Tested Too Soon for HIV? Here’s What That Negative Could Mean
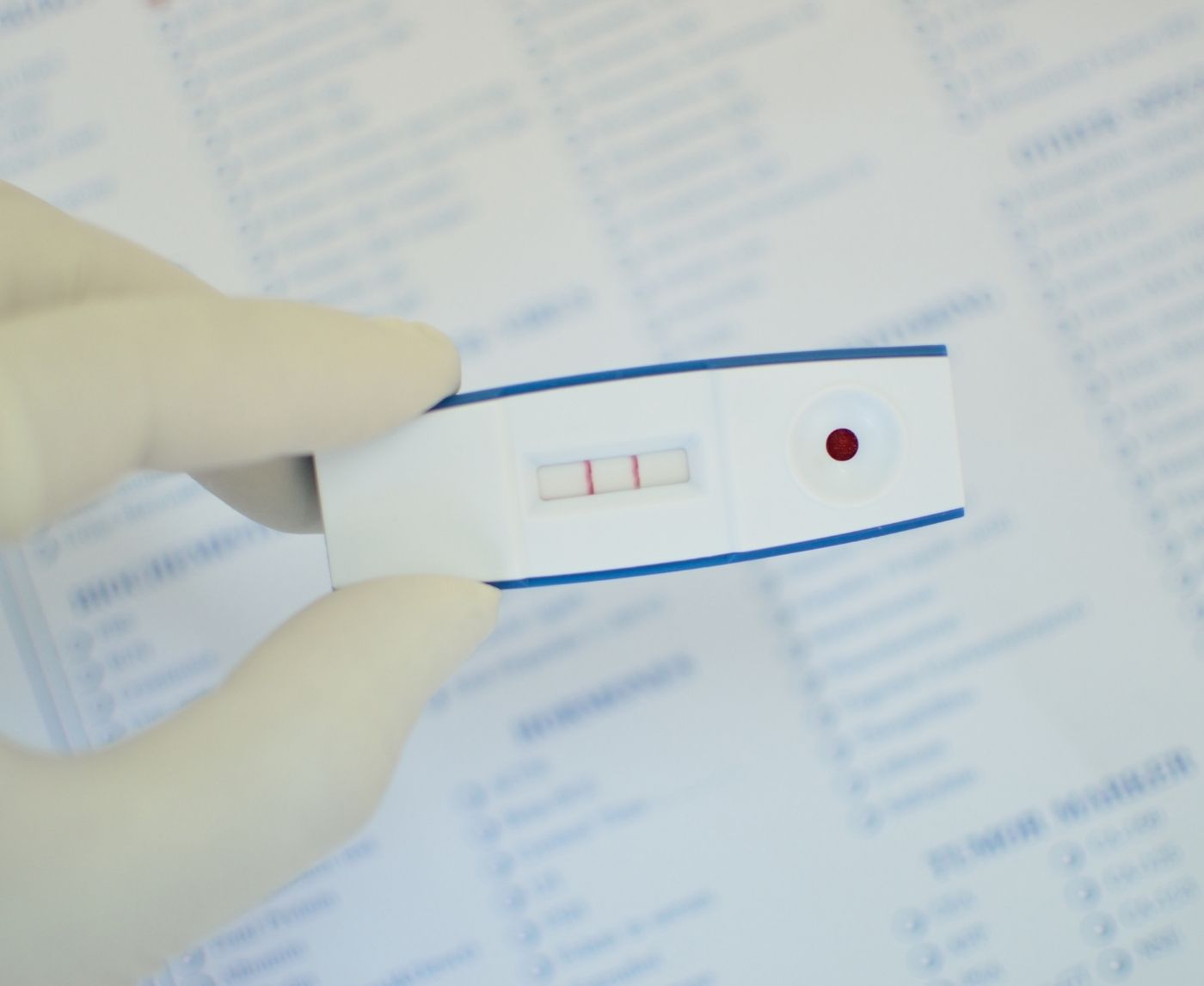
Quick Answer: If a faint second line shows up on an HIV rapid test within the test's read window and is easy to tell apart from an evaporation line, it could mean a reactive result. Don't guess if you're not sure. Do the test again in a few days, or get a lab-based test to be sure.
