HIV Rapid Test Errors and Faint Lines: How to Know What’s Real
Quick Answer: A negative Hepatitis B test doesn’t always mean you're in the clear. Testing too early, using the wrong test type, or misunderstanding faint lines can all lead to false negatives. Retesting is often necessary for accurate results.
Who This Article Is For (And Why It Matters)
This guide is for anyone who’s faced the limbo of a negative test result but still feels uneasy. Maybe you had a risky hookup during a weekend trip. Maybe your partner just tested positive. Maybe your doctor ordered liver labs, and they came back “slightly elevated,” but you feel totally fine.
If you’ve taken a Hepatitis B test, especially an at-home rapid version, and you're wondering if it was too soon or done wrong, this article is for you. We’ll walk you through how Hep B testing works, why timing and test type matter so much, and what to do if you still feel unsure after a negative result. Testing is not just about getting a result, it’s about getting the right result at the right time.
We'll also explain how test types differ, what those confusing antigen and antibody labels actually mean, and when a second test is not only reasonable but essential.

People are also reading: Does Herpes Cause Cancer? What the Research Really Shows
How Rapid Hepatitis B Tests Actually Work
Most at-home Hepatitis B rapid tests use a lateral flow method to detect specific antigens (usually HBsAg, Hepatitis B surface antigen) or antibodies (anti-HBs, anti-HBc) in your blood. These proteins only appear at certain stages of the infection, which makes timing critical.
Here’s the simplified science: If your body hasn’t yet produced enough of the virus or your immune system hasn’t started reacting to it, the test won’t pick anything up. That’s why testing during the so-called “window period” can produce a false negative, even if you're infected.
The most common test kits fall into one of these categories:
Figure 1. Common Hepatitis B markers and what each test looks for. Misunderstanding these can lead to false assumptions about your status.
If your test only checks for HBsAg, and you're still in the incubation period, you might test negative even if you're infected. That’s why retesting is recommended, especially after high-risk exposure.
When Negative Doesn’t Mean “Safe”
A negative Hepatitis B result feels like a green light, but in many cases, it’s more like a yellow light at best. Why? Because your body may not yet be producing the detectable antigens or antibodies that the test is looking for. The technical term for this is the “window period”, a stretch of time after exposure when the virus is present but undetectable.
According to the CDC, the window period for Hepatitis B surface antigen is typically 4 to 10 weeks after exposure. Testing too early, even as little as one or two weeks post-risk, can lead to a false negative.
Let’s say you had unprotected sex with someone whose status you didn’t know. You test yourself the next day with a rapid HBsAg kit. Negative. You exhale. But if the virus hasn’t had time to replicate and become detectable, the test simply won’t catch it. You’re not “clean”, you’re just early.
We hear this story all the time. One user shared in a forum: “I tested negative two weeks after a needle stick injury at work. But at six weeks, I tested positive. That first result made me delay telling my partner, which I now regret.”
This is why second testing, at the right time, isn’t paranoia. It’s smart prevention.
The Hepatitis B Timeline: When to Test, When to Retest
Hepatitis B doesn’t show up overnight, and that’s where a lot of testing confusion begins. After exposure, your body goes through stages: incubation, immune response, and finally detectability. If you test during the early stage, even the most accurate test might miss the infection.
Here’s how the timeline typically unfolds:
Figure 2. The Hepatitis B testing timeline. Testing too soon is the most common reason people receive false negative results and delay care.
If you tested within the first 3–4 weeks after exposure, even a high-quality test may not show anything. Retesting after 6–8 weeks gives your body time to show signs of infection that the test can detect. This is especially important for high-risk exposures like unprotected sex, needle sticks, or if your partner has tested positive.
