The STDs Dentists Spot First, Before You Even Feel Sick
Quick Answer: Yes, you can absolutely get an STD from oral sex, even if it’s your only form of sexual contact. Infections like chlamydia, gonorrhea, herpes, syphilis, HPV, and even HIV can be passed through oral-genital or oral-anal contact.
This Feels Safer, So Why Are People Still Getting Infected?
Oral sex is often seen as the “safe” alternative to penetrative sex. It’s talked about casually in locker rooms, whispered about at sleepovers, and even sometimes excluded from conversations around virginity. But here’s the uncomfortable truth: just because it feels less intimate or risky doesn’t mean it’s medically safe.
Unlike vaginal or anal sex, oral sex doesn’t always leave obvious signs of transmission. There’s no broken condom, no discomfort during the act, and often, no symptoms afterwards. That creates a dangerous illusion of immunity, especially among young people and partners who assume monogamy equals protection. But STDs don’t care about the technicalities of “what counts” as sex. If there's mouth-to-genital or mouth-to-anus contact, there’s risk.
And it's not theoretical. Studies show rising rates of gonorrhea in the throat, and researchers have identified oral herpes as one of the most underdiagnosed routes of transmission. You can’t taste an infection. You can’t feel one being passed. And for many STDs, your partner might not even know they’re carrying it.
The Infections That Love to Hide in Your Mouth
Most people don’t think of the mouth as a high-risk zone. But it’s actually a prime environment for bacterial and viral STDs. Warm, moist, full of mucous membranes, basically the same qualities that make genitals vulnerable.
Here’s how some of the most common STDs can be transmitted through oral sex, and what they tend to look like (or not look like) when they land in your throat or mouth:
Table 1. Common STDs that can be transmitted through oral sex, including likelihood of symptoms in the mouth or throat.
Here’s what most people don’t realize: chlamydia in the throat rarely causes pain. Oral gonorrhea might feel like a seasonal allergy. HPV might never show until a dentist spots abnormal tissue years later. That’s why routine testing is crucial, even if you feel totally fine.
People are also reading: Safe Sex Isn’t Just for the Young: Seniors and STI Prevention
“But I Didn’t Swallow!” , Why Fluids Aren’t the Only Risk
Many readers believe that if they don’t swallow ejaculate or vaginal fluids, they’ve sidestepped the risk. This is a dangerous half-truth. STDs are spread through contact, not just fluid exchange. That means skin-to-skin transmission, contact with pre-ejaculate, or even exposure to viral shedding on the genitals.
Take herpes, for example. It doesn’t require visible sores to transmit. The virus can shed even when someone feels completely normal. If a partner has HSV-2 on the genitals and receives oral sex, there’s a real possibility the giver could contract the virus, especially if they have micro-abrasions or gum irritation in their mouth.
Or consider syphilis, which often presents with a single, painless sore that can appear on the lip, inside the cheek, or on the tonsils. That sore is highly infectious. The person may not notice it, or may confuse it for a canker sore or bite injury, yet it’s enough to transmit the disease to a partner during a brief oral encounter.
Here’s a scenario we hear all too often: someone meets a new partner. They’re not ready for penetrative sex, but they’re open to oral. There’s no condom. There’s no discussion of testing. And weeks later, something doesn’t feel right. A sore throat. A lesion. A worry. That’s how it happens, quietly, and without drama.
Why Testing Often Misses Oral Infections
Most people who get tested for STDs don’t realize their throat needs its own swab. That’s not a mistake, they’re just following default clinic protocol. The problem is, if you only provide a urine sample or genital swab, you’re not checking the mouth or rectum. And many clinics won’t test those sites unless you specifically ask for them.
Let’s say you have throat gonorrhea. You feel nothing, but you carry the bacteria. You get a clean bill of health from a standard genital screening, and assume you're STD-free. Then you give oral sex to a partner. You pass the infection along, unknowingly. Now they have a new infection, and neither of you knows where it came from. This cycle is incredibly common, and it’s a key driver of reinfection and frustration, especially in long-term couples.