Why This Happens More Than You Think
It’s easy to assume that rapid tests give you black-and-white answers. Two lines = positive. One line = negative. No lines or one control line = invalid. But in the real world, it’s rarely that clean. Lighting, test timing, your own anxiety, and even the way the cassette absorbs the sample can create misleading visuals. And when it’s your health on the line, even a shadow of pink can feel like a verdict.
Marcus, 31, took an HIV rapid test after a casual encounter he couldn't stop thinking about.
“I did it in my car at lunch,” he told us. “There was one line at first. Then about twenty minutes later, I thought I saw a second one. It was barely there. I freaked out, called in sick, and went straight to urgent care.”
What Marcus saw may have been an evaporation line, an issue that happens when test cassettes dry past their intended read time, making ghost lines appear. Or it could have been an actual reactive line forming slowly due to low viral load. Either way, he did the right thing by retesting with a provider.
There’s a reason this keeps happening: rapid tests are designed to be easy, but not necessarily foolproof. Especially when we’re scared, tired, or desperate for a clean answer.

People are also reading: Herpes Symptoms but Negative Test? Read This First
How HIV Rapid Tests Actually Work (And Why Faint Lines Happen)
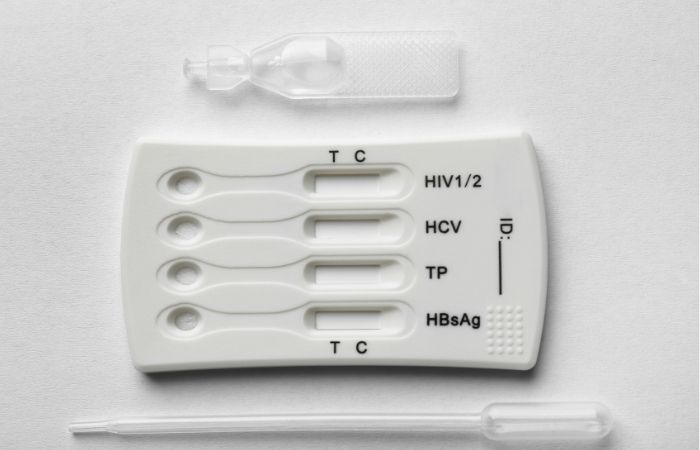
Most at-home HIV rapid tests are lateral flow devices, the same basic tech as pregnancy tests and COVID swabs. You apply a sample (usually blood or oral fluid), and the device pulls that sample across a strip coated with antibodies. If your body has produced HIV antibodies (or in some test types, antigens), they bind and form a visible line.
But here’s the tricky part: these tests are incredibly sensitive to timing, temperature, humidity, and user handling. A faint line can appear because of:
• A low level of antibodies (early infection)
• Slight evaporation effects after the read window
• Residual blood in the cassette well
• Improper lighting when interpreting the result
• A truly weak but real positive signal
That last one is especially critical. In some cases, a faint line is a positive. In others, it’s noise. How do you tell the difference?
Start by understanding the read window for your specific test. Many kits, especially those from brands like OraQuick or similar fingerstick-based cassettes, specify a 20 to 40 minute result window. After that, anything that appears is considered invalid. That includes ghost lines, bleed-throughs, or anything you think you see once the timer’s done.
Understanding What “Positive” Actually Looks Like
If you’ve ever seen a crisp, blazing second line appear on a pregnancy test, you might expect HIV rapid tests to work the same way. But HIV lines can be fainter, especially if antibody levels are low or the person is early in their infection. Some test kits are highly sensitive but don’t produce bold visuals, and that’s where panic often starts.
Let’s break it down with what most HIV rapid test kits are designed to detect:
Table 1. Common HIV rapid test types and how their positive results typically appear. Always check your test's official insert for read-time rules and interpretation examples.
If you see a line and aren’t sure whether it’s real, here’s a general rule: if it shows up within the official time window and is even slightly visible, it warrants a retest or confirmatory lab test. If it shows up after the window or only when you squint under a desk lamp an hour later, don’t trust it.
The Mental Spiral: When a Line Is All It Takes
Leila, 22, had been testing regularly ever since her ex cheated. One night, she took an at-home HIV rapid test after a new partner disclosed he had multiple previous partners but hadn’t tested in months. The control line appeared quickly. But after ten minutes, a faint shadow started to emerge where the test line should be.
“I stared at it for thirty minutes,” she told us. “I took a photo. Zoomed in. Sent it to a friend. Then started shaking.”
