When the STD Test Says “Negative” But Your Body Says “Something’s Wrong”
Quick Answer: If you were too drunk to remember what happened, test for STDs no earlier than 7 days after exposure, and again at 14–30 days for best accuracy. If you're unsure when (or if) sex occurred, use 14 days as your reference point.
Who This Guide Is For (And Why It Matters)
Anyone who’s ever woken up anxious after a night out. People who feel too embarrassed to ask a partner what happened. Anyone whose memory is hazy, but whose gut says “I should probably test.” This is especially for those who aren’t sure what kind of sex (if any) took place, and don’t know where to begin.
You don’t need a full memory to take care of your health. Whether you blacked out, browned out, or just don’t have the details, the risk doesn’t disappear because the memory did. But panic isn’t the same as risk either. That’s why this guide walks you through real testing timelines, symptoms that matter (and don’t), and how to take action when you're unsure what happened.
Testing is care, not confession. It’s one of the most powerful things you can do after a blurry night, not because it changes the past, but because it gives you clarity for what’s next.

People are also reading: Yes, You Can Get Herpes Without Sex,Here’s How It Happens
What Actually Counts as an STD Test?
Let’s get one thing clear: not all tests are the same. If you walk into urgent care after a risky hookup, you might get tested for chlamydia and gonorrhea with a urine or vaginal swab, maybe HIV with a blood test. But they won’t always check for herpes, syphilis, or trichomoniasis unless you ask or have symptoms.
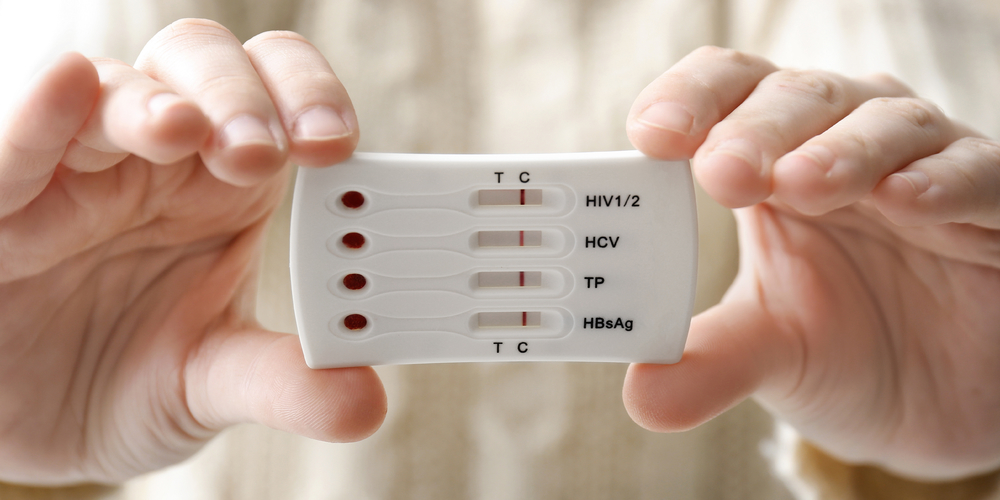
At-home STD tests can fill those gaps, offering panels that cover the most common infections, often with just a fingerprick or urine sample. The science behind them includes NAAT (nucleic acid amplification tests), which detect the actual DNA of an infection (like chlamydia), and rapid antigen or antibody tests, like those used for HIV or syphilis.
If you don’t remember what kind of sex occurred, oral, vaginal, anal, go broad. Choose a test panel that screens for multiple STDs. You can explore full panels at STD Test Kits.
Window Periods: What to Know When You Can’t Remember the Date
STD testing isn’t instant. Every infection has a “window period”, the time between exposure and when a test can actually detect it. Testing too early might give you a false sense of safety. But here’s the thing: if you were drunk, you might not know the exact time of exposure. That’s okay. You can still use general timelines.
Figure 1. Window periods after potential exposure. If you're unsure what day the hookup occurred, estimate based on the last time you remember drinking or being in that setting.
When to Test if You Don’t Remember What Happened
Maybe you woke up sore. Maybe you’re just panicked. Either way, if you were too drunk to remember what kind of sex happened, or if sex happened at all, you’re not alone. We hear this question more than people admit out loud: “Do I need to test even if I’m not sure anything happened?”
Here’s how to break it down. Think of the timeline like a decision tree:
- If it’s been fewer than 5 days since the night in question, your best move is to wait before testing, unless you have clear symptoms or suspect assault. Most STDs won’t show up on tests this early. Testing now may give you false reassurance, especially for chlamydia, gonorrhea, and HIV.
