When to Test for Syphilis After Exposure (And When Not To)
Quick Answer: Reduced STD testing means fewer diagnoses, which leads to underreporting, delayed treatment, and increased transmission, especially among asymptomatic carriers. It also weakens public health data, making outbreaks harder to track and contain.
Testing Gaps Aren’t Just a “You” Problem
In early 2023, a college senior named Jules skipped her routine STD test. She was in a new monogamous relationship, hadn’t had any symptoms, and figured it could wait. Three months later, her partner tested positive for chlamydia. Jules never developed symptoms. But when she finally got tested, she was positive too, and likely had been transmitting it unknowingly. “I felt guilty, but also mad,” she shared. “I thought we were being responsible.”
This story isn’t rare. According to CDC surveillance data, as many as 70% of chlamydia cases and 50% of gonorrhea cases are asymptomatic, meaning people can spread the infection without ever knowing. And when people don’t get tested, those cases never enter official records.
That’s where the accountability problem begins. Public health relies on confirmed diagnoses to allocate funding, issue alerts, and adjust outreach. Fewer tests mean fewer “confirmed” infections, even if the actual transmission rates are climbing. It's not just dangerous, it's misleading.
People are also reading: I Treated a Yeast Infection for Months, It Was an STD
The Domino Effect: One Missed Test Becomes Many
When individuals skip testing, it doesn’t just affect their own health. It cascades through sexual networks. Here's how:
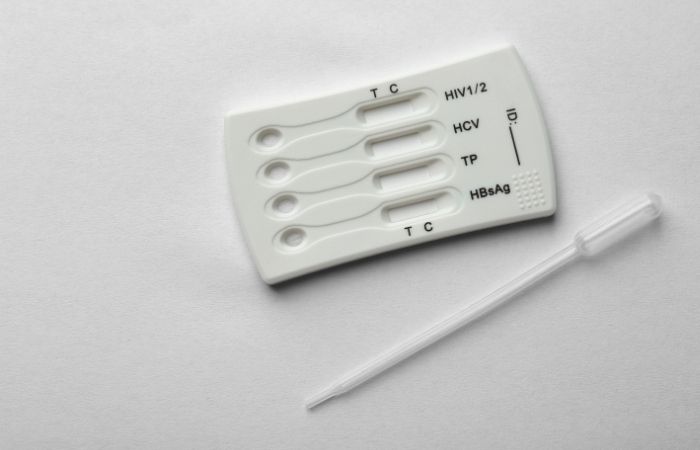
Figure 1. Chain of underreporting: how missed tests lead to silent spread and flawed data.
This is how the system fails. Not from malice, but from absence. And absence doesn’t trigger funding, policy shifts, or prevention alerts. It just hides the truth.
Fewer Tests, Fewer Numbers, But Not Fewer Infections
Let’s get blunt: declining test numbers do not equal declining STD rates. In fact, in several U.S. states, reported STD cases dropped sharply during the early years of the COVID-19 pandemic, not because transmission stopped, but because testing plummeted by 40–50% in some regions.
Public health officials were clear: the dip was artificial. Clinics were closed. Supplies were redirected to COVID response. People were scared to visit health centers or didn’t want to risk being seen there. Testing deserts, areas with no accessible, affordable testing, widened. And even when clinics reopened, staffing shortages and appointment delays discouraged many from coming back.
Now, years later, we’re still playing catch-up. “We lost the thread,” said one sexual health nurse from Phoenix. “People fell off the testing routine, and some haven’t returned. That messes with our data. It messes with contact tracing. It messes with trust.”
Who’s Getting Missed, and Why It Matters
Under-testing doesn’t affect all communities equally. Here’s what the data and experience show:
Figure 2. Populations affected most by under-testing, with unique access and stigma challenges.
When these communities aren’t getting tested at recommended intervals, the public health picture gets skewed, and resources may not go where they're most needed. That’s how disparities worsen. And that's why convenient, private access to at-home STD test kits is more important than ever.
When You Feel Fine but Still Infect Someone
One of the most dangerous myths in sexual health is this: “If I had an STD, I’d know.” But over half of all STD cases, including chlamydia, gonorrhea, and even syphilis, present no symptoms at all, especially in early stages. That means someone can carry and transmit an infection for weeks or months before ever feeling anything wrong.