What Leila experienced wasn’t uncommon, it was what clinicians call HIV test anxiety. When fear kicks in, the mind amplifies signals. That pinkish hue becomes undeniable. Your pulse pounds in your ears. You see what you’re most afraid to see. And with HIV stigma still so entrenched, even the suggestion of a positive result can feel like a life sentence.
This is why no one should go through testing alone, especially if you’ve got trauma, high anxiety, or a history of health spiraling. If you're holding your test right now and don’t trust your eyes, pause. Take a photo. Step away from the light. Then breathe. You are allowed to feel scared. But you also deserve clarity, not panic dressed as proof.
False Positives, False Negatives, and the Trouble with “Trusting the Line”
Here’s the kicker that no one tells you in the instruction booklet: HIV rapid tests aren’t infallible. They’re good, some even excellent, but they live in the real world, not a lab. That means there’s a margin for error, and if you’re testing at the wrong time or reading the test incorrectly, you might walk away with the wrong answer. Sometimes that answer is too hopeful. Sometimes it’s needlessly terrifying.
A false positive occurs when the test shows a reactive result, even though the person is not infected. It’s uncommon, but not impossible. Some causes? Cross-reactivity with other antibodies (like those from recent vaccines or viral infections), test contamination, or reading the test after the valid result window. It’s why test instructions emphasize that anything showing up after 40 minutes, for example, should be ignored, even if it looks real.
On the flip side, a false negative can happen if you test too early, before your body has produced detectable antibodies. In that case, you could be HIV-positive, but the test just isn’t picking it up yet. This is especially risky during the “window period”, the early weeks after exposure when the virus is present, but your immune response isn’t strong enough to flag it on a rapid test.
Let’s say you test at 12 days post-exposure. You’re panicking. The test is negative. You breathe, then Google for five hours straight. Only later do you find out that most rapid tests won’t show accurate results that early. The result felt reassuring, but it wasn’t reliable. That’s false reassurance. And that, too, can be dangerous.
So how long should you wait? Let’s look at what the data says about window periods and test reliability:
Table 2. Typical detection timelines and accuracy risks for common HIV test types.
So no, it’s not that rapid tests are unreliable. It’s that many people use them before the clock has run its course, or misinterpret what they’re seeing. Testing too soon is like pulling cookies from the oven before they’ve baked. You want the truth, not gooey guesswork.
The Most Common Mistakes People Make with Rapid Tests
Aaron, 26, thought he did everything right. He followed the steps, waited 15 minutes, saw one clear line, and tossed the test in the trash. Relief. But later that night, something gnawed at him. He dug the test out of the bin. And there it was, a second line, faint but unmistakable.
Here’s what went wrong: he read the test too early. Some rapid HIV tests require the full window to process. Reading them at 10–12 minutes might not reveal a reactive result yet. On the flip side, waiting too long can create evaporation lines that look like positives when they’re not.
Other common missteps? Using an expired kit. Not waiting long enough after exposure. Storing the test in extreme heat. Or misreading the control line as the test line. (Yes, it happens, and it’s terrifying.)
Rapid tests are designed to be user-friendly, but they’re still medical devices. The kind that respond badly to rushing, humidity, and late-night panic. That’s why we always recommend reading your results within the official window, in good lighting, and only from a test that’s been stored at room temperature, not in your car’s glovebox or a sweaty backpack.
And if you’re unsure? Retest. Or better yet, follow up with a lab test that can put the what-ifs to rest.
People are also reading: New HIV Injection Lowers Risk by 96%, Here’s What to Know
When You Should Ignore the Line Entirely
There are moments when the line, faint, clear, or ghostly, just isn’t trustworthy. If it appears outside the test window, it’s not valid. If the control line fails to appear at all, the test is invalid. If you bled too much into the sample well and the cassette looks flooded, the results might be compromised. Same goes for damaged tests, expired materials, or instructions that got tossed in a moment of panic.
Valerie, 33, used a test that had sat in her bathroom drawer for over a year. The control line was weak, the test line barely visible. She spent the weekend convinced she was positive. Monday morning, she bought a new test, used it in fresh light, and it was clearly negative. She still followed up with a lab test just to be sure, but the contrast was undeniable.
Sometimes the problem isn’t your blood, or your body. It’s the test itself.