- If it’s been 7 to 13 days, you’re in a good window to test for faster-showing infections like chlamydia, gonorrhea, and trichomoniasis. Even if your test comes back negative, you might want to retest later, especially if symptoms show up or if you continue feeling unsure.
- If it’s been 14 days or more, you’re now hitting the peak testing window for most infections. This is the best time for a more complete panel that includes HIV and syphilis, both of which take longer to show up in blood work.
For example, one reader shared this:
“I tested on day 4 after a party I blacked out at. It came back negative, but I still felt gross and paranoid. I retested at 15 days and found out I had chlamydia.”
This isn’t about scaring you, it’s about testing smart. Start with what you can test for now. Then plan a retest around day 30 if your first results were early or if symptoms change.
What If I Think I Was Assaulted?
This part is hard, but if you suspect you were assaulted or touched without consent, you’re not alone. Sexual assault doesn't always look like violence. If you were too drunk to consent, or if someone took advantage while you were unconscious, that still counts.
You have options. You can go to a hospital or clinic that provides sexual assault forensic exams (SAFEs), also called rape kits. These exams can include STD testing, emergency contraception, and evidence collection, even if you’re unsure you want to report. In the U.S., you can find help through the RAINN National Sexual Assault Hotline at 1-800-656-4673 or via online chat.
If you're not ready to involve anyone else, at-home STD tests can be a quiet first step. You don’t have to decide everything at once. You deserve safety and healing, even if you're still unsure what happened.
Can Alcohol Affect STD Symptoms or Test Results?
Alcohol can't give you an STD, but it can make things more confusing. Some people say that early STD symptoms are like a hangover: they make you feel achy, tired, or sick. Dehydration, not gonorrhea, could make you feel burning when you pee. It's possible that your throat hurts because you threw up, not because you have oral herpes.
But if symptoms persist or feel unusual, like a rash, discharge, sores, or pelvic pain, it’s worth testing. And no, alcohol doesn’t mess up the results of the test itself. It just makes it harder to interpret your body’s cues. When in doubt, trust your instinct. If something feels off, it probably is.
Rapid Test vs Mail-In Lab: Which Is Better When You're Anxious?
When you’re spiraling after a night you don’t remember, speed and privacy matter. You want answers, but you don’t want to walk into a clinic and explain why.
At-home tests give you control. You can do a rapid fingerstick test in your bathroom and see results in 10–20 minutes. Or you can collect a urine or swab sample and mail it to a lab, which gives you higher sensitivity and broader screening.
Figure 2. Comparing test methods for post-drinking anxiety. Choose based on your timeline, symptoms, and privacy needs.
Do I Need to Retest? What If the First Result Was Negative?
Here’s the reality: one test might not be enough. That doesn’t mean you’re doomed. It just means timing matters.
If you test before day 7, you might catch nothing, even if you were exposed. A negative result that early is not a green light to move on. It’s a check-in, not a final word. We recommend retesting at day 14–30 to cover the window period fully, especially for HIV, syphilis, and herpes.
If you’ve already tested at day 14 or later, that’s solid for infections like chlamydia and gonorrhea. If your panel didn’t include HIV or herpes, consider a follow-up or broader test around day 30–45 for peace of mind.
Here’s a snapshot scenario:
“I tested on day 10 with a mail-in kit. It came back negative, but I still had this sore spot I couldn’t ignore. I did another test at 5 weeks, turns out it was HSV-1. I wouldn’t have caught it without retesting.”
Retesting isn’t about fear, it’s about confirmation. Especially if symptoms develop, or if your test was taken early. If you’re unsure what’s included in your kit, check whether it screens for herpes, trichomoniasis, and syphilis, some rapid panels skip those.
Privacy, Discreet Shipping, and No One Else Needs to Know
Worried someone will find out you ordered a test? You’re not alone. Many people delay testing not because they don’t want answers, but because they’re scared of someone seeing the box or email.
That’s why discreet shipping is the norm for at-home STD kits. Orders arrive in plain, unbranded packaging, no pharmacy logos, no “STD” labels. Results are delivered securely, either by email, app, or printed cassette readouts you interpret privately.
If you’re traveling, living with roommates, or in a new relationship where things feel fragile, timing your delivery and choosing the right test method can help you stay in control. And if you need support understanding your results, most services offer anonymous chat or follow-up resources without requiring a name.

People are also reading: You Got Tested… But Did They Actually Check for Everything?
What If I Test Positive?
First: breathe. A positive STD result isn’t a punishment, it’s a diagnosis, and most are treatable. Some, like chlamydia, gonorrhea, and trichomoniasis, can be cured with one round of antibiotics. Others, like herpes or HIV, are lifelong, but manageable with daily care and medication.
