Can You Go to Urgent Care for STD Testing?
Quick Answer: Female STD symptoms like discharge, itching, or pelvic pain are frequently dismissed by medical providers, especially when tests aren’t immediately ordered. This leads to delayed diagnosis, unnecessary complications, and loss of patient trust.
This Isn’t Just a UTI, And Here’s Why That Matters
Most STDs in women don’t start with the textbook symptoms we see in posters or sex-ed classes. There’s rarely a dramatic sore or full-body rash. Instead, symptoms are subtle, and often overlap with “everyday” conditions like yeast infections, UTIs, or hormonal shifts.
But just because something is common doesn’t mean it’s harmless. Here are real symptoms women report before being diagnosed with an STD:
- Itching or irritation without visible sores
- Thicker discharge or changes in smell
- Spotting after sex (often brushed off as “normal”)
- Pelvic pain or pressure mistaken for cramps
- Burning during urination that’s not from a UTI
The problem? These symptoms are easy to dismiss, by doctors and by patients. Many women are told it’s “just bacterial vaginosis” or “you’re probably overreacting.” That internalized doubt leads people to delay testing, downplay their concerns, or never seek care at all.
According to the CDC, up to 70% of women with Chlamydia show no noticeable symptoms, or mistake them for something else. Even symptomatic cases are often misdiagnosed due to overlapping signs with non-STI vaginal conditions.
This isn't rare. In fact, we heard dozens like hers while researching this piece. Women reporting itching, pain, discharge, or post-sex bleeding are often told:
- “It’s probably just yeast.”
- “You’re too young for cervical issues.”
- “That’s normal discharge. Nothing to worry about.”
- “You're being overly sensitive.”
When you hear those things over and over, especially from white coats, you start to question yourself. That’s the quiet trauma of medical gaslighting. It’s not just disbelief, it’s a subtle erosion of your body’s truth.
Keira says she now avoids in-person clinics unless absolutely necessary. “I trust my body more than I trust being told it’s ‘just a hygiene issue.’ I’ll pay out of pocket if I have to, just to know I’m being taken seriously.”
This erosion of trust doesn't just affect individuals, it hurts public health. People who don’t feel heard stop seeking care. And STDs don’t wait politely until someone feels ready, they spread silently.

People are also reading: No Clinic Nearby? Here’s How Rural Americans Are Testing for STDs Anyway
“You’re Fine”: The Gender Bias Hiding in Plain Sight
When women walk into a clinic complaining about vaginal pain, weird discharge, or burning during sex, there’s a decent chance the response won’t be, “Let’s test you for STDs.” Instead, it might be: “Are you stressed? Could it be hormones? Is your partner rough during sex?” In too many exam rooms, women's bodies are seen through the lens of exaggeration, not urgency.
And it's not just stories; there are real numbers to back it up. The Journal of the American Medical Association published a study in 2023 that found that women who went to the doctor with genital or pelvic problems were 33% less likely than men to be tested for STIs on their first visit. Let that sink in: different bodies, same symptoms, less care. And when women do finally get tested, it's often after a lot of appointments and having to prove they weren't lying.
That's what medical gaslighting looks like. It's not just a doctor with a bad attitude; it's a problem with the system. It starts in medical school, where textbooks often show male anatomy as the norm. It lives in how pain is charted (“vague discomfort” vs. “sharp localized pain”). It gets bigger when you think things like, "She's probably just here to feel better," or "It's probably just BV." What happened? Testing that was put off. Missed diagnoses. Complications that can be avoided. And a lot of people leaving appointments feeling like they weren't heard and ashamed.
This isn’t just frustrating, it’s dangerous. Untreated Chlamydia and Gonorrhea can lead to pelvic inflammatory disease (PID), a condition that can cause chronic pain, infertility, and increase risk of ectopic pregnancy. Herpes, when left undiagnosed, can be misattributed to things like shaving bumps or allergic reactions, delaying critical treatment and ongoing care.