If your result leaves you with more questions than answers, don’t rely on pixel zooming and group chat consensus. Order a fresh kit. Or better yet, get a lab test that removes the human error factor. Your peace of mind is worth more than your pride.
Order an FDA-approved HIV rapid test here, confidential, shipped discreetly, and backed by real clinical guidance. Because guessing shouldn’t be how you navigate something this serious.
When to Retest, and Why It Matters More Than You Think
There’s a reason most health providers don’t consider a single HIV rapid test the final word, especially when timing, stress, or visual uncertainty is involved. Even if your result seems clear, if you’re still inside the window period, you need to test again. Not to doubt the science, but to confirm the timing lined up with what the test is built to detect.
Let’s say you took a test at 14 days post-exposure and it came back negative. That doesn’t mean you're in the clear just yet. Antibodies may not have formed fully. Your body might be lagging. Or maybe the test wasn't sensitive enough that early. Retesting at the 4-week mark, and again around 8 to 12 weeks, closes that uncertainty loop.
Same goes if you got a faint positive line. Even if the test window matched and the line was within the time limit, a lab-based follow-up is key. A rapid test is a powerful screening tool, but it’s not a diagnosis. That final word comes from a confirmatory lab assay, like a Western blot or PCR-based test.
So when should you test again?
- Immediately: if your first test was invalid or the result was unclear, take a new one now.
- 4 weeks post-exposure: best for early detection, especially with 4th gen or RNA tests.
- 6–12 weeks: optimal window for antibody-based rapid tests to catch reactive cases.
- After PEP: test 4–6 weeks after finishing PEP meds, then again at 12 weeks.
Don't think of retesting as something you have to do out of fear; it's just part of the process. Like checking the locks at night, not because you don't trust the door, but because it makes you feel better.
Rapid Test vs Lab Test: What’s the Real Difference?
There’s a misconception that at-home rapid tests are “cheap” or “less accurate,” but that’s not really fair. They’re just different. Rapid tests are designed for speed, privacy, and accessibility. Lab tests are built for depth, sensitivity, and confirmatory precision.
If you're stuck between them, or considering both, here’s what matters:
Table 3. Key differences between rapid and lab-based HIV tests.
For many people, rapid tests are the first step. But if your result is unclear, your timing was off, or you’re someone who spirals easily, getting a lab test might be your way out of the uncertainty loop.
You can order a rapid HIV test discreetly here, but remember, it’s only one part of a full picture.
Burnout from Testing: When Checking Becomes Obsessive
Andre, 29, had tested himself for HIV 17 times in six months.
“Every time it was negative,” he said. “But I kept seeing faint lines. Or I thought I did. And I’d spiral all over again.”
What Andre was experiencing wasn’t bad science, it was health anxiety. And for people living with trauma, perfectionism, or high-stakes sex, the rapid test becomes a ritual. A source of temporary comfort that slowly becomes a trap.
This is common. If you find yourself checking old tests hours later. Holding cassettes up to a light repeatedly. Taking photos and zooming in. Retesting three times a day. You’re not alone, but you may be trapped in a loop that tests can’t fix. At that point, support isn’t just about labs, it’s about people. Friends. Counselors. Providers who understand HIV panic without judgment.
You’re allowed to need reassurance. But your life deserves more than constant scanning for pink lines. When testing becomes torment, it’s time to shift the focus, from chasing certainty to choosing care.
Is It Time to Test Again?
Not sure yet? Think about this:
- Has it been at least three weeks since you might have been exposed?
- Did I follow the test instructions exactly, even the timing?
- Is my result clear, or does it make me doubt?
- Am I testing to get answers or to calm down my never-ending panic?
If you’re nodding through these, it’s time. Test again, with clarity. With compassion. With timing on your side.
Order your next test now, delivered discreetly, no questions asked. Take back control, one answer at a time.
FAQs (Faint Lines, False Alarms, and What to Actually Do)
1. Does a faint line mean I’m HIV positive?
It might, but don’t jump to conclusions. If the faint line showed up within the test’s result window (usually 15–40 minutes), and it’s clearly in the test region, that can mean a reactive result. But “faint” doesn’t mean “for sure.” It could also be an early immune response or just a fluke. Retest. Confirm with a lab. What matters isn’t how dark the line is, it’s whether your next move is grounded in facts, not fear.
