KZN’s HIV Progress Is Real, But Here’s Why At-Home Testing Still Matters
Quick Answer: No, standard STD tests don’t check for everything. Herpes, trichomoniasis, and even HPV are often excluded unless you ask. Knowing what’s missing is key to protecting yourself, and your partners.
So What’s Actually Included in a “Standard” STD Test?
Here’s the hard truth: there is no universal definition of a “standard” STD panel. What’s included depends on where you go, what you ask for, and what the provider or kit assumes you want. Most basic panels test for chlamydia, gonorrhea, and sometimes HIV and syphilis. That’s it.
Even at clinics that offer full panels, certain infections, like herpes simplex virus (HSV-1 and HSV-2) and trichomoniasis, require specific testing that isn’t bundled in unless you request it. Many providers won't include a herpes test unless you have visible sores. Some at-home kits skip trich altogether. And few places test for HPV unless you're getting a cervical Pap smear.
This isn’t just a policy problem. It’s a public health blind spot. And it leaves thousands of people each year confused, symptomatic, and falsely reassured.
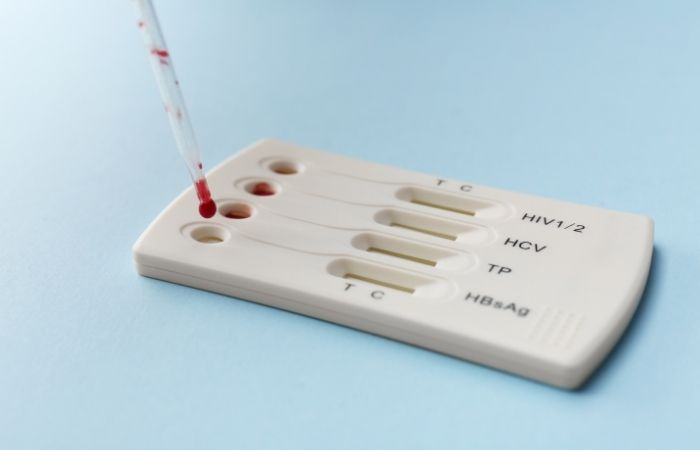
Figure 1. What’s usually tested in a standard panel, and what gets skipped unless you speak up.
Think about that for a second: a person could leave their “STD checkup” thinking they’re all clear, when in reality, they’ve never been tested for the two viruses responsible for the majority of lifelong STIs in the U.S. That’s a failure of communication, not morality. And it’s one we can fix, if we start asking better questions.
Why Are Some STDs Left Out of the Standard Test?
The short answer? Cost, stigma, outdated assumptions, and insurance policies. The long answer is more frustrating, especially if you’ve ever gotten tested, felt relief, and then found yourself back in the exam room weeks later with unexplained symptoms.
Unlike other health screenings, STD testing isn’t standardized across clinics or labs. Providers often default to what’s covered by insurance or what’s considered “routine.” If you don’t specifically ask, they might skip tests they assume you don’t need. In some cases, they’ll only test for infections based on your gender, sexuality, or whether you’re showing symptoms, decisions that often reflect bias more than science.
And herpes? That’s its own can of worms. Many providers actively avoid testing for it unless a sore is visible. Why? Because the blood test shows past exposure, not necessarily an active infection. So instead of explaining that, they just leave it off the panel, and most patients never know to ask.
Figure 2. Why certain STDs aren’t included in standard panels, even though they’re common and contagious.
But here’s the kicker: many people don’t know what their test included until something goes wrong. They assume “negative” means “safe.” Then comes the itch, the discharge, the pain, the panic, and the second visit, where they’re told that test didn’t include what they thought it did.
“I Had Symptoms… But My Test Said Negative”
Rafael, 31, started feeling discomfort during urination and noticed a greenish discharge. He went to a walk-in clinic and asked for an STD check. The test came back negative, and the doctor told him it might just be irritation or stress. A week later, he visited a second clinic, where they tested specifically for trichomoniasis, and it came back positive.
“I was furious,” he said. “Not at myself, but at the fact that I had to guess which infections they were checking for. I thought they knew what to test for. I had symptoms.”