This is why many health experts recommend site-specific screening. If you’ve given or received oral sex, your throat deserves testing, especially if your only protection has been “pulling out” or abstaining from full intercourse.
Table 2. Common testing sites and the infections they detect. Many people are never tested at all relevant sites unless they ask directly.
This matters. If you’re only testing where you feel symptoms, or where you think risk occurred, you might be missing the full picture. Oral infections are real, they’re transmissible, and they deserve screening just like any other part of your body.
Why You Might Not Know You’re Infectious
It’s terrifying to think you could give someone an STD without knowing you had one. But it happens all the time. Let’s break down why.
First, many STDs have incubation periods, a span of days or weeks between exposure and detectability. During this time, you may have zero symptoms. You may even test negative. But that doesn’t mean the infection isn’t there. It just means it hasn’t built up enough to trigger a positive result yet.
Second, even after that window period, you might carry an oral STD with no obvious symptoms. Throat gonorrhea, for example, is almost always silent. So is oral chlamydia. People may have no idea they’re infected for months, until they test for a different reason, or a partner develops symptoms.
Here’s a quick visual on how this plays out in real life:
Table 3. How a silent oral STD can spread even with a negative test result, because site-specific swabs were missed.
This kind of story happens more than we like to admit. It’s not about recklessness. It’s about gaps in testing and a false sense of safety.
If You’re Worried, Here’s What You Can Do Now
The good news? You don’t have to wait for symptoms to protect yourself, or your partners. At-home test kits now offer mouth-specific swabs, and they ship discreetly so you can test without leaving your house. These kits are easy to use and can detect multiple infections, including gonorrhea and chlamydia, from the throat.
If you're wondering whether what happened last weekend “counts” as risk, the answer is yes, it might. And whether it’s been a week or a year since your last test, you deserve clarity. Knowing your status isn’t about shame or fear. It’s about confidence, intimacy, and protecting the people you care about.
This at-home combo test kit screens for the most common infections and includes easy instructions for collection and use. It’s fast, private, and doctor-trusted.
If your head keeps spinning, peace of mind is one test away. You don’t need permission. You just need the right information and the tools to act.
What If the Test Comes Back Positive?
Finding out you’ve tested positive for an STD you didn’t even know could live in your throat can feel like a punch to the gut. But take a breath. Most STDs are treatable, and oral infections often clear faster with medication than genital ones. This isn’t a life sentence, it’s a starting point.
If you test positive for something like throat gonorrhea or chlamydia, your provider will likely prescribe a round of antibiotics. It’s important to take the full course, even if you feel fine. And yes, you’ll want to let recent partners know so they can get tested too. That’s not always an easy conversation, but anonymous text tools, telehealth scripts, and clinic support can make it easier. You’re not alone in this.
Here’s what often happens next: someone panics, googles nonstop, and spirals into shame. But within 48 hours, they’ve talked to a nurse, taken a pill, and started to feel empowered again. You can get there, too.
If your positive result came from an at-home test, some kits offer telehealth support to confirm results and prescribe treatment. If not, you can bring your result to a local clinic and request care. The most important thing? Don’t ghost the process. Treating oral STDs early can prevent complications like reinfection, systemic symptoms, and, very rarely, long-term damage.
People are also reading: White Discharge, Itching, No STD? It Might Not Be What You Think
“We Didn’t Think We Needed to Test for That”
When Sam and Javi started dating, they agreed on testing before going all the way. “We wanted to do it right,” Sam said. “No sex until we were both cleared.” They both got tested, urine samples, blood work, clinic visit. Everything came back negative. They breathed easy and got closer. But a few months in, Javi developed a sore at the back of his tongue. His dentist flagged it, and a follow-up test revealed syphilis.
