedicated to making his work available to more people, both in cities and in rural areas.
Reviewed by: S. McCall, MSN, FNP-BC | Last medically reviewed: September 2025
This article is for informational purposes and does not replace medical advice.