How to Read Your At‑Home STD Test (And When to Trust the Result)
Quick Answer: A negative herpes test doesn’t always mean you’re in the clear, especially if you tested too early, chose the wrong test type, or made a common user mistake. Retesting after the window period often reveals the truth.
It Feels Like Herpes. So Why Did the Test Say No?
Let’s start with the disconnect, the emotional and physical whiplash of feeling all the signs of a herpes outbreak, only to get a negative result. Maybe it started with an unusual itch. Or you noticed a small blister after a rough weekend. Maybe a partner told you they tested positive and now every twinge in your genitals feels like proof.
That was Marcus’s situation. He’s 28, lives in Oakland, and had what he described as “a friction sore” after a camping trip. “It wasn’t even painful,” he said. “But my ex had tested positive for HSV-2, and I panicked. I ordered a rapid test. Negative. But I couldn’t let it go.” Marcus retested three weeks later with a lab-based blood test. This time, it came back positive for HSV-2.
This isn’t rare. In fact, it’s a common sequence: symptoms, negative test, persistent worry, retest, confirmation. So why the false calm up front? Let’s break it down.
What the Herpes Rapid Test Actually Detects
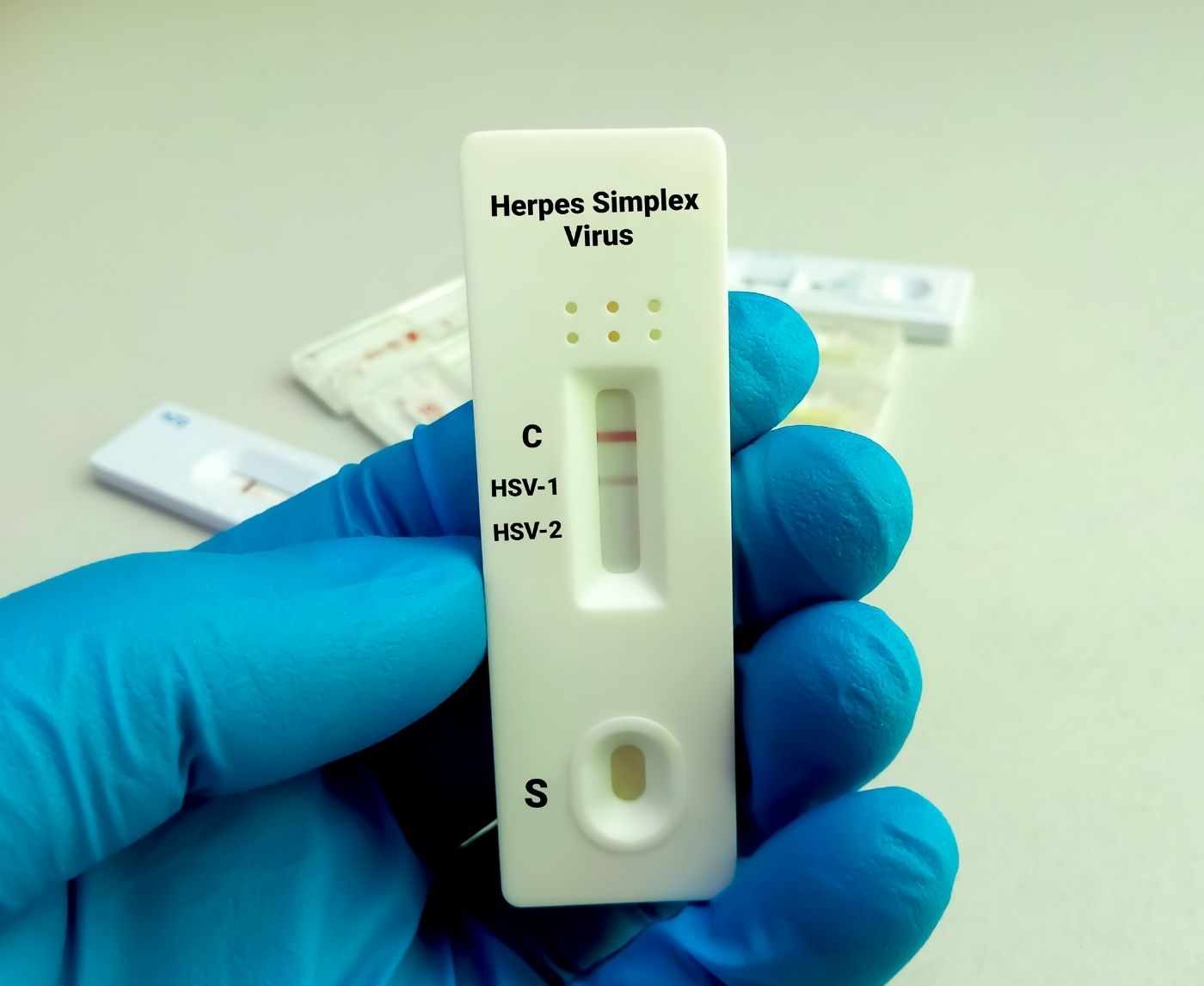
Most at-home herpes rapid tests detect antibodies in your blood, usually IgG, the class of antibodies your immune system produces in response to HSV-1 or HSV-2. Some newer rapid cassettes attempt to detect antigen presence or viral proteins using oral or lesion swabs, but these are less common and often harder to interpret.
