Polyamory and STDs: Are You Really at Higher Risk?
Quick Answer: Yes, you can get HPV without having sex. The virus spreads through intimate skin-to-skin contact, including hands, fingers, and genital touching, not just penetrative intercourse.
Who This Article Is For (And Why It Matters)
This guide is for anyone who’s ever had a doctor say “You have HPV” and then immediately felt ashamed, confused, or betrayed, especially if they’ve never had penetrative sex. It’s for people in queer, non-penetrative, or low-body-count relationships who still ended up with an STD they thought they were safe from. It’s for virgins who feel blindsided by their first abnormal Pap result.
Picture this: Nia, 22, had never had intercourse, by choice. She was with her first partner, experimenting with mutual touching and making out. Months later, a routine OB-GYN visit revealed high-risk HPV. Her first reaction: “How is that even possible?” Her second: “Who’s going to believe me?”
We’re here to break down exactly how HPV transmits, when it doesn’t, what counts as “sex” from a viral standpoint, and how to move forward, without blame or fear. Testing is care, not a confession. Let’s clear the air.

People are also reading: Can You Catch Gonorrhea from a Toilet Seat?
What HPV Actually Is, and Why It's So Easy to Catch
Human papillomavirus (HPV) is not a single virus, it’s a group of more than 100 related viruses, some of which cause genital warts, while others can lead to cervical, anal, throat, or penile cancers. According to the Centers for Disease Control and Prevention (CDC), nearly everyone who is sexually active will get HPV at some point in their lives, even if they’ve only had a few partners, or none at all by traditional definitions.
The virus is incredibly common and incredibly efficient. It spreads through skin-to-skin contact, often in places that condoms don’t cover. It doesn’t require ejaculation, orgasm, or even penetration. In fact, HPV can be transmitted:
Table 1: Activities that can transmit HPV without traditional intercourse.
In other words, yes, you can be a “virgin” by social or religious standards and still get HPV. It’s not about morality. It’s about biology.
Why “Virgin” Doesn’t Mean “Immune”
In many cultures, virginity is treated as a protective shield. If you haven’t had penetrative sex, you’re “safe.” But HPV isn’t bound by those definitions. Studies show that even people who identify as virgins have tested positive for HPV, especially when they’ve had oral sex, manual sex, or non-penetrative genital contact.
Consider Luis, 19, who had only received oral sex from a long-term partner. After developing a small wart on his shaft, he got tested. It came back positive for a low-risk strain of HPV. His reaction? “I thought you could only get STDs if you went all the way.” That belief isn’t just wrong, it’s dangerous, because it leads people to skip protection and delay testing.
HPV isn’t picky about what “counts.” It lives in the skin, and it spreads through skin. That means outercourse, fingering, and even skin-on-skin during cuddling sessions can all carry a degree of risk, especially if the virus is active on the skin’s surface at the time of contact.
HPV also has a silent feature: most people who carry it have no visible symptoms. That makes it nearly impossible to “screen” a partner by sight. They may feel perfectly healthy, and still be contagious.
Can You Get HPV from Hands, Toys, or Towels?
Let’s break down a few of the most common (and misunderstood) non-sexual scenarios that come up when people test positive for HPV “out of nowhere.”
Fingers and Hands
Yes, research shows HPV DNA has been found under fingernails and on the skin of people who engage in manual sex. It’s rare for HPV to transmit solely from hand-to-genital contact, but it’s possible, especially if there’s broken skin or shared exposure from prior touching.
Sex Toys
HPV can live on surfaces like vibrators and dildos for hours, even longer in warm, moist environments. If you share toys without cleaning them thoroughly between uses or partners, the risk is real. Use condoms on toys, sanitize between uses, and don’t share if you’re unsure of a partner’s status.
Towels and Toilet Seats
This one’s more myth than fact. While HPV can survive on surfaces briefly, it doesn’t thrive there. There’s very little evidence suggesting that people catch HPV from towels or toilet seats in the real world. It’s far more likely to spread via close contact.
So while the virus isn’t airborne and doesn’t leap across the room, it doesn’t need “real” sex either. HPV is sneaky, stubborn, and sometimes slow to show symptoms, but it’s not mysterious once you know how it works.
If you’re sitting with a new diagnosis and no clear memory of “when it happened,” you’re not alone. The virus could’ve been with you for months, or even years, without ever making itself known. We’ll dive into latency, symptoms, and what to do next in the coming sections.
When HPV Shows Up Late (And Why That Doesn’t Mean Cheating)
One of the most emotionally charged moments in HPV diagnosis comes from timing. You might be in a committed relationship. Maybe you both got tested early on. Then suddenly, months or years later, one of you tests positive. Cue suspicion, heartbreak, and blame.
The truth? HPV can remain dormant for months or even years. It’s a virus that often lies low, without symptoms or detectable signs, and then reactivates due to stress, illness, or immune system changes. This means someone can carry HPV from a previous partner and not know it until a test or Pap smear uncovers it down the line.
According to the Planned Parenthood HPV guide, many people never show symptoms at all, and some clear the virus within 1 to 2 years without ever realizing they had it. But others hold on to it much longer, especially if their immune system isn’t able to fight it off efficiently.
This delay is why HPV doesn’t equal infidelity. Just because a test turns positive during a monogamous relationship doesn’t mean someone cheated. It might simply mean a previously silent virus is now detectable, or was never tested for before.
This matters not just for medical understanding, but emotional protection. Too many relationships rupture over a virus that behaves nothing like most STDs.
Myth vs Fact: Breaking the Shame Cycle
HPV often triggers panic not just because of cancer risks, but because it’s laced with myths. Let’s break a few of them open:
Table 2: Common myths and facts about HPV.
The shame around HPV is socially constructed, not medically warranted. This virus doesn’t care if you’re queer, monogamous, inexperienced, or cautious. It’s stubborn, sneaky, and spreadable in situations most people don’t even realize count as exposure.
If you’ve just been diagnosed, or if you’re watching a partner wrestle with it, breathe. This is not your fault. And you are not alone.
HPV in Queer, Virgin, and Non-Penetrative Communities
Most sexual health research and education still centers on heterosexual, penetrative sex. But that leaves out huge populations at risk, including queer folks, virgins, and those who only engage in mutual touching or toy use.
HPV in WLW (Women Loving Women) relationships
Studies confirm HPV spreads between women, even when neither partner has had sex with a man. Shared toys, oral sex, and skin-to-skin contact all carry risk. Yet many providers still under-screen queer women or assume their risk is low.
HPV in virgin men and AFAB individuals
For those who haven’t had vaginal, anal, or oral sex, the shock of an HPV diagnosis can feel like betrayal. But if you’ve engaged in mutual masturbation, dry humping, or skin-on-skin cuddling, you may have unknowingly been exposed. Virginity doesn’t block skin contact, and that’s all HPV needs.
Trans and nonbinary individuals
Gender-affirming care rarely includes tailored STD education. But genital HPV risk exists for anyone with genital skin, especially if they engage in touch-based intimacy, toy use, or oral contact. Access to vaccines and screening should be inclusive and stigma-free.
This is why we advocate for a broader, more realistic definition of sexual risk, one that includes touch, pleasure, intimacy, and care without shame or binaries. HPV is common, manageable, and preventable, but only if we talk about it honestly.
What HPV Feels Like (When It Feels Like Anything)
Most of the time, HPV doesn’t “feel” like anything. It’s symptomless. That’s part of the danger, it spreads quietly, living on skin without causing immediate warts, pain, or discharge.
When symptoms do show up, they can include:
- Genital warts: Soft, skin-colored bumps on or near genitals, anus, or mouth
- Abnormal Pap smear: The most common way HPV is discovered in people with cervixes
- Oral symptoms: In rare cases, lesions in the throat from oral HPV
But many people test positive with zero signs. This is why regular screening and routine Pap smears matter, especially since some strains of HPV are linked to cervical and other cancers.
And no, genital warts don’t always mean “high risk.” In fact, the strains that cause warts (like HPV 6 and 11) are considered low-risk for cancer. High-risk strains (like HPV 16 and 18) don’t usually produce visible signs, but can cause changes inside the cervix that only a Pap or HPV DNA test can catch.
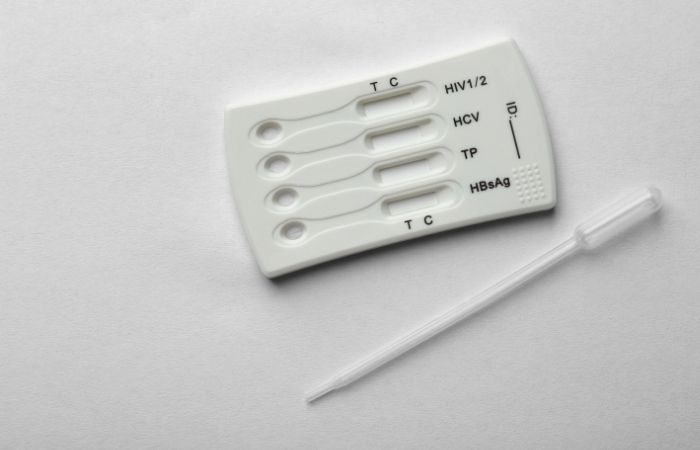
Want to know your HPV status? You can check discreetly from home with our at-home HPV test kit. It’s private, easy to use, and doctor-trusted, because you deserve answers, not assumptions.
People are also reading: Still Positive After Treatment? Here’s What Might Really Be Going On
How to Test for HPV Without Leaving Home
If you’ve never had penetrative sex, walking into a clinic for an STD test can feel awkward, or downright impossible. But HPV doesn’t care about how sex is defined, and thankfully, neither do modern testing options. You can now check for HPV privately with an at-home STD test kit, and for many people, it’s a game-changer.
At-home HPV tests work by collecting a vaginal or cervical swab (for those with a cervix). Some kits also offer anal swab options, though they’re less common. The sample is then mailed to a lab, and results are provided online in a few days. These tests are discreet, accurate, and don’t require a pelvic exam, ideal for people avoiding in-person care due to trauma, privacy, or stigma.
If you don’t have a cervix or are worried about genital warts, a visual exam by a healthcare provider might be necessary. There’s currently no routine HPV test for men or people with penises, but if visible symptoms appear, a diagnosis can often be made based on appearance and context.
Whether you use a home test or go to a clinic, timing matters. HPV can take weeks or even months to become detectable after exposure. If you’re testing after recent contact, you may need to retest later for accurate results.
Can You Prevent HPV Without Abstaining?
Yes, and this part is hopeful. While HPV is incredibly common and easy to catch, you can take powerful steps to protect yourself and your partners, even if you’re sexually active in non-traditional ways.
Vaccines
HPV vaccines like Gardasil 9 offer protection against the most high-risk and wart-causing strains. They’re FDA-approved for ages 9 through 45 and are recommended regardless of sexual history. Even if you’ve already been exposed to some strains, the vaccine can still offer protection against others.
Condoms
Condoms and barriers aren’t perfect against HPV, because the virus lives on skin outside the areas they cover, but they do reduce risk. Use condoms on toys, with oral sex, and during any genital contact. Dental dams and nitrile gloves can also help during touch-based play.
Limit shared surfaces
Clean sex toys between uses, don’t share them without protection, and avoid using them on multiple people without washing. If you’re unsure of a partner’s status, assume risk is possible, even without penetration.
Regular screening
If you have a cervix, begin PAP smears at age 21. Discuss the co-test or home options with your healthcare provider. For the rest of you, be aware of visible changes, such as warts or new growths on your skin.
HPV prevention = awareness, not fear. Sex and intimacy and pleasure and connection = all possible and all yours – without sacrificing your health. No guilt. No judgment. Just good decisions for your body.
Retesting and What to Do If You’re Positive
If you test positive for HPV, take a deep breath. Here’s what comes next:
- Confirm and clarify: If you got your results from a home test or Pap smear, your provider will tell you whether it’s a high-risk or low-risk strain. Most low-risk types cause warts. High-risk types may require a colposcopy or follow-up in 6–12 months to check for abnormal cell changes.
- You don’t need antibiotics: HPV is a virus, so it doesn’t respond to antibiotics. Most cases go away on their own. What’s monitored is your immune system’s ability to clear it, and whether any cell changes are developing.
- When to retest: If your provider recommends follow-up, it’s usually within 12 months. Some people clear the virus quickly, others don’t. If you’re using a home test, wait at least 6 months before rechecking to avoid false reassurance.
- Talk to your partner(s): It can feel awkward, especially if they assume “sex” never happened. But you don’t need to explain or justify every past contact. Just let them know they may want to get tested or vaccinated.
- Vaccination still helps: Even if you’re positive, the HPV vaccine can protect you from other strains. It’s not too late, and getting vaccinated is part of protecting partners too.
Return to STD Test Kits to explore test kits that work with your body, your timeline, and your privacy needs.
What About Emotional Fallout?
HPV doesn’t just hit your body, it hits your identity. For some, a diagnosis triggers panic: “What does this say about me?” For others, it creates spirals of guilt or mistrust in relationships. And for too many, it feels like a stain they didn’t deserve.
You are not dirty. You are not reckless. You are not alone.
This virus doesn’t define your value or sexual choices. In fact, most people get it, and most clear it without ever knowing. Testing positive means you have information now, and with it, the ability to protect your health, and your partners, more than ever before.
Case in point, Ana’s HPV diagnosis at 24; she thought her partner would leave her. Instead, they got vaccinated together. They researched options, booked her follow-up Pap, and made a plan. That’s what sexual health should look like, not blame, but partnership.
Don’t let a virus control your story. You get to write it from here.
FAQs
1. Can you really get HPV without having sex?
Yes, and it messes with a lot of people’s heads. HPV spreads through skin-to-skin contact, not just traditional “sex.” That means fingers, rubbing, oral, shared toys, basically any close contact involving genitals. You don’t need penetration for transmission. You don’t even need to take your underwear all the way off.
2. Wait… so I could’ve gotten HPV from just touching?
It’s possible. Manual stimulation (hands, fingers) can carry the virus, especially if someone recently touched their own genitals or someone else’s. It’s not the most common route, but it’s real. If there’s direct contact, especially skin that’s moist or has microtears, HPV can sneak in.
3. Does a positive test mean my partner cheated?
Nope. HPV can hide out for months or even years before showing up on a test. You or your partner could’ve had it from a long-past relationship, even if things have been monogamous since. It’s a virus, not a moral verdict. Accusations won’t help, but facts will.
4. What if I’ve never had “real” sex, am I still at risk?
Define “real.” If there’s been any skin-to-skin contact near the genitals, think mutual masturbation, humping, or toy play, there’s some level of risk. Virginity doesn’t equal immunity. And by the way, your body doesn’t care how you label things. Viruses don’t check for a “technically still a virgin” card.
5. I only had oral sex. Can that cause HPV?
Definitely. HPV can be transmitted through oral-genital contact, and in some cases, lead to oral HPV or throat cancers down the line. Most people never notice symptoms. That’s why even “just oral” counts when we talk about exposure risk.
6. Is it true that condoms don’t fully prevent HPV?
It’s true. Condoms help a lot, but they only cover certain areas. HPV lives on skin, and it can spread from places that condoms don’t protect, like the base of the penis, labia, or even nearby thighs. Still, barrier protection is way better than nothing.
7. How long can HPV stay in your body without symptoms?
Honestly? It’s the ghost of STDs. It can stick around quietly for years. Most people clear it in 1–2 years, but some don’t. That’s how you can be in a long-term relationship, get tested for the first time, and get a surprise result that isn’t anyone’s “fault.”
8. Can I get HPV from sharing towels or a toilet seat?
Not likely. Those myths have been around forever, but HPV doesn’t do well on dry surfaces. It likes warmth, moisture, and direct skin contact. The odds of getting it from your roommate’s towel? Pretty close to zero.
9. Should I tell my partner I have HPV?
Yes, and it doesn’t have to be dramatic. Think of it like saying, “Hey, heads up, I learned something about my body that might matter to yours.” Most people have or will have HPV. The real power is in having the info, not hiding it.
10. Can I still have sex if I’m HPV positive?
Absolutely. Having HPV doesn’t mean you’re off-limits or dangerous. It means you’re human. Use protection, stay on top of screenings, and talk openly with partners. Sex is still on the table, you just know a little more now than you did before.
You Deserve Answers, Not Assumptions
If you’ve tested positive for HPV, or are terrified you might, you are not dirty, broken, or alone. The truth is, HPV is so common that nearly everyone will encounter it. What matters is how you care for yourself, protect your partners, and take back control of the narrative.
Don’t wait and wonder, get the clarity you deserve. This at-home HPV test kit lets you check privately, safely, and on your terms.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. National Cancer Institute – HPV and Cancer Risk
2. About HPV (Human Papillomavirus) | CDC
3. HPV Transmission and Infection – STI Treatment Guidelines | CDC
4. Non-Sexual HPV Transmission and Vaccination Role | NIH/PMC
5. Human Papillomavirus and Cancer Fact Sheet | WHO
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to stop, diagnose, and treat STIs. He combines clinical accuracy with a straightforward, sex-positive attitude and is dedicated to making his work