Faint Lines and Misreads: A Common Pitfall
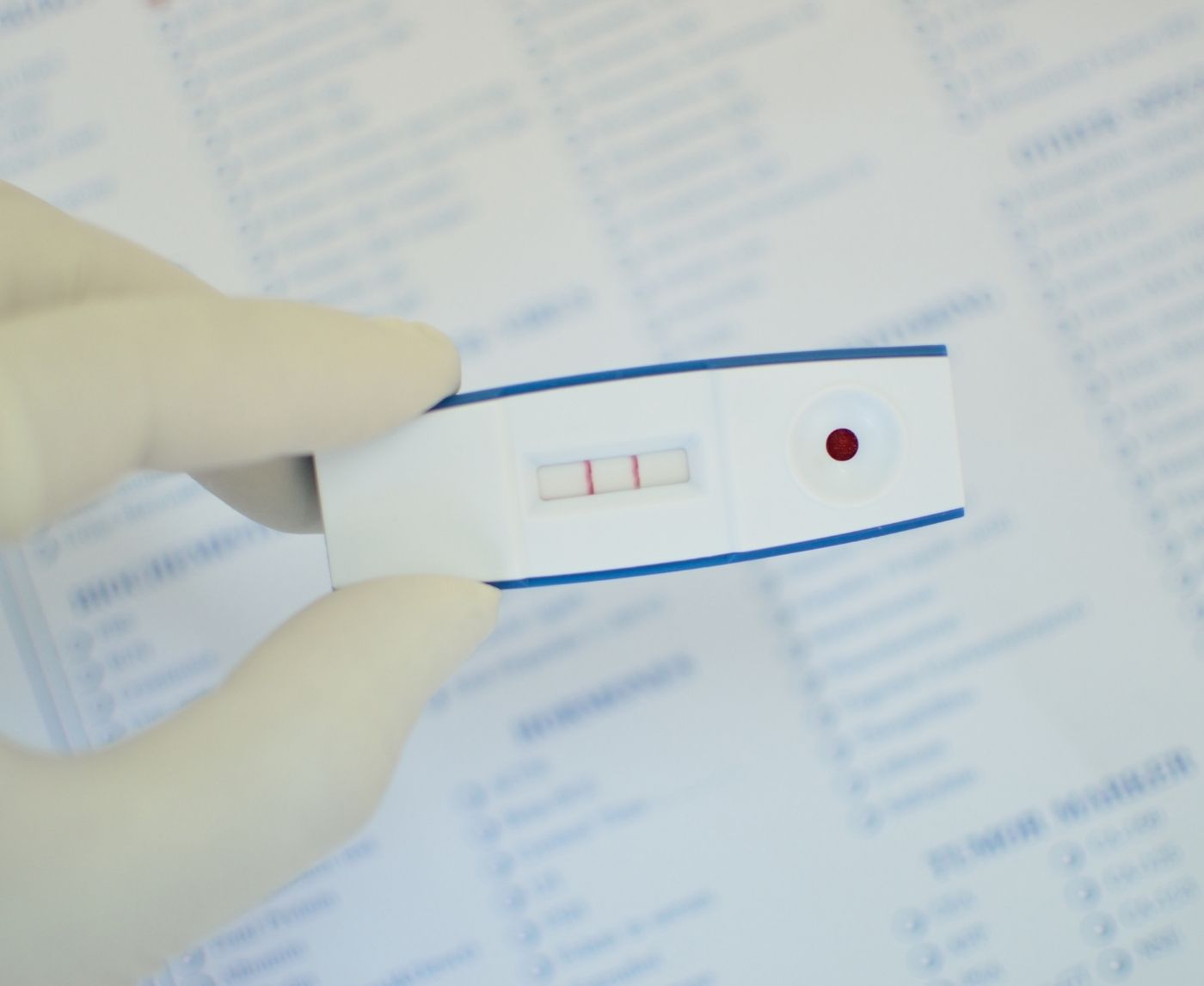
Rapid test results can be deceiving, especially if you're staring at the cassette under bad lighting, with sweaty hands, and anxiety in your chest. One of the most common issues? Misreading faint lines.
Here’s the thing: A faint test line doesn’t always mean “negative.” In fact, most Hepatitis B rapid tests are designed so that any visible test line, no matter how faint, is considered a positive. Many users discard faint lines as “invalid” or “too weak to count,” which leads to missed diagnoses.