Here’s the problem: it takes time for your body to build enough antibodies to trigger a positive result. If you test too early, before your immune system has fully responded, you might get a false negative even if you’re infected. This window period varies from person to person, which makes testing feel like a game of chance unless you understand the science behind it.
Here’s a breakdown of what type of herpes test detects what, and how that impacts your results:
| Test Type | What It Detects | Sample Needed | Earliest Detection Window |
|---|---|---|---|
| IgG Antibody (blood) | Long-term immune response | Fingerstick or venous blood | 16–20 days, most accurate after 6 weeks |
| IgM Antibody (blood) | Early immune response (less reliable) | Fingerstick or venous blood | 7–14 days, but high false-positive rate |
| Viral Culture or PCR | HSV DNA or active virus | Swab from sore | 1–3 days from symptom onset |
| Rapid Antigen Swab | Viral protein on surface | Swab from lesion | During active symptoms |
Table 1. Different herpes test types and what they actually detect. Each test has strengths and timing requirements that affect your results.
If you used a rapid antibody test and took it within two weeks of your first possible exposure, there’s a good chance your body hadn’t produced enough detectable antibodies yet. That doesn’t mean you’re negative, it means you’re early.

People are also reading: Can You Get HIV from Oral Sex? What the Science Really Says
Window Periods and the Waiting Game
The window period is the stretch of time between when you're exposed to HSV and when a test can reliably detect it. For antibody-based tests, the most common type of at-home herpes rapid test, that window can range from 16 to 42 days, depending on your immune response, test sensitivity, and whether you’ve had herpes before.
Here’s a deeper look at how window periods affect herpes test accuracy over time:
| Days Since Exposure | Likelihood of Accurate Result | Recommended Action |
|---|---|---|
| 1–10 days | Low | Wait to test unless symptoms are active (use swab if so) |
| 11–20 days | Moderate | Initial test okay, but follow up in 2–3 weeks recommended |
| 21–42 days | High | Most antibody tests become reliable in this window |
| 43+ days | Very high | If still negative, likely true negative, unless exposure ongoing |
Table 2. Window periods and herpes test reliability over time. Testing too early leads to the highest rate of false reassurance.
That means if your partner had a known outbreak and you had sex five days ago, your negative test today doesn’t rule out infection. If you wait until the 3–6 week mark, your antibody levels are far more likely to register.
The Most Common Herpes Test Mistakes (And How to Avoid Them)
Herpes rapid tests can offer privacy, convenience, and relief, when used correctly. But in real life? People are human. They’re anxious, distracted, sometimes drunk or stoned, and often terrified of what the result might say. That’s a recipe for mistakes, and when it comes to at-home herpes tests, even a small slip can throw off your result.
Take Priya, for example. She was 24, had a one-night stand, and started noticing what she thought was a yeast infection, itching, redness, discomfort during sex. She ordered a rapid test the same day. But in her rush, she didn’t realize she needed to wait 15 minutes exactly to read the results. She peeked early. Then forgot about it and came back an hour later. There was a faint line. She wasn’t sure what to believe.
Here are the most common user errors we’ve seen in herpes rapid testing, told through stories like hers, and explained in plain language:
Misreading Faint Lines: Many rapid tests rely on color change or lines to indicate a positive result. A common error is dismissing a faint line as a “maybe.” In most tests, any visible test line, no matter how light, should be considered positive. Faint lines often appear during early seroconversion when antibody levels are just starting to rise.
Timing Errors: Every test comes with a result window, often 10 to 20 minutes. Read too early, and antibodies may not have bound yet. Read too late, and evaporation lines can appear, creating a false positive. Use a timer. Set an alarm. Don't guess.
Storage Mistakes: Heat, humidity, or expired kits can compromise accuracy. Don’t keep the test in a hot car. Don't store it in a bathroom cabinet where steam collects. Check the expiration date before use. These kits are sensitive medical devices, not breath mints.
If you didn't wash your hands or followed bad hygiene when you collected blood, you might have added things that change the results. Use sterile lancets and alcohol swabs. Don't touch the cassette surface with your fingers or reuse anything.