Sam was confused. “We never had penetrative sex. Just oral. How could this happen?”
Turns out, Sam’s test didn’t include an oral swab. And Javi’s initial panel didn’t include a syphilis antibody check. Both were told they were negative, yet neither had been tested for the thing they actually transmitted.
This happens more often than you’d expect. Many testing panels are built around assumptions: that people are heterosexual, that vaginal or anal sex is the primary risk, and that symptoms will appear if something’s wrong. None of those assumptions hold up under scrutiny, especially for queer couples, casual partners, or anyone whose sex life involves mouths, fingers, or toys.
Oral sex isn’t an afterthought. It’s sex. And it deserves testing protocols that match its reality.
How Long Should You Wait Before Testing After Oral Sex?
If you had oral sex recently and you're wondering when to get tested, here's the short version: don’t rush. It takes time for most STDs to incubate and become detectable by tests. Testing too early can produce a false negative, and give you a false sense of safety.
Most experts recommend waiting 7 to 14 days after a potential exposure before testing for chlamydia, gonorrhea, or syphilis in the throat. For herpes, it depends on whether you’re testing by swab (which requires an active sore) or blood (which detects antibodies formed after infection). For HIV, a throat exposure is lower risk, but if you're worried, wait two to four weeks before testing, with a follow-up at 12 weeks to confirm.
Here’s the part nobody tells you: even if you test negative at the “right” time, some cases require a retest. Why? Because STDs don’t always behave on schedule. If you test on day 10 and it’s negative, but you still feel “off” by day 25, get checked again. The test doesn’t lie, but it can only see what’s there in the moment.
This is why at-home kits with repeat access or clinics that support follow-up care are essential. You need flexibility, not a one-shot deal. You need throat swabs, not just genital panels. You need tests that match your life, not someone else’s assumptions.
Read our guide on when to test after exposure to understand timing by infection type, testing method, and symptom status.
Your Mouth Deserves the Same Care as the Rest of You
The hardest part of oral sex and STD risk isn’t the science, it’s the silence. The way we downplay “just oral,” the way we skip protection, the way we accept partial testing panels as good enough. But your mouth, your health, and your relationships deserve more than guesswork. They deserve care. Full-spectrum, shame-free, clear-eyed care.
You don’t need to feel sick to get tested. You don’t need to wait for your partner to bring it up. And you don’t need a clinic visit to take action. You just need information, and a test that sees what standard screenings miss.
Explore at-home test kits built for the real world, not outdated assumptions. Privacy, accuracy, and peace of mind, all in your hands.
FAQs
1. Can you really get chlamydia in your throat?
Yep, wild, right? Chlamydia doesn’t just hang out in genitals. If you give oral sex to someone who’s carrying it, that bacteria can set up camp in your throat. The tricky part? You might never feel a thing. No sore throat, no fever, nothing. That’s why a lot of people walk around with oral chlamydia and don’t know it until a partner tests positive.
2. Is herpes from oral sex more common than people think?
Oh, 100%. Herpes doesn’t care how “mild” or “clean” the sex felt. If your partner has oral herpes (cold sores) and goes down on you, that can transmit to your genitals. And vice versa: if they have genital herpes and you give them oral? It can show up in your mouth. Most people spreading herpes have no clue they’re doing it because they’re asymptomatic or between outbreaks.
3. Can you pass an STD even if you didn’t swallow?
Absolutely. This one trips people up. Fluids aren’t the only thing that carry infections, skin-to-skin contact, pre-cum, and even viral shedding can be enough. Herpes? Doesn’t need penetration. Syphilis? One small sore in the mouth is enough. It’s not about “swallowing or not”, it’s about exposure. So yeah, still a risk.
4. Is it possible to get HIV from oral sex?
It’s rare, but possible. Especially if there are open sores, bleeding gums, or untreated cavities in the mouth, and if your partner has a high viral load and isn’t on meds. It’s not the top risk behavior for HIV, but if you’re worried after a high-risk exposure, it’s totally legit to get tested and talk to a provider. Better to ask than assume.
