Can You Get an STD from Hands Alone?
Quick Answer: Virginity doesn’t guarantee safety from STDs. Infections like herpes, HPV, and chlamydia can spread through oral sex, skin contact, or shared objects, even without intercourse.
Who This Article Is For (And Why the Confusion Hurts)
This guide is for anyone who’s been told that “virgins don’t need to worry,” or that STDs only happen to people who’ve had “real sex.” It’s for teens having oral sex in secret but thinking they’re staying safe, for queer folks whose intimacy doesn’t involve penetration, for people in religious communities who’ve been taught that abstinence is protection, and for anyone whose body is telling them something is wrong, even when their label says otherwise.
The myth of virgin immunity creates shame, confusion, and missed diagnoses. People delay testing because they believe they’re low risk. They miss early treatment windows. They don’t tell partners because “it couldn’t be that.” But STDs don’t wait for definitions. They follow biology, not belief. And testing? That’s not a confession. It’s care. This article will break down how STDs can happen without intercourse, what counts as risky contact, when to test, and what to do next if you’re scared, confused, or already seeing symptoms.

People are also reading: Hookup Regret or Real Risk? When to Test After Drunk Sex
Why ‘Virginity’ Doesn’t Equal STD Immunity
The word “virgin” carries more weight than science. In medicine, there’s no universal definition. Some people think of virginity as “penis-in-vagina” intercourse. Others include anal or oral sex. Many queer people have intimacy that never includes penetration at all. And none of that changes your body’s ability to transmit, or contract, an infection.
STDs aren’t tied to the word “sex.” They’re tied to exposure: skin, fluids, and mucous membranes. You can get herpes from kissing. You can get HPV from skin-to-skin rubbing. You can get chlamydia from oral sex. And if your partner had a previous infection they never knew about, or picked up something non-sexually in childhood like oral herpes, it can still be passed even if neither of you has ever “gone all the way.”
One study published in the American Journal of Obstetrics & Gynecology found that 1 in 4 girls who reported never having had vaginal sex still tested positive for HPV. Virginity, in other words, isn’t a diagnosis. It’s a social idea. And it’s often misleading when it comes to your actual risk.
“We Were Both Virgins. But I Got Chlamydia.”
Jared, 21, and his girlfriend had waited. No intercourse. No penetration. But they had experimented with oral and mutual masturbation. A month later, she started experiencing burning when she peed. “We were both supposed to be clean,” Jared said. “We were each other’s first. So I didn’t understand how this was even possible.” A urine test confirmed chlamydia.
“It messed with my head,” Jared recalls. “I didn’t cheat. She didn’t cheat. But the doctor said oral sex was enough.”
Chlamydia can infect the throat and then pass to the genitals during oral sex, or vice versa. And because most people with chlamydia have zero symptoms, it’s easy to carry unknowingly. The virus doesn’t need ejaculation. It doesn’t need vaginal sex. It just needs mucous membranes. And in Jared’s case, that was enough.
What Experts Actually Look For (Hint: It’s Not the ‘V’ Word)
When clinicians assess STD risk, they don’t ask, “Are you a virgin?” They ask:
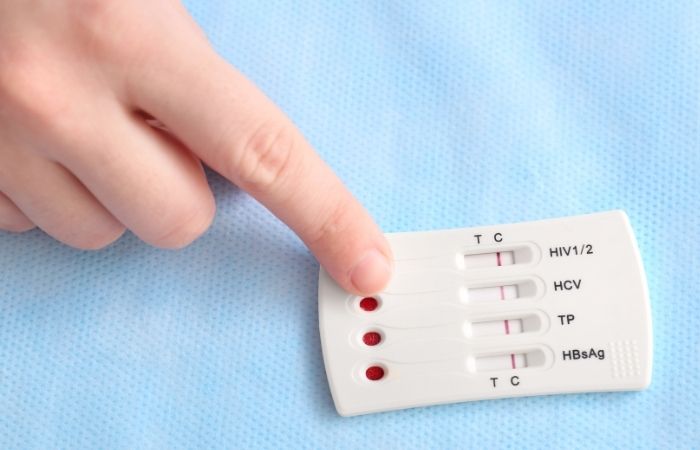
Figure 1. Risk factors clinicians assess regardless of “virgin” status
Medical risk isn’t about a binary label, it’s about exposure. And if your body’s had any of these contacts, it’s worth having a real conversation about testing, especially if you’re experiencing symptoms or starting a new relationship.
The Biggest Myth: “If You’re Both Virgins, There’s No Way”
This is the myth that does the most damage. The assumption is: if neither person has had penetrative sex before, there's no possible STD risk. But this relies on an extremely narrow definition of sex, and an even more flawed idea of how STDs work.
In real life, many STDs are transmitted in ways that don’t require intercourse at all. A partner may have been exposed through non-sexual childhood contact with herpes (HSV-1), or had oral sex with a previous partner and carried gonorrhea in the throat unknowingly. If that partner now gives oral sex to someone else, even if both believe they’re “still virgins”, the infection can be passed on.