This happens more than anyone talks about. You feel something off, you do the “responsible” thing, and then you’re told it’s probably nothing, until it turns out to be something that wasn’t even part of the original test. The system puts the burden on patients to know what they need, but most people don’t have a medical degree, or a crystal ball.
That’s where better testing options, better education, and more transparency come in. No one should have to guess what they’re being tested for. And no one should be shamed for asking to go beyond the basics.
Why “Negative” Doesn’t Always Mean “Clear”
Let’s be real: getting that text or email that says your STD panel is “negative” can feel like a clean bill of sexual health. But unless you know exactly what was tested, and what wasn’t, you might be working with a false sense of security.
Herpes, HPV, and trichomoniasis are some of the most commonly missed infections in standard testing. They’re also some of the most frequently passed between partners who thought they were all clear.
Here’s the other reality: false negatives can happen. If you test too soon after exposure, especially during the window period, your body might not have produced enough antibodies to show up on a test. That’s why knowing when to test and when to retest matters just as much as knowing what to test for.
If your test came back negative but something still feels off, trust yourself. Test again. Ask for more. You’re not being paranoid. You’re being smart.
People are also reading: Yes, You Can Get Herpes Without Sex, Here’s How It Happens
How to Ask for the Tests You Actually Need
One of the trickiest parts of getting tested is realizing you might need to be the expert in the room. If you're at a clinic or urgent care and say, “I want a full STD test,” they’ll often nod, but you won’t know what that means unless you press. So press.
Here’s how that conversation might go:
“Can you walk me through exactly which infections you’re testing for today?”
“Does this panel include herpes, trichomoniasis, or hepatitis testing, or do those need to be requested separately?”
“If I’m asymptomatic, are there any infections you’d normally skip unless I ask?”
It might feel awkward in the moment, but the alternative is walking out the door without the clarity you came for. And if your provider won’t give you straight answers, or makes you feel judged, it’s okay to go somewhere else. Or skip the clinic entirely.
At-Home STD Tests: What They Offer (and What They Don’t)
Over the past few years, at-home STD testing has exploded. And for good reason: it’s discreet, accessible, and often faster than waiting for an appointment. But just like in clinics, not all home test kits include every infection, and some don’t tell you exactly what you’re being screened for unless you read the fine print.
Some kits are super targeted, only testing for HIV or chlamydia. Others are broad panels, but still skip herpes or trich. A few premium kits include everything, but you’ll need to check carefully before you click “buy.” If your symptoms are genital but your kit only tests via blood sample, that’s a mismatch. Likewise, if you want to know your HSV-2 status, make sure the test distinguishes between HSV-1 and HSV-2.
Figure 3. What different testing methods include, and what they leave out.
Our take? If you want clarity across the board, don’t gamble.
Shame and Silence: The Real Barriers to Better Testing
For many people, the hardest part of getting tested isn’t booking the appointment or waiting for results. It’s asking for more than the bare minimum. It’s saying the words “herpes” or “trich” out loud without flinching. It’s wondering if someone will judge you for being thorough, for being curious, for wanting full control over your sexual health.
Here’s your reminder: asking for what you need doesn’t make you paranoid. It makes you powerful. You’re not being “extra.” You’re being exact. In a system that often gives the most limited test by default, you have every right to say, “That’s not enough for me.”
Whether you’re freshly hooking up, starting a new relationship, healing from a breakup, or simply overdue, knowing your full status isn’t just peace of mind. It’s self-respect. And it's care for the people you touch.
FAQs
1. Wait... so “full STD panel” doesn’t actually mean full?
Not even close. Most “full panels” only test for chlamydia, gonorrhea, HIV, and maybe syphilis if you're lucky. Herpes? Not usually. Trich? Doubtful. HPV? Forget it unless you’re getting a Pap smear. So yeah, "full" is more of a marketing term than a medical truth. Always ask what's actually on the menu.