Take Andre, a 29-year-old chef who assumed his annual check-up covered everything. “I thought the regular blood work included STDs. It didn’t. I had no clue until my ex called, crying, because she tested positive for gonorrhea.” Andre later learned he’d had the infection for at least six weeks, without symptoms, without warning, and without testing.
Silent infections like Andre’s make data unreliable. They also delay care, increase complications like pelvic inflammatory disease (PID), and raise the odds of long-term transmission. Without proactive testing, especially in sexually active adults under 30, STDs become invisible, not because they’re rare, but because they’re ignored.
How COVID Broke the Testing Habit
The pandemic didn’t just strain hospitals, it broke people’s routines. That included routine STD testing. From 2020 through 2022, many clinics closed temporarily, reallocated staff to COVID testing, or paused walk-in appointments. Even as restrictions eased, a lingering fear of healthcare spaces kept many away.
Telehealth rose, but it didn’t fully replace in-person testing. Many providers couldn’t offer mailed kits. Others didn’t screen for STDs unless patients asked. And as people moved, lost insurance, or lost access to student health services, testing fell off the radar.
Now, as services stabilize, we’re still dealing with the aftershocks. The CDC’s 2024 STD Surveillance Report noted ongoing inconsistencies in state-level data, especially among younger adults and queer communities. The decline in testing wasn’t just temporary, it reshaped the way infections are counted and tracked.
Can At-Home Testing Close the Gap?
In a word: yes. But only if people know it's an option, and trust it.
At-home STD tests, like the ones offered at STD Test Kits, allow users to collect samples privately, on their own time, without judgment or waiting rooms. Some offer instant results (rapid tests); others use mail-in samples sent to certified labs. Accuracy varies depending on test type and infection window, but for many people, it's the best chance at detection.
Public health experts have begun advocating for wider distribution of these tests, especially in rural or underserved areas. One 2023 study found that offering free at-home tests to high-risk populations increased test uptake by 65% compared to clinic-only options. It’s not a full replacement for in-person care, but it’s a powerful bridge.
And for someone silently carrying an STD, it can mean the difference between unknowingly spreading infection, or finally getting answers.
What “Bad” Data Means for Public Health
Data drives decisions. But when the data is incomplete, when infections go unreported because tests never happen, health officials can’t respond accurately. That affects everything from budget allocations to school health policies to national STD prevention campaigns.
For example, a state with rising real-world infections but falling confirmed cases might see its funding cut, because on paper, it looks like things are improving. That means fewer outreach programs, less partner notification staffing, and no new testing centers.
Worse, bad data means no one rings the alarm bell when an outbreak begins. That’s what happened with congenital syphilis, a preventable infection passed from parent to infant. Testing drops led to missed prenatal screenings, and between 2019 and 2024, congenital syphilis cases more than doubled in several U.S. states.
This isn’t hypothetical. It’s the cost of invisible infections. And it’s a cost we’re already paying.

People are also reading: The Forgotten STD: Why No One Talks About Donovanosis (Until It’s Too Late)
When One Partner Doesn’t Test
Sabrina, 26, thought her situationship was exclusive. He said he was clean. He hadn’t tested, but “he looked healthy” and said he’d only been with one other person since his last relationship. Three months later, Sabrina tested positive for trichomoniasis. He ghosted. She was left managing the treatment, the shame, and the confusion. “I didn’t even know that was an STD,” she admitted. “I thought that was like a yeast infection or something.”
This is what happens when testing becomes optional in hookup culture, or assumed unnecessary in monogamy. Without clear testing norms between partners, infections slip through. Not maliciously. Not intentionally. Just silently. And people like Sabrina are left cleaning up the aftermath of someone else’s assumptions.
When a partner skips testing, their risk becomes your risk. That’s why mutual testing conversations, and accessible options, matter so much more than people think.
Stigma Still Stops People from Testing
Even in 2025, STD testing carries stigma. People worry about being judged, outed, or seen as “dirty.” Some still associate getting tested with being promiscuous. For men, especially straight men, there’s an added barrier: fear of being perceived as weak, sick, or reckless.
Studies have shown that emotional discomfort, shame, embarrassment, fear of the result, is a major reason people delay or avoid testing entirely. Add to that the fear of being seen at a clinic, a lack of privacy at home, or cultural taboos around sexuality, and it’s no wonder that many infections stay undetected.