5. How can I test for throat STDs at home?
Easy. Some at-home kits now come with special throat swabs made just for this. You swab the back of your throat (think COVID test vibes), seal it, and send it off. No awkward doctor visit, no guessing. Just make sure the kit you're using explicitly says it tests “extra-genital” or “oral” samples, otherwise, you might only be testing down south.
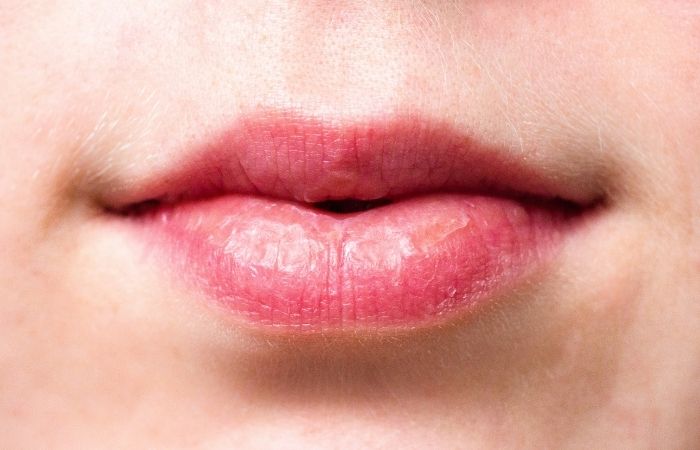
6. What does an oral STD sore look like?
Depends on the infection. Herpes might look like a cold sore, blistery, crusty, maybe painful. Syphilis usually shows up as a single, painless ulcer or sore (that often gets mistaken for a bite or canker sore). HPV? You may not see anything at all, but sometimes small, flesh-colored bumps pop up. If you notice something weird that wasn’t there last week, get it checked. Better awkward than untreated.
7. Should I use protection during oral sex?
Honestly? It's smart. Dental dams, flavored condoms, even unlubricated ones, any barrier helps cut risk. Most people don’t use them, but that doesn’t mean you can’t. If you’re nervous about taste or sensation, try experimenting solo or with a partner before the moment hits. Normalize it, make it part of the fun, and know you're protecting both of you.
8. Can I reinfect my partner after treatment?
Unfortunately, yes. Let’s say you get treated, but your partner doesn’t, or doesn’t finish their meds. You hook up again, and bam, right back where you started. That’s why it’s crucial that both (or all) partners get treated and wait the recommended time before getting sexy again. Nobody likes a loop of “I thought we were clear” moments.
9. How often should I test if I only have oral sex?
Great question. If oral sex is your main move, testing is still important, especially for gonorrhea, chlamydia, and syphilis. How often? That depends on your partners and protection use. Once or twice a year for monogamous folks; every 3 to 6 months if you're more active or non-monogamous. Don’t downplay it just because it’s “not real sex.” Your body knows better.
10. Does throat gonorrhea go away on its own?
Technically, sometimes. But relying on that is a bad plan. Untreated throat gonorrhea can linger and spread, plus it can develop resistance to meds over time. If you’ve tested positive, don’t wait it out. Get the treatment. Clear it up. Protect your future self and anyone you’re getting intimate with.
You Deserve Answers, Not Assumptions
Oral sex might feel low-risk, but the science says otherwise. Infections don’t care whether you used protection, swallowed, or just “did it once.” They care about contact. And contact is enough.
Testing isn’t about punishment or paranoia, it’s about respect. For yourself, for your health, for the people you love. Whether you’re experiencing symptoms or just asking “what if,” your body deserves the clarity only a test can provide.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. About STI Risk and Oral Sex — CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Natalia Vega, MSN, FNP-BC | Last medically reviewed: October 2025
This article is just for information and should not be used as medical advice.







