How Long Can Chlamydia Stay in Your Body Without Symptoms?
Quick Answer: Endometriosis and PID from chlamydia can cause similar pelvic pain, cramping, and spotting. But PID is an active infection that needs urgent antibiotic treatment to prevent long-term damage. Testing is the only way to tell them apart.
When Pelvic Pain Isn’t What You Think
Endometriosis is a master of disguise. It mimics other conditions, flares inconsistently, and evades detection. But that same shapeshifting nature means it’s also a convenient catch-all diagnosis. Too convenient. Because in the absence of classic STD symptoms, like unusual discharge or painful urination, many providers default to "it's probably your endo acting up" and stop there.
That’s how chlamydia can quietly evolve into PID. It climbs through the cervix and into the uterus, fallopian tubes, and ovaries, causing inflammation, internal scarring, and chronic pain. And for many people, there are no early warning signs. No fever. No smell. No clue. Until one day the pain spikes or bleeding shows up out of cycle, and suddenly everything hurts for a reason you can’t quite name.
If you’ve ever had an “endo flare” that felt different, deeper, more sudden, or not tied to your usual patterns, it’s worth considering that it might not be endo at all. Especially if you’re sexually active, have had a new partner recently, or haven’t been tested in a while.
Testing doesn’t mean you’re “dirty” or promiscuous. It means you’re paying attention, and catching something that could cause permanent damage if ignored.
People are also reading: Can You Get Trich Without Cheating?
Why These Conditions Get Confused All the Time
On paper, endometriosis and pelvic inflammatory disease can look shockingly similar. Both can cause lower abdominal pain, painful periods, pain during sex, fatigue, and spotting between cycles. But the root causes couldn’t be more different. One is caused by endometrial-like tissue growing outside the uterus. The other? A bacterial infection, usually from chlamydia or gonorrhea, that’s gone too far.
Here’s the problem: many providers don’t routinely test for STDs unless you ask. And if you already have a known endometriosis diagnosis, new symptoms often get folded into that narrative, even when something new is going on. That leads to missed diagnoses, worsening infections, and unnecessary suffering. It also means people with endo are at higher risk of untreated PID simply because no one thought to check.
What’s worse? Sometimes people are misdiagnosed with endo when it’s really PID all along.
“They Said It Was Just My Endo. It Was Actually PID.”
Alyssa, 31, had been diagnosed with stage II endometriosis at 26. She’d managed it with birth control and NSAIDs, but when she started dating again after a long breakup, something changed. Two weeks after unprotected sex with a new partner, she felt a deep cramp radiating down her thighs, along with bloating and light spotting. Her doctor said, “It’s just your endo again,” and sent her home with stronger meds.
“But it felt different. It was sharper, not cyclical, and it didn’t respond to my usual meds. I went back two weeks later and basically begged for an STD panel.”
The test came back positive for chlamydia. By then, the infection had progressed into PID. She needed a strong course of antibiotics and two follow-up visits. Her doctor admitted they hadn’t considered PID because “she didn’t fit the profile.”
“I was furious. They thought I was too ‘put-together’ to have an STD. But if I hadn’t pushed, I might’ve lost my chance to have kids.”
This happens more often than you'd think. And it’s why we need to talk about the overlap, loudly, clearly, and without shame.
If any of this sounds familiar, don’t wait for someone else to take you seriously. You can test discreetly at home, without judgment or delay.
Symptoms That Blur the Line
If you've ever Googled “pelvic pain no discharge” or “is this endo or an infection,” you already know the search results are a minefield. That’s because the symptoms of endometriosis, chlamydia, and PID often blur together in real life, especially when they show up subtly or overlap.
One person might feel a dull, persistent ache. Another might notice pain only during sex. Some have spotting mid-cycle. Others feel bloated, feverish, or emotionally off without knowing why. And then there are those with absolutely no symptoms, until the damage is done.
Here’s how the common signs compare, so you know what to flag, and when to test instead of guessing.
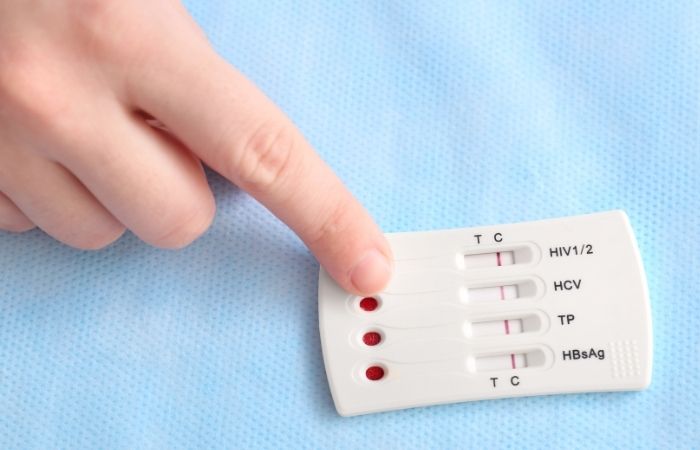
Figure 1. Overlapping symptoms of endometriosis, chlamydia, and PID. Note how nonspecific or subtle signs can delay diagnosis.