2. Why does the line look different every time I test?
Because tests live in the real world. Maybe your lighting changed. Maybe your hand shook. Maybe the test sat out too long before you started. Some lines come in bold. Others whisper. The thickness, color, and visibility can all vary, especially if you’re testing early after exposure. So don’t try to compare lines like Instagram filters. Focus on whether the line is there within the read window. That’s what counts.
3. I saw a line hours later. Should I be worried?
Nope. That’s a ghost line. Once the test window closes, the results don’t count, period. Evaporation lines can show up later and mess with your head. If you threw the test in the trash, then dug it out “just to check,” and now you’re spiraling… pause. That line didn’t exist when the result was valid. Time to retest, not overanalyze.
4. Can my anxiety make me see a line that’s not there?
Oh yes. Big time. We’ve heard from people who held the cassette under three types of lighting, took 20 photos, adjusted contrast, and swore there was something there. Anxiety plays tricks, it makes shadows look like signals. You’re not crazy. You’re scared. But that’s why we don’t trust the eye alone. If you’re unsure, retest with a new kit, good light, and a calm mind (or at least a cup of tea in hand).
5. Is a faint line more or less serious than a dark one?
Line color isn’t a ranking system. It’s not “kind of positive” vs “super positive.” If antibodies are detected, even faintly, the test considers it reactive. That said, low antibody levels (like in early infection or during PrEP use) can cause fainter results. The important thing? If it’s there and it’s valid, take it seriously, but don’t panic. Let the lab tell you what’s next.
6. Can other things cause a false positive?
They can. Certain autoimmune conditions, recent vaccines, or even technical errors (like too much blood or bad storage) can cause a misleading positive. That’s why no one is diagnosed on a rapid test alone. Every reactive result needs confirmation with a lab test. So if you're staring at a surprise second line and losing sleep, skip the Reddit threads, get the follow-up instead.
7. What if I’ve tested three times and still feel unsure?
That’s not unusual. Some folks test negative repeatedly but keep doubting because of guilt, trauma, or symptoms that feel “too real.” If your tests were taken outside the window period and followed the instructions exactly, they’re likely accurate. But you’re not just looking for a number, you’re looking for peace. Sometimes, the best next step isn’t another test. It’s talking to a provider or therapist who gets what testing stress really feels like.
8. Can I just wait until symptoms appear instead of testing?
Please don’t. HIV can live in your body silently for years without symptoms, and by then, damage may already be happening under the surface. If you’ve had a possible exposure, don’t wait for illness to confirm what a test could tell you sooner. Early detection = early treatment = long, healthy, unshakable life. Don’t play the symptom lottery.
9. Is it better to use a rapid test or go to a clinic?
They both work, what matters is what you need. If privacy, speed, and control help you breathe easier, use a trusted at-home kit. If you want someone to walk you through the process, answer your questions, and do a confirmatory test on the spot, a clinic is gold. You’re not choosing better or worse, you’re choosing your comfort zone.
10. How do I stop obsessing over the test result?
That’s the hardest question. Because sometimes, it’s not about HIV, it’s about needing to feel safe. Seen. Clean. In control. If that line is controlling your sleep, your appetite, your ability to focus, you’re not weak. You’re overwhelmed. Testing should be a tool, not a punishment. If you're caught in the spiral, give yourself permission to step out. Talk to someone. Take a walk. Let your next test be about information, not fear.
How We Sourced This: This article is based on the most recent medical research, real-world testing data, product inserts from the top HIV rapid test makers, and advice from sexual health professionals. The information shared here came from about fifteen reliable sources, such as HIV.gov, WHO testing protocols, CDC guidelines on window periods, and peer-reviewed studies on false positives and testing anxiety. We have picked out some of the most useful and easy-to-read sources below.
Sources
1. CDC — Getting Tested for HIV
2. CDC — HIV in STI Treatment Guidelines
3. OraQuick — Testing & Understanding Results
4. OraQuick IFU — Faint Lines Interpretation
5. Misdiagnosis of HIV Status (NCBI) – Issues with Faint Lines
6. University of Washington — HIV Diagnostic Testing Core Concepts
7. NY State Rapid HIV Testing Workbook & QA Guidelines
Author: Dr. F. David, MD
Reviewed by: Janelle Rivas, MPH – Sexual Health Researcher
Visit our homepage to explore more guides or order your next test discreetly and confidently.