And if you think the bias stops with cisgender women, think again. When you layer in race, sexuality, or gender identity, the gap in care grows wider. Black women are more likely to be diagnosed with an STD at a later stage, despite reporting symptoms earlier. Latina patients report feeling less heard when describing pain or vaginal concerns. Queer women are often told they’re “not at risk,” despite STI rates showing otherwise. Trans men and nonbinary people are frequently misgendered, misdiagnosed, or not tested at all because the provider is too uncomfortable, or uninformed, to offer full-panel care.
“They told me it was just hormones because I’m on testosterone,” said Devyn, 25, a transmasc patient who was eventually diagnosed with Gonorrhea after three separate visits. “I knew it wasn’t hormones. I was in pain.”
These aren’t rare stories. They're structural patterns. They reflect a system that was never built with female, queer, or trans bodies in mind. And they create a ripple effect: shame, fear, distrust, avoidance. If you’ve ever walked out of a clinic more confused than when you walked in, you’ve felt it. If you’ve ever gone home and Googled your symptoms at 2AM because your concerns were waved off, you’ve lived it.
Bias isn’t just a bad vibe, it’s a barrier to care. And it’s costing people their peace, their health, and sometimes, their future fertility.
Let’s talk about the elephant in the room: STD tests aren’t perfect. And for women especially, some STDs are harder to detect, or test for altogether.
For example, Herpes testing is notoriously murky. If you don’t have visible sores, many doctors won’t offer a blood test. And if they do, the results may come back as “equivocal”, a gray area that leaves patients more confused than comforted.
False negatives are also more common than many realize. Peer-reviewed research has shown that urine tests for Gonorrhea and Chlamydia in women can miss up to 20% of infections, especially if the swab wasn't taken vaginally. Add that to rushed appointments, poor technique, or outdated equipment, and you have a recipe for misdiagnosis, or no diagnosis at all.
Here are just a few ways the system fails women in STD detection:
- Testing refusals: “You don’t need a test unless you’re high-risk.”
- Limited panels: Some clinics don’t include herpes, trichomoniasis, or HPV in standard tests unless requested.
- Insurance barriers: Out-of-pocket tests can cost $200–$500 at labs.
- Asymptomatic infections: Especially with Chlamydia and HPV, women often have no noticeable signs until complications arise.
It's no wonder many women turn to at-home STD kits. Not because they don't trust medicine, but because they don’t trust being ignored.
Medical dismissal doesn’t just delay diagnosis, it rewires how we relate to our bodies. When you’re told “it’s nothing” over and over, you start believing it might be. For many women, especially those navigating symptoms like discharge, irritation, or pain during sex, that internal doubt becomes paralyzing.
Shame thrives in silence. And when you can’t get a straight answer, you might start blaming yourself. Was I overreacting? Did I clean wrong? Am I dirty? These thoughts don’t just reflect poor healthcare, they reflect the toxic way we’ve been conditioned to ignore or distrust female pain.
“I started questioning everything,” said Grace, 31, who was misdiagnosed with “stress-related vaginal pain” three times before getting a positive test for Trichomoniasis. “I felt crazy, like I was making it up for attention.”
She wasn’t. And neither are you.
How to Speak Up When Your Doctor Doesn’t Listen
You don’t have to be a medical expert to advocate for your health. But you do need tools, and permission, to push back. Here’s what that can look like:
- Ask directly: “Can we test for STDs today, including herpes and trichomoniasis?”
- Clarify refusal: “Can you note in my chart that I requested testing and it was declined?”
- Get specific: “I’m not sexually active now, but I was three months ago. Please don’t assume I’m low risk.”
- Reframe ‘normal’: “This discharge isn’t normal for me, even if it’s common.”