If you’re experiencing a mix of these signs, especially pain outside your normal cycle or new discomfort with sex, don’t chalk it up to stress or “just your endo.” It could be something else, something you can test for and treat.
The Diagnosis Trap: When Familiar Pain Masks a New Problem
Endo warriors are used to pain. That’s the problem. You’ve likely learned to tolerate discomfort that would send most people to urgent care. But when new pain arises, especially between periods or after sex, it’s easy to assume it’s “just another flare.” That assumption can delay diagnosis of an active infection, and that delay can cause scarring, blocked tubes, and long-term reproductive damage.
In a 2023 study published in Reproductive Health, researchers found that up to 18% of PID cases were initially misdiagnosed as endometriosis in patients with a history of chronic pelvic pain. That’s not a small number. And many of those patients had gone weeks, or even months, without proper treatment because no one thought to test.
If you've had a recent partner, especially if protection wasn’t used every time, and your symptoms feel new or more intense, a discreet STD test is a smart next step. You don’t need to wait for a doctor’s approval to prioritize yourself.
Partner Awareness: It’s Not Just About You
Let’s be real, if it turns out your pelvic pain is from chlamydia or PID, you’re not just dealing with physical symptoms. There’s the emotional weight too: Who did I get this from? Did I pass it to someone else? What does this mean for my relationships?
Here’s what matters most: you’re not to blame. STDs are incredibly common, often silent, and they don’t care about relationship status, body count, or how “safe” you felt. What matters now is that you know, and that you communicate. Testing doesn’t just help you, it protects your partner too, and lets you both move forward with honesty and care.
Worried about having that conversation? We’ve got a guide for that. But first, get the clarity you need.
What Happens If You Wait Too Long?
Whether it’s endo or PID, time matters. But with PID caused by untreated chlamydia or gonorrhea, the stakes are especially high. The longer the infection goes untreated, the more likely it is to cause permanent internal scarring, adhesions, and even damage to the fallopian tubes. In many cases, the pain doesn’t go away even after the infection clears, because the inflammation has already changed your anatomy.
Let’s break down how these three conditions progress over time if misdiagnosed or untreated:
Figure 2. Progression and consequences of delayed or missed treatment for PID, chlamydia, and endometriosis.
One major difference? PID is treatable with antibiotics, if caught early. Endometriosis, by contrast, is chronic and often requires hormonal or surgical management. That’s why knowing what you’re dealing with matters. Because not knowing could cost you everything from your fertility to your peace of mind.
False Negatives and Retesting: Why One Test Isn’t Always Enough
You finally get brave enough to test. You order the kit, swab or pee, send it off, wait. The result comes back: negative. Huge relief, until the pain gets worse. What gives?
This is when timing is important. There are times when you can get STDs, which is the time between when you get them and when a test shows that you have them. Chlamydia usually takes 7 to 14 days to show up. But if you test too soon, especially within a few days of having sex, you might get a false negative.
Here’s a solid retesting timeline to keep in your back pocket:
- If you test within 5–7 days of exposure: consider it a baseline, and retest at 2–3 weeks
- If symptoms worsen or persist despite a negative test: retest after 10–14 days
- If you're diagnosed with PID but test negative for STDs: request a repeat panel with NAAT (nucleic acid amplification) testing
This isn’t paranoia, it’s protocol. Because missing an active infection due to poor timing can delay treatment, especially when symptoms mimic endo flares. You deserve certainty, not guesswork.
And if your provider won’t listen? That’s what at-home testing is for.

People are also looking for: Trichomoniasis Symptoms in Women vs Men
“I Was Diagnosed With Endo, Then Found Out It Was an STD”
Jamie, 28, had been dealing with pelvic pain since college. After years of being dismissed, she finally got an endometriosis diagnosis and felt relieved, like she had a name for the pain. But six months later, things changed. She had a new partner, started bleeding between periods, and the pain shifted. It wasn’t cyclical anymore. It burned.
Her OB chalked it up to stress and hormone fluctuations. But Jamie ordered an at-home test anyway. It came back positive for chlamydia. Her provider was stunned. Jamie wasn’t. She’d started listening to her body more than her medical charts.