2. Why wouldn’t they just test for everything while they're at it?
You’d think it would be standard, right? But nope. There are a few reasons, insurance restrictions, outdated guidelines, and some serious stigma. Herpes, for example, isn’t tested unless you’ve got visible sores, and many providers avoid it because explaining the results takes time. The system assumes people don’t want to know. We say: that’s outdated BS.
3. Can I have trich or herpes even if my test came back negative?
Yup, totally possible. If your panel didn’t include those tests, and most don’t, then your “negative” result only applies to what they did check. Trich often gets skipped unless you specifically ask, and herpes? It’s practically a ghost test. Ask by name. Or better yet, go for a combo kit that includes it all.
4. Is it awkward to ask a doctor to test me for everything?
It can feel that way at first, especially if you're not used to advocating for yourself in a medical setting. But let’s be real, this is your health, your body, your future sex life on the line. It’s not awkward to want answers. It’s badass. And if a provider makes you feel weird for asking? Find one who won’t.
5. How soon after sex can I take an STD test?
Depends on the infection. Chlamydia and gonorrhea can show up within a week or two. HIV and syphilis need more time, around 3 to 6 weeks. Herpes antibodies can take months to show. If you test too early, you might get a false negative. That’s why many folks test at 2 weeks, then again around 12 weeks to be sure.
6. My partner says they were “tested recently”, should I believe them?
Believe their intention, but don’t assume they know exactly what they were tested for. Most people think a negative result means they’re 100% clear. But unless they saw the list of included tests, or asked for herpes or trich by name, they probably weren’t checked for those. This is why honest convo matters.
7. Do all at-home STD kits test for herpes?
Definitely not. Many only cover the basics: chlamydia, gonorrhea, HIV. Some skip herpes entirely, or lump HSV-1 and HSV-2 together without clarity. If you want herpes results, look for a kit that clearly includes both types. No guessing.
8. What if I tested negative, but something still feels off down there?
Trust your instincts. A negative test only means they didn’t find what they looked for. If they didn’t test for herpes or trich, those infections are still on the table. You’re not being dramatic for going back or testing again. You’re being thorough, and that’s smart, not paranoid.
9. Why is herpes treated like some secret shame bomb in the medical world?
Because stigma dies hard. Herpes is wildly common, most adults have some version of it. But providers worry patients will panic if they see “positive” on a test without understanding what it means. So instead of educating, they often skip it. That’s not care. That’s cowardice. You deserve better.
10. Can I just test at home and skip the whole awkward clinic thing?
Absolutely. At-home testing has come a long way. Just be picky. Not all kits are built the same. Choose one that includes the infections you care about, not just the easy ones. Bonus? No small talk. No stirrups. Just results.
You Deserve the Whole Truth, Not Half the Picture
Getting tested shouldn’t be a gamble. You shouldn’t have to decode the fine print or cross-reference test panels to make sure you’re protected. You did the right thing. You got tested. But now you know, most panels don’t check for everything. Not by default. Not unless you ask.
If you’re here reading this, maybe you’re second-guessing a “negative” result. Maybe you’re experiencing symptoms that won’t go away. Or maybe you’re just trying to stay ahead of the curve. Wherever you are, you’re not overreacting. You’re being smart.
This at-home combo kit tests for chlamydia, gonorrhea, HIV, syphilis, and both types of herpes. It skips the clinic but doesn’t skip the details. Because clarity isn’t a luxury, it’s a right.
How We Sourced This Article: We used current guidelines from global and U.S. health authorities, peer-reviewed studies, and firsthand accounts from people navigating real STD testing confusion. This article was shaped by lived experiences, medical facts, and practical tools for readers. Around fifteen reputable sources informed the content; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. WHO – Herpes Simplex Virus Fact Sheet
2. Getting Tested for STIs | CDC
3. Which STI Tests Should I Get? | CDC
4. Sexually Transmitted Infection (STI) Tests | MedlinePlus
5. Get Tested for STIs | American Sexual Health Association
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to stop, diagnose, and treat STIs. He combines a no-nonsense, sex-positive approach with clinical accuracy and is dedicated to making his work available to more people in both urban and off-grid settings.
Reviewed by: L. Harrell, NP, MPH | Last medically reviewed: October 2025