If you test positive after a drunk hookup, that doesn’t make you reckless or dirty. It makes you human. What matters next is confirming the result (especially if it came from a rapid test), accessing treatment, and notifying any current or recent partners.
Many people freeze at the idea of texting someone: “Hey, just so you know…” But you don’t have to do it alone. Some clinics offer anonymous partner notification tools, and at-home services often include scripts or resources.
One reader shared:
“I tested positive for gonorrhea and panicked. I didn’t even know if it was from that night. I told my recent partner anyway, and they were grateful. We both got treated. It felt like damage control, not shame.”
If your test comes back positive, most providers will offer next steps, or you can bring the result to a clinic for confirmation and treatment. If you want to retest later or make sure a partner has access to their own kit, the 7-in-1 Complete At-Home STD Test Kit offers a confidential way forward.
FAQs
1. I was blacked out. What if I don’t even know if sex happened?
That’s more common than you think. If you woke up with your clothes off, some soreness, or just a gut feeling that something happened, even if no memory is there, it’s okay to test. You don’t need proof of penetration to justify taking care of your health. Testing isn’t a courtroom decision. It’s a wellness check.
2. How soon should I test after drunk sex I barely remember?
Aim for at least 7 days after the night in question, even if it’s all fuzzy. That’s when things like chlamydia and gonorrhea start to show up. For more accuracy, and for infections like HIV or syphilis, day 14 to 30 is better. If you’re still unsure? Test now, then again later. Two tests = peace of mind without the guessing games.
3. I tested negative at 5 days. Am I in the clear?
Not yet. That’s a little early, especially for anything blood-based like HIV or syphilis. Think of your first test as a checkpoint, not a finish line. A second test around the 2–4 week mark will give you more confidence in the results. No shame in double-checking. It's what smart people do.
4. Will a rapid test work even if I was wasted the night it happened?
Yup. Being drunk during exposure doesn’t affect how the test works. The real factor is time. If it’s been long enough (usually 14+ days), rapid tests for HIV, syphilis, and others can give you solid results. Just don’t test too early and expect clarity, that’s how people get false peace of mind and then stop testing too soon.
5. I feel gross, but I don’t have symptoms. Should I still test?
Yes. Some STDs can be completely silent, especially in the early stages. You could feel fine and still be positive for something like chlamydia or trichomoniasis. That anxious gut-feeling you’re having? It's valid. Testing helps you stop the mental spiral and know what’s real.
6. Can I really do this without anyone finding out?
Absolutely. At-home STD tests ship in boring, totally unmarked boxes. No pharmacy logos, no weird labels, no “you got chlamydia!” surprises on the packaging. Results are sent online or shown on the test strip, and that’s it. No one sees them unless you choose to share. Your health, your timeline, your power.
7. What if I think I was assaulted?
First of all, we’re so sorry you’re even asking that. If there’s even a chance that what happened wasn’t consensual, you deserve care and support, period. That might mean going to a hospital for a forensic exam (they won’t pressure you to report). Or it might mean starting with a private test at home. You don’t have to figure it all out today. But you do deserve answers and safety moving forward. The RAINN hotline is a great place to start if you want to talk to someone anonymously.
8. How do I even tell someone if I test positive?
This is hard. But it doesn’t have to be a confession, it can be an act of care. You can say, “Hey, I recently tested positive for [STD], and I think you might want to get checked too.” Some clinics offer anonymous notifications. Some apps do it with one click. Most people actually respect the honesty, and it might help them catch something early, too.
9. I don’t want to go to a clinic. What’s the best test I can do from home?
A full panel kit is your best bet, one that covers the big ones: chlamydia, gonorrhea, trichomoniasis, syphilis, herpes, and HIV. You can grab a rapid combo test or a lab-processed one depending on how fast you need results.
10. Wait, what if the condom broke and I didn’t know?
Another real scenario. Condoms can slip or tear, especially during drunk, clumsy, or blackout sex. If you’re unsure, or you just can’t remember whether a condom was even used, treat it like unprotected sex. Better safe than secretly infected.
You Deserve Answers, Not Assumptions
Nobody should feel ashamed or unsure after a night they don't remember well. Getting tested for STDs isn't just about finding infections; it's also about taking care of yourself when things seem unclear, scary, or out of control.
You are making a strong, clear choice whether you have already tested or need to test again. And that is more important than what you forgot.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. WHO – Global Fact Sheet on STIs
2. Getting Tested for STIs – CDC (testing recommendations and timing)
3. STI Screening Recommendations – CDC
4. Otorhinolaryngological and STI Testing Considerations (PubMed)
5. STD Testing Guidance – Mayo Clinic
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Dr. Eleni K. Vassos, MPH | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.