The CDC notes that herpes can be transmitted from skin not covered by condoms, and that HPV spreads through skin-to-skin contact even without penetration. Virginity, again, does not offer immunity. Biology doesn’t care what language you use to define your past.
STDs That Don’t Need Intercourse to Spread
Some infections are more efficient than others. But several high-prevalence STDs don’t need “sex” to get in.
Figure 2. Common STDs that don’t require penetration for transmission
This means two people who believe they’re “safe” because they haven’t had traditional sex may still unknowingly pass infections, especially if neither has been tested. And since many infections show no symptoms, they may never realize it.
Should You Get Tested If You’re a Virgin?
Short answer: yes, if you’ve had any form of intimate contact, or if you’re starting a new relationship and want to be sure. Planned Parenthood emphasizes that testing is based on behavior, not identity. So if you’ve ever received or given oral sex, kissed someone with cold sores, shared toys, or had genital contact, testing can still be medically appropriate.
Even if your only partner is also a “virgin,” if either of you has had oral sex in the past or prolonged skin contact, there’s still potential exposure. Remember, you’re not being paranoid, you’re being practical. Testing doesn’t mean you don’t trust your partner. It means you care about each other’s health.
And if you're ready to take the next step but feel nervous about going to a clinic, you don’t have to. You can test from home with discreet kits designed to check for chlamydia, gonorrhea, herpes, and more. STD Test Kits offers a range of at-home options that are fast, private, and FDA-approved.
When to Test: Timing Still Matters (Even for Non-Penetrative Exposure)
Just like with traditional exposures, testing too early after a new contact can result in a false negative. The window period, the time between exposure and when a test can reliably detect infection, still applies.
Here’s a general guide for testing after non-intercourse exposures like oral sex, genital rubbing, or shared toys:
- Chlamydia & Gonorrhea: 7 to 14 days after contact
- HSV (Herpes): 3 to 12 days for symptoms to show; antibody tests may take weeks
- HPV: Often asymptomatic; only detected through pap/visual exam or HPV testing (for cervix)
- Syphilis: 3 to 6 weeks post-exposure
If you test early and results are negative, consider retesting after the full window period, especially if symptoms appear, or if you plan to become sexually active with that partner in new ways. Accuracy increases over time.
Confused about what type of test you need or when to use it? This combo STD home test kit screens for multiple infections and can provide peace of mind before a first sexual experience.
What About Oral Sex, Kissing, and Toys?
They count, more than people think. In fact, oral sex is one of the most underrecognized routes of transmission for STDs like chlamydia, gonorrhea, syphilis, and herpes. If you’ve ever received or given oral sex, even without penetration, you could be at risk. The CDC has documented cases of teens acquiring STDs solely through oral contact.
Kissing isn’t entirely innocent either. HSV-1 (oral herpes) is commonly transmitted through kissing, even if cold sores aren’t visible. According to the WHO, nearly 3.7 billion people under age 50 carry oral herpes globally, and it often starts young, sometimes before any “sexual” contact occurs at all.
And shared toys? If unwashed or used between partners without condoms, they can carry bacteria or viruses from one person to another. Herpes, HPV, and even HIV (in rare cases) have been traced to contaminated objects. This is why condoms on toys, cleaning between use, and keeping personal items separate matters, no matter how “low risk” you think the act was.
Why Many People Don’t Know They Have an STD
Part of the problem is silence. But part of it is biological. Many STDs don’t show symptoms right away, or ever. According to the CDC, 75% of women and 50% of men with chlamydia show no symptoms. Herpes can lie dormant for months or years. HPV often clears on its own but can still be passed in the meantime.
This creates a cycle: someone believes they’re uninfected because they feel fine. They engage in intimate contact. They pass an infection unknowingly. Their partner also feels fine. Then one of them develops symptoms, or gets tested for a routine reason, and suddenly the question of “how?” emerges. Virginity, in this model, offers no answers.
This is why routine testing matters. Not because it’s about shame. But because most people who transmit STDs genuinely don’t know they have one. And if no one ever told you oral sex could do it, or that herpes doesn’t always show up as “obvious blisters,” you wouldn’t think to test. That’s not your fault. But now you know.
“We Thought Testing Was Only for ‘Real’ Sex”
Nicole, 20, and her college girlfriend had been together for almost a year. Neither had ever had penetrative sex. But they’d had oral sex, shared toys, and lots of skin contact. “We both said we were virgins,” Nicole remembers. “We thought that meant we were safe.”
During a routine exam, Nicole’s doctor offered a panel. “I almost said no,” she says. “I didn’t think I needed it.” But when the results came back, Nicole tested positive for gonorrhea. Her partner did, too.
“It was terrifying at first,” she says. “But the doctor explained how it can live in the throat and be passed through oral. No one ever told us that. Not in sex ed, not online, not anywhere.”
The couple treated their infections easily with antibiotics. But the emotional fallout lingered. “We didn’t cheat. We weren’t lying. But we were ignorant. And that’s what hurt the most. We thought we were doing everything right.”