Testing Too Soon After Exposure: We’ve already covered this, but it bears repeating, timing is the #1 error. Testing three days after sex might offer emotional comfort, but scientifically, it doesn’t mean much. The test can’t detect what your body hasn’t built yet.
Mixing Up Control vs. Test Lines: Every test has a control line (C) and a test line (T). If the control line doesn’t appear, the test is invalid, period. Some users confuse the T line as the only indicator and ignore a missing C line, wrongly assuming they’re negative. Always read both markers.
Alcohol or Blood Flow Errors: Not squeezing enough blood, not allowing it to flow properly into the cassette, or using lotion-covered fingers can all cause invalid results. If the test feels like it “didn’t work right,” it probably didn’t. Retest when calm, clean, and ready.
What Does a Faint Line Really Mean?
This is one of the most emotionally charged questions in at-home herpes testing: is that barely-there line a yes or a no?
The answer: in most rapid herpes antibody tests, any visible test line, even if faint, is considered a positive result. That’s because antibodies don’t appear all at once. Early in your immune response, your body may produce just enough to trigger the test but not enough to make the line dark. Over time, as antibody levels rise, that line will become stronger.
But here’s where it gets complicated. Some users see faint lines appear after the designated read window. These “ghost lines” or evaporation shadows can look real but aren’t. That’s why you must read the test only during the time window printed in the instructions. Not earlier. Not later.
Jessica, 35, had been exposed to HSV-1 through oral sex and tested herself 10 days later. “There was a line, but I could barely see it,” she said. “I didn’t know what to think. I Googled for hours.” She retested at day 28. This time, the line was unmistakable.
So if you’re seeing a faint line and you’re within the read window? Consider it a signal. Retesting a few weeks later can confirm whether it was the start of a seroconversion or a misread.

People are also reading: First Time Getting an STD Test? Here’s Exactly What to Expect
When Confirmatory Testing Is a Good Idea
At-home tests are powerful tools, but they aren’t the final word. If you have symptoms but test negative, or if you get a positive result and need confirmation for peace of mind or treatment access, clinical follow-up is a smart move. Here’s when confirmatory testing is recommended:
1. You have symptoms but tested negative: Especially if you tested before the 21-day mark, confirm with a follow-up antibody test or a swab if sores are present.
2. Your test had a faint line and you’re unsure: Don’t guess. A repeat rapid test or a lab-based IgG/IgM combo can clarify.
3. You had a known exposure within the past 2–3 weeks: Even if you feel fine, a clinical PCR swab or lab test can catch early infections that rapid kits may miss.
4. You’re pregnant, immunocompromised, or planning to disclose status to a partner: Clinical confirmation ensures accuracy and protects both you and others.
Herpes confirmatory testing is usually done through a blood draw (IgG) or a PCR swab of a lesion. You can request this through a telehealth provider, urgent care, or primary doctor. Some lab-based online services also allow self-scheduling without seeing a clinician in person.
If you want discreet access, our at-home Herpes Rapid Test Kit can offer a first step before booking a clinical confirmation. But always follow up if symptoms persist or questions remain.
Interpreting Results in Special Cases
Herpes testing isn’t one-size-fits-all. Some bodies react differently. Some immune systems delay. And some situations introduce extra noise that makes results harder to read.
Pregnancy can alter immune response timelines, leading to delayed or ambiguous antibody production. False negatives are more common, and swab testing may be a better route during outbreaks.
Immunosuppressed individuals, such as those with HIV or on medications for autoimmune diseases, may also take longer to produce detectable antibodies. Clinical support is critical in these cases.
Recurrent outbreaks without a prior positive test often mean the person was infected earlier but never confirmed it. In these situations, PCR testing of active lesions is the gold standard for confirmation.
Mixed HSV status (positive for HSV-1 but unsure about HSV-2) can complicate blood test interpretation. Some rapid tests don’t differentiate, leading to false assumptions about genital vs. oral infection.
Each of these cases deserves a second look. If your result feels out of sync with your symptoms or history, don’t brush it off. Retest or escalate to a provider who understands herpes testing deeply.
FAQs
1. Can you really have herpes and still test negative?
Yes, and it’s more common than you think. Herpes is sneaky, your body needs time to build up enough antibodies for most tests to catch. If you test too soon after exposure (especially in the first two weeks), your result could come back negative even if the virus is already settling in. It doesn’t mean the test is bad. It just means biology hasn’t finished doing its thing yet. We’ve seen people test negative at day 10, then positive by week five. Timing is everything.
2. What’s the deal with faint lines on herpes test kits?
Think of it like a pregnancy test, if there's a line, no matter how light, something’s up. A faint line usually means your body is starting to show antibodies, but they’re not strong yet. It's not a maybe. It's a "probably, but let's double check." If it showed up within the test’s read window, you should consider it a positive and either retest later or confirm with a lab. But if that faint line popped up an hour after you were supposed to read the test? That’s an evaporation line, not a result. This stuff is sensitive, use a timer and trust it.