In forums and support groups, we’ve heard everything from “I thought it was a shadow” to “It disappeared after 15 minutes, so I figured it was negative.” These misunderstandings are incredibly common and dangerous.
Most test kits include an interpretation guide, but they’re often printed in tiny font or use unclear photos. If you're unsure, the safest move is to assume that a faint line is valid and get confirmatory testing through a clinic or lab.
If you need clarity now, our Hepatitis B Test Kit includes visual guides and follow-up support if you have questions about your result.
“I Waited Two Weeks. It Wasn’t Enough.”
While on vacation, 27-year-old Amira had a one-night stand. Her partner said he was "clean," but she didn't believe him. Two weeks later, she ordered a Hepatitis B test to do at home. It came back negative. She let out a sigh of relief and moved on.
Three weeks later, she got a fever and started throwing up. A visit to urgent care showed that the liver wasn't working right. The clinic did a full HBV panel this time. The result was that HBsAg was present. It had been too early for her last test.
"I thought the first test was enough." If I had waited longer, I might have been able to catch it before I got sick and saved myself a lot of stress.
Amira's story is a classic case of getting false hope from early testing. She did the right thing by testing early, but she didn't do a second test. What happened? A late diagnosis and weeks of an untreated infection.
How Test Type Affects Your Result
Not all tests for Hepatitis B are the same. There are tests that test for the virus itself (antigen test), while others test for the body’s reaction to the virus (antibody test). This means that using the test wrongly may provide an inaccurate test result.
Here’s how test types compare:
Figure 3. Different Hepatitis B test methods and their ideal timing windows.
If you're testing early or need high accuracy, lab-based testing (like NAAT or PCR) is the most reliable, especially during the first month after exposure. But these aren't available in most home kits, which is why timing and test repetition matter so much.
You Deserve Answers, Not Assumptions
If your test came back negative but something still feels off, don’t gaslight yourself. Testing is a tool, not a guarantee. False negatives are more common than most people realize, especially when testing is done early or the kit is misused.
Whether you’re checking after a new partner, managing long-term liver health, or just trying to ease the anxiety of a “what if,” clarity matters. STD Test Kits offers discreet options, support, and fast results, without clinic lines or judgment.
When a Confirmatory Test Becomes Essential
"If you’ve had a high-risk exposure, symptoms, or a faint test result, you need more than one data point. And that’s where confirmatory testing, usually in the form of a lab-based test, comes in. This has much higher sensitivity than the at-home tests," the source explained.
The clinics might do a full Hepatitis B test that includes:
- HBsAg (surface antigen) shows that you are currently infected.
- Anti-HBs (surface antibody) means that you are getting better or are immune.
- Anti-HBc (core antibody) shows that you have had or are still having an infection.
- IgM anti-HBc means that you have a recent infection (acute phase).
This multi-marker method gives you a much clearer picture of where you are in the infection timeline. A quick test might say "negative," but that doesn't mean there isn't an infection. It means "not found with this method at this time."
For people in high-risk groups, like healthcare workers, pregnant individuals, or those with multiple partners, getting confirmatory lab testing is especially important. It can guide treatment, prevent transmission, and in some cases, protect newborns from infection during delivery.
Some clinics offer this testing through telehealth and mail-in kits. If access is a barrier, STD Test Kits can point you to solutions with more privacy and fewer delays.

People are also reading: Can You Get HPV Without Having Sex?
Testing Isn’t Always One-and-Done
People often think that one bad test means they are "clear forever." But with Hepatitis B, you often need to take several tests at different times to get a full picture of your health. Especially when things are complicated, like:
- People with weakened immune systems: It may take their bodies longer to show signs that can be seen.
- Pregnant women: False negatives early in pregnancy can make it take longer for the baby to get the help they need to stay alive.
- Chronic liver symptoms: A person may test negative on an antigen test but still have a long-term, low-grade infection that can be found by antibody tests or DNA analysis.
This doesn't mean the test failed; it just means that infections change over time, and so should your testing strategy.
If your symptoms change, your risk factors increase, or your first test was done during a questionable time window, consider yourself overdue for a retest. You're not paranoid. You’re informed.