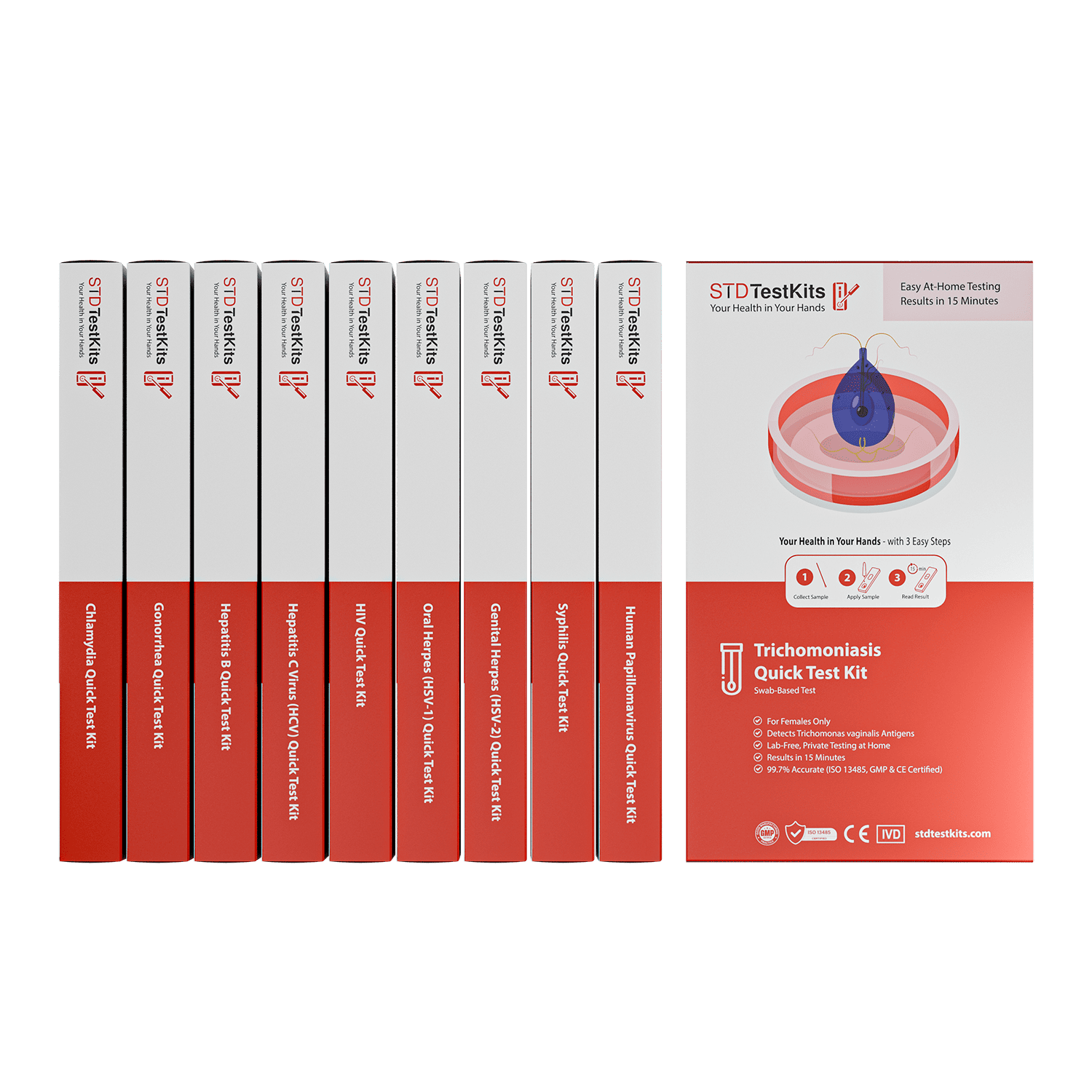
If the provider still won’t listen, get a second opinion, or take matters into your own hands with an 8‑in‑1 Complete At-Home STD Test Kit.
At-home testing isn't about skipping the doctor, it's about reclaiming your body’s truth when no one else will.