“I almost let my ‘endo’ diagnosis blind me to what was really happening. If I hadn’t tested again, I might have ended up in the ER with PID.”
Jamie’s story is proof that two things can be true. You can have endo and get an STD. You can feel symptoms that don’t match your usual pattern. And you can reclaim your health story, even if you’ve been misdiagnosed before.
If something feels different, trust your gut and test. You’re not overreacting. You’re protecting your future.
FAQs
1. Can chlamydia really feel like endometriosis?
Honestly? Yes. You might feel cramping that won’t quit, dull pelvic pressure, spotting that throws off your whole cycle. It can look a lot like an endo flare, until it doesn’t. The big difference? Chlamydia is an infection, not a chronic condition. And it doesn’t go away without treatment.
2. What if I have both PID and endo?
Then you're not alone. Plenty of people with endo have also had chlamydia or PID and didn’t know it. In fact, chronic pain conditions can mask or overlap with infections. That’s why knowing your “normal” is so important, because when something feels off, it probably is.
3. I don’t have discharge or a fever. Could it still be PID?
100%. PID doesn’t always show up with a dramatic entrance. Sometimes it’s just persistent cramping, pain during sex, or a weird feeling deep in your pelvis. If you’re thinking, “This doesn’t feel like my usual endo,” trust that instinct and test.
4. What’s the quickest way to find out if it’s chlamydia or gonorrhea?
At-home combo STD tests are your best friend here. No clinic. No eye contact with a nurse who mispronounces your name. Just a discreet kit, accurate results, and peace of mind. Fast. Quiet. Empowering.
5. Can chlamydia really make me infertile?
Yes, and that’s what makes early testing so critical. Left untreated, it can quietly inflame your reproductive organs and evolve into PID, which causes scarring in the fallopian tubes. The scary part? You might not even know it's happening until years later.
6. I already have an endo diagnosis. Do I still need to test for STDs?
Absolutely. An endo diagnosis doesn’t mean you're immune to infections. If anything, it makes self-advocacy even more crucial. Don’t let doctors write off every symptom as “just your endo”, especially if something feels new or different.
7. If I test at home, will anyone else see the results?
Nope. No insurance trail. No surprise lab bills. And no awkward EHR notes that follow you forever. You control the results, the timing, and whether or not anyone else ever sees them.
8. How soon after sex can I test?
The sweet spot is 7–14 days after exposure for chlamydia and gonorrhea. Test too early, and you might miss it. If you're feeling anxious, test now, and again in a few weeks to be sure. It's not overkill. It's ownership.
9. Can PID go away on its own if I just wait it out?
Wishful thinking. PID is serious business and needs antibiotics ASAP. Waiting it out can lead to long-term complications like infertility or chronic pelvic pain. This isn’t one of those “let’s see if it gets better” situations. It won’t.
10. My doctor brushed me off. What do I do now?
You take the power back. Order an at-home test. Book with a provider who listens. And know this: being dismissed doesn’t mean your symptoms aren’t real. It just means you need a better team. You're not overreacting, you’re advocating.
You Know Your Body. Trust It.
If you're reading this, you're probably already doing what too many providers don’t: paying attention. Whether it’s a new kind of pain, bleeding that doesn’t fit your cycle, or just a gut feeling that something isn’t right, trust that instinct. Endometriosis is real. So are STDs. So is the risk of confusing the two when no one’s looking close enough.
But you can change the script. You don’t have to choose between silence and suffering. You can test. You can get treated. And you can move forward with facts instead of fear.
Order a discreet combo STD test kit today, because what you don’t know can hurt you, and what you do know can change everything.
How We Sourced This Article: This article was developed using guidance from major public health agencies, clinical research journals, and patient-led endometriosis communities. Around fifteen reputable sources informed this content. Here are five key ones that shaped what you’ve just read.
Sources
2. Similarities in Pathogenetic Mechanisms Underlying Endometriosis and PID | PMC
3. Eutopic Endometrium from Women with Endometriosis and Chlamydia-Induced Endometritis – ScienceDirect
4. Pelvic Inflammatory Disease (PID): Symptoms & Treatment | Cleveland Clinic
5. Endometriosis – Symptoms and Causes | Mayo Clinic
6. PID and Endometriosis – Dr Seckin
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who advocates for better STI education and diagnostic clarity across age groups. His work focuses on eliminating shame from sexual health care and expanding access to reliable, fast testing options for everyone, especially those misdiagnosed or ignored.
Reviewed by: Dr. N. Lin, DO, OB-GYN | Last medically reviewed: September 2025
This article is for informational purposes only and does not substitute professional medical advice, diagnosis, or treatment.