Mythbusting: Common Misbeliefs That Lead to Misdiagnosis
Let’s clear up a few dangerous myths that often cause people to ignore the need for a second test:
- “If I don’t have symptoms, I can’t have it.” , Over 50% of Hepatitis B cases are asymptomatic, especially in early stages.
- “My test was negative, so I’m immune.” , A negative result does not mean immunity unless you're specifically testing for antibodies after vaccination.
- “I only needed one test.” , Timing, test type, and exposure level all influence how many tests you may need to get an accurate picture.
Believing any of the above can lead to missed diagnoses, ongoing transmission, and emotional stress down the road. The fix? Accurate knowledge and a proactive testing plan.
When to Retest: A Simple Summary
If you’ve tested negative for Hepatitis B but have concerns about accuracy, here’s a quick guide to retesting:
Figure 4. Retesting recommendations based on exposure and symptom context. When in doubt, repeat testing is always safer.
Peace of Mind Is a Test Away
If you’re sitting with that uneasy “but what if” feeling, here’s your permission to act on it. Testing is care. Retesting is smart. And clarity is always worth it.
You don’t have to wait until symptoms worsen or anxiety takes over. Whether you use an FDA-approved at-home kit or talk to a doctor about confirmatory labs, the goal is simple: know your status, protect your health, and stop second-guessing.
You deserve peace of mind, not false reassurance. Order a Hepatitis B Test Kit today and take back control of your health.
FAQs
1. Can you have Hepatitis B and still test negative?
Yes. If you test during the window period, which is usually the first 4 to 6 weeks after being exposed, your body may not show any signs. This could give you a false negative even if you have the disease.
2. How long does it take to find out if you have Hepatitis B?
Most surface antigen tests (HBsAg) have a window period of 30 to 60 days. If you test before that, you might not get the right results. Antibody tests take a little longer to work, but they work better later on.
3. Do faint lines on Hepatitis B tests mean that the test is positive?
Most quick tests do see any test line, even a faint one, as positive. People often think these are "invalid" or "negative," which makes it take longer to figure out what's wrong.
4. When should I get tested for Hepatitis B after being around someone who has it?
You can test for the first time as soon as two weeks after the first test, but for more accurate results, you should wait six to eight weeks before doing it again. Early tests might not find an infection because there aren't enough antigens in the blood.
5. Should I get tested again if I had sex with someone who tested positive?
Yes. Even if you tested negative on the first test, you should retest at 6 weeks and 12 weeks. You were exposed to someone who actually does have Hepatitis B. You can also ask for post-exposure prophylaxis.
6. Is one negative test enough to prove that I don't have Hepatitis B?
Not all the time. If you took the test too soon or your immune system isn't strong, the result might not be right. You might want to think about getting a second test if you have symptoms or were at a high risk of being exposed.
7. Can you have Hepatitis B and not show any symptoms?
Yes. A lot of people who have acute or chronic Hepatitis B don't show any signs of it, especially at first. That's why it's so important to test and follow up on a regular basis.
8. Do at-home tests for Hepatitis B work?
Yes, they can be correct, especially if you use them after the window period and follow the directions exactly. But they aren't as accurate as lab tests and might not catch early or mild infections.
9. Should pregnant women get tested for Hepatitis B more than once?
Yes. Pregnant women are frequently screened early and subsequently during pregnancy if there is a risk of exposure, as they may transmit the virus to the infant during delivery.
10. How do Anti-HBs and HBsAg differ?
HBsAg (surface antigen) shows that the infection is still going on, while Anti-HBs (surface antibody) shows that the person has gotten better or is immune from vaccination. If you mix them up, it can be hard to understand the test results.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. CDC – Hepatitis B Information
2. WHO – Hepatitis B Fact Sheet
3. Johns Hopkins Medicine – Hepatitis B Overview
4. Clinical Testing and Diagnosis for Hepatitis B | CDC
5. Hepatitis B Diagnosis and Testing | Mayo Clinic
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Erin T. Silva, MPH | Last medically reviewed: January 2026