You’re Not Being Dramatic, You’re Being Dismissed
Too often, women are taught to minimize discomfort. To endure. To protect others from the inconvenience of their needs. That conditioning doesn’t disappear in a clinic, it shows up when we say things like:
- “Sorry, this is probably nothing…”
- “I know it’s TMI but…”
- “I hate to bother you, but…”
It’s not “bothering” to want answers. It’s not “too much” to advocate for clarity. Your body deserves attention, not apology. And if a doctor doesn’t see that? They’re the problem, not you.
Your story, your symptoms, and your intuition matter.

People are also reading: Condoms Cover Genitals, Not Everything Else: The Skin-to-Skin STD Problem
FAQs
1. Can I have an STD even if there’s no weird smell or discharge?
Totally. STDs aren’t always loud. In fact, a lot of them are subtle, or straight-up silent. You might just feel “off” down there. Trust that.
2. My doctor said it’s probably yeast. Should I push for testing anyway?
If your gut says yes, yes. Yeast infections are common, but so is mistaking herpes, BV, or trich for yeast. If something doesn’t feel right, you have every right to ask for a swab or a second opinion.
3. Is it normal to feel embarrassed asking for an STD test?
Unfortunately, yes, and that sucks. But getting tested is literally one of the most protective, badass things you can do for yourself (and your partners). Testing ≠ shame. It means you care.
4. Why do some clinics refuse to test for herpes?
Because the system is flawed. Many doctors won’t test unless you have visible sores, even though type-specific blood tests exist. You can absolutely ask for one, or use an at-home kit that includes it.
5. I got tested, but everything came back negative... and I still feel off?
You’re not crazy. False negatives are real, especially with early infections or the wrong kind of sample. If symptoms stick around, retest in a few weeks, or try a more comprehensive panel.
6. Can I get an STD from someone who has no symptoms?
Yep. A lot of STDs spread when people don’t know they’re infected. That’s why waiting for your partner to “look sick” or “say something” isn’t a solid plan. Protect yourself regardless.
7. Do at-home STD tests actually work?
Yes, as long as you use a reputable brand. Look for FDA-cleared or lab-validated options like the ones right here. They’re discreet, fast, and accurate when you follow instructions.
8. Can I really ask my doctor to document if they refuse testing?
100%. You can say, “Please note in my file that I requested an STD panel and it was denied.” That one line can shift the dynamic, and remind them you're not just a passive patient.
9. Is spotting after sex always a red flag?
Not always, but it’s not something to ignore either. It could be irritation, hormonal shifts, or something like Chlamydia or HPV. If it keeps happening, get checked out. Your body’s not trying to inconvenience you, it’s communicating.
10. What if I’ve been gaslit before and don’t trust doctors now?
That’s valid. Medical trauma is real. Start by testing in ways that feel safe, like at home. And know this: you are not dramatic. You are not dirty. You are not overreacting. You’re advocating for the body you live in every damn day. That’s brave.
You Deserve Answers, Not Assumptions
If you’ve ever been dismissed, doubted, or gaslit about your symptoms, you are not alone. This isn’t about being dramatic. It’s about getting the care you deserve. It’s about knowing when something’s off, even if a provider won’t listen.
Whether you’re dealing with itching, burning, weird discharge, or just that gut feeling that something isn’t right, you don’t have to wait for permission to take action.
Testing is care. Testing is clarity. Testing is how you stop the guessing game and start protecting your health.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
Sources
1. Provider disbelief and pain dismissal among women with chronic pelvic issues – PMC
2. Gaslighting in women's health: Misdiagnosis & dismissal trends – Northwell Katz Institute
3. Female doctors-turned-patients describe how their symptoms were dismissed – WebMD
4. Gendered pain: chronic pain more common in women, yet their pain is often minimized – PMC
5. Gender bias in medical diagnosis – Wikipedia (systemic skepticism toward women’s symptoms)
6. Women delay seeking STD care, thinking symptoms are “normal” or not STD-related – PMC