How to Protect Yourself, Even If You’re Not Having Sex
You don’t need to be sexually active in the traditional sense to take your health seriously. Here’s how to protect yourself no matter where you fall on the spectrum of experience:
- Use protection during oral and toy play. Dental dams and condoms aren’t just for intercourse.
- Get tested before a new partner, even if no one has had “sex.” History matters. So does honesty.
- Clean toys, hands, and surfaces between partners or uses. Bacteria doesn’t care who used it last.
- Watch for symptoms, but don’t rely on them. Many STDs stay silent.
- Normalize talking about status and past exposure. Shame thrives in silence. But prevention lives in honesty.
And remember: you can always test at home. No appointments. No waiting rooms. Just clarity. This herpes rapid test detects antibodies from a simple blood sample and gives results within minutes. Or explore combo kits if you want broader screening.
Testing Is Self-Respect, Not a Confession
One of the most dangerous beliefs about STD testing is that it’s something to be ashamed of. That it “says something” about you. That it means you’ve done something wrong. That’s a lie, one baked into sex-negative culture, harmful abstinence-only education, and silence between generations.
The truth? Testing is one of the most responsible, protective things you can do for yourself and your partners, no matter what you have or haven’t done. Whether you’ve kissed one person or a dozen. Whether you’ve had intercourse or only oral. Whether you feel safe or scared. Testing is power. It’s proof that you care. It’s preparation, not punishment.
If you’re questioning your risk, wondering about symptoms, or simply want to start your next relationship with clarity, there’s a test for that. You don’t need a doctor’s permission to protect your health. You just need the facts, and a test that works for you.
FAQs
1. Can I really get an STD if I’ve never had sex?
Totally. If by “sex” you mean penis-in-vagina intercourse, your body still doesn’t care about that definition. Herpes, HPV, and even gonorrhea can spread through oral sex, deep kissing, or skin-on-skin grinding. You don’t need to “go all the way” to get all the risk.
2. Okay, but what if we’re both virgins?
Even then, it’s not a free pass. Maybe one of you got oral from an ex, or had cold sores growing up (that’s oral herpes, by the way). Maybe you’ve been rubbing genitals together or sharing toys. STDs don’t wait for a punch card to fill up, they just need a way in.
3. How would I even know if I had something?
Honestly, a lot of people don’t. That’s the trap. Most STDs don’t scream their arrival. You might feel fine, and still be carrying something like chlamydia or HPV. Or you could get a sore throat after oral sex and think it’s allergies when it’s gonorrhea in your throat.
4. Does oral sex really count?
It counts. Ask anyone who tested positive for gonorrhea or syphilis after a hookup that “didn’t really count.” Your mouth has mucous membranes, and those are prime entry points for a bunch of STDs. Plus, if your partner has something in their throat? It goes both ways.
5. Can I get herpes from kissing?
Yup, especially if someone has oral herpes (HSV-1). Cold sores aren’t just cosmetic. They’re contagious. Even without visible blisters, the virus can shed and spread. And once you’ve got it, it’s yours for life.
6. What’s the deal with toys, is that actually risky?
If you’re using the same toy with different people (or even the same partner but without cleaning it), then yes, it can pass infections. Herpes and HPV can live on surfaces. Wrap that thing in a condom or wash it between uses like your health depends on it. (Because it kinda does.)
7. I don’t have symptoms. Should I still test?
Yes. No symptoms ≠ no infection. Think of testing like brushing your teeth. You don’t wait for cavities to start brushing, right? Testing is maintenance. It’s how you stay ahead of the stuff you can’t see or feel, yet.
8. What if I get a positive result and I’ve never had “real” sex?
First off, you’re not alone. This happens more than people think. Take a breath. You didn’t do anything wrong. The virus didn’t ask for your definition of virginity before it made itself at home. What matters now is getting treated and protecting your future self.
9. How do I ask my partner to get tested without it sounding shady?
Try this: “I care about both of us and I just want us to start on the same page. Let’s get tested together so we both know what’s up.” It’s not a test of trust, it’s an act of respect. And if they push back? That’s a red flag, not a conversation.
10. Is it overkill to test before anything even happens?
Not at all. In fact, that’s smart as hell. If you’re thinking about having sex, or even just getting more intimate, testing clears the fog. No guesswork, no guilt, just facts. You don’t wait to wear a seatbelt until the crash. Same deal here.
You Deserve Answers, Not Assumptions
If you’ve been told you’re too “inexperienced” to need an STD test, that you’re “safe” just because you haven’t had sex, or that you’d somehow “know” if something was wrong, forget all of that. The only way to truly know your status is to get tested. Not because you’re guilty. Because you’re empowered.
Your body is worth protecting. Your peace of mind is worth securing. And your experience, whatever it has or hasn’t included, doesn’t disqualify you from care. A combo at-home test kit checks for common infections discreetly and quickly, no judgment, no clinic, no guesswork.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
2. About Sexually Transmitted Infections (STIs) – CDC
3. About Genital HPV Infection – CDC
4. STI Risk with Oral Sex – CDC
5. How STIs Spread – CDC (oral/anal/vaginal and skin contact)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: R. Chen, MPH | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.