This is where at-home testing can be a game changer. Private. Non-judgmental. Empowering. You don't need to explain yourself to anyone. You don't need permission. You just need the kit, the knowledge, and a few quiet minutes to protect your body and your partners.
Testing Timelines: When to Screen and When to Retest
If you’ve had unprotected sex, or even protected sex where a condom slipped, broke, or was removed, testing isn’t just “smart.” It’s necessary. But timing matters. Test too early, and you might get a false negative. Wait too long, and you might unknowingly spread something that could’ve been caught earlier.
Here’s a general guide:
Figure 3. Optimal STD testing windows. Use this chart to plan your next screening based on exposure timing.
If you’re unsure when to test, or if your exposure falls across multiple infection windows, a multi-panel option like the Combo STD Home Test Kit may be the best place to start. It covers multiple infections and is built for privacy, clarity, and ease.
FAQs
1. If fewer people are testing, does that mean STDs are going away?
Nope, quite the opposite. Fewer tests just mean we’re catching fewer infections on paper. The STDs are still out there; we’re just not counting them properly. It’s like turning off your smoke detector and saying the fire stopped.
2. Why would someone skip an STD test?
So many reasons. They feel fine. They’re embarrassed. Their partner said “we’re exclusive.” Or maybe they just don’t know where to go, or how awkward it might feel. But here’s the truth: testing isn’t a confession, it’s self-respect. And it’s easier than ever to do from home.
3. Can I have an STD and have no clue?
Absolutely. In fact, it’s more common than not. Infections like chlamydia and gonorrhea are often completely silent, especially in the early stages. You could be carrying and spreading something and never feel a single twinge. That’s why testing matters even when nothing seems “off.”
4. How often should I be getting tested?
If you’re sexually active, aim for once a year at minimum. But if you have new partners, multiple partners, or recently ditched condoms, go for every 3 to 6 months. Think of it like oil changes, but for your sex life.
5. Do at-home STD tests really work?
Yes, when used correctly and at the right time. Some give results in minutes; others require you to mail a sample to a lab. Either way, modern at-home kits can be just as accurate as clinic tests, without the awkward waiting room or paperwork.
6. What if my partner refuses to get tested?
That’s a red flag, plain and simple. Testing should be mutual, respectful, and non-negotiable, like wearing a seatbelt. If they push back, you get to push pause. Your body deserves better than uncertainty and crossed fingers.
7. I tested negative, do I need to retest?
It depends on when you tested. Every STD has a “window period”, a time between exposure and detectability. If you tested too soon after a hookup or scare, you might need to retest in a few weeks for full confidence. A negative today doesn’t always mean you’re totally clear tomorrow.
8. Will anyone find out I got tested?
Not if you don’t want them to. At-home kits ship in plain packaging and results stay private. Even lab-reported positives go to health departments stripped of your personal identity. You’re in control of who knows what.
9. Do I really need to test if I’ve only been with one person?
Here’s the tricky part: unless both of you tested at the beginning of your relationship, you’re both operating on faith, not facts. And faith doesn’t kill bacteria. If your last partner didn’t test either, there’s still a risk, even if everything feels safe.
10. Is it ever “too late” to test?
Never. Whether your exposure was last night or last year, knowing is always better than guessing. STDs don’t disappear just because we ignore them. Testing now could clear up symptoms you didn’t even connect, or protect a partner down the road.
You Deserve Answers, Not Assumptions
Skipping a test might feel like a small decision in the moment. But collectively, missed tests reshape public health, and not in a good way. They hide outbreaks. Delay treatment. Hurt communities. And leave people like Sabrina and Andre wondering what went wrong when the signs weren’t even there.
You don’t have to wait for symptoms. You don’t need to justify your choices. You just need information, and access. Start with a private, reliable option like the Combo STD Home Test Kit, which checks for multiple common infections in one go. The answers are closer than you think.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Sexually Transmitted Infections (STIs) Fact Sheet | WHO
2. Point-of-Care Testing for Sexually Transmitted Infections | PMC
3. Enhanced Surveillance of STIs to Foster Public Health | JAMA Network Open
4. STI Prevention and Testing Recommendations | CDC
5. STI Screening Recommendations | CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Dr. Lina Vo, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.