3. How long should I wait to retest if I think I tested too early?
Aim for three to six weeks post-exposure. That’s when most people’s immune systems have built up enough antibodies for a test to catch. Some people seroconvert faster, others take longer, especially if they’re immunosuppressed or have other health conditions. One test too soon doesn’t give you the full picture. Waiting sucks, but knowing for sure is better than guessing.
4. Can stress mess up my herpes test result?
Not directly, but indirectly, absolutely. Chronic stress can slow down your immune response, and if your immune system is dragging, it may take longer to develop detectable antibodies. Plus, stress can trigger herpes outbreaks if you already have the virus, which leads people to test during a flare-up, but if they’re using the wrong type of test (like an antibody test instead of a swab), they might still get a negative. TLDR: stress matters. But the test isn't lying, it just might be asking your body for answers it hasn’t produced yet.
5. Is it true you can have herpes and never know it?
Yep. That’s the kicker. Up to 90% of people with HSV-2 and a huge chunk of HSV-1 carriers don’t realize they’re infected. No sores, no pain, maybe just a rash they blamed on shaving or tight jeans. Herpes can be totally silent, until it’s not. That’s why so many people get blindsided by a positive test after years of thinking they were fine. Silence doesn’t equal safety. It just means the virus is quiet.
6. My test was positive but I feel totally normal. What now?
First, take a breath. This is common. A positive herpes test without symptoms just means your body has been exposed and developed antibodies. You might never get an outbreak. You might get one tomorrow. Either way, it doesn’t mean you're dirty, dangerous, or doomed. It means you now know something important about your health, and you can take steps to care for yourself and your partners from here on out.
7. Can I test myself at home if I just had unprotected sex last weekend?
You can, but just know it’s probably too soon to get a reliable result. If it’s been less than 10 days, most rapid tests won’t pick up anything yet. Testing early might soothe your anxiety for a minute, but it won’t give you certainty. Wait until at least day 21 if you can. If you absolutely can’t wait, use a swab test during symptoms (if you have any), and follow up with an antibody test later. Peace of mind takes a little patience.
8. Do herpes tests tell you where the infection is?
Not really. Blood-based tests like IgG just say whether you have antibodies to HSV-1 or HSV-2. They don’t tell you if it’s oral, genital, or somewhere else entirely. Only a swab of an active sore can do that with certainty. So if your test says HSV-1 positive, and you’ve had cold sores your whole life, that makes sense. But if you’re HSV-2 positive and never had symptoms, it’s worth asking your doctor what that might mean for your risk profile and future partners.
9. How reliable are these at-home herpes tests anyway?
When used correctly and during the right window period? Pretty solid. Most are 90–97% accurate, especially IgG blood-based kits. But they're not foolproof. Use them as part of your health toolkit, not the only piece. If something feels off or if your result doesn’t match your symptoms, retest or go clinical. Trust your gut, and trust your timeline.
10. Do I really have to tell someone if my test was only faintly positive?
That’s a personal choice, but here’s the truth: if the test picked something up, even faintly, it’s worth being honest. You don’t have to dump your whole sexual history over dinner, but saying, “Hey, I got a weird result, and I’m following up, but I wanted you to know” is powerful.It shows that you care, not that you are ashamed. And what if they judge you? That says more about them than it does about you.
You Deserve Answers, Not Assumptions
If you've made it this far, you’re already taking control of your health. That moment of doubt, the negative test that doesn't match your symptoms, isn’t the end of the road. It’s the start of a smarter path forward.
Whether it’s your first test or your fifth, remember that herpes testing isn’t always straightforward. Immune systems are unique. Timing matters. And your intuition, if something doesn’t feel right, deserves attention, not dismissal.
Don’t stay stuck in the maybe. Retesting is easy, discreet, and sometimes the only way to get the truth. This at-home combo test kit checks for the most common STDs and helps you rule out other possibilities too. Peace of mind is only a few drops of blood away.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. Performance Characteristics of HSV-1 and HSV-2 IgG Assays – NIH Study
2. Comparison of HSV Antibody vs PCR Testing – Clinical Comparison Study
3. Diagnosis of HSV: Laboratory and Point-of-Care Tools – PubMed
4. HSV PCR vs Culture Accuracy in Genital Herpes Diagnosis – Virology Journal
5. Mayo Clinic – Herpes Diagnosis and Testing Overview
6. Planned Parenthood – Herpes: Symptoms, Testing, and Treatment
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: K. Langford, RN, MPH | Last medically reviewed: October 2025
This article is just for information and should not be used as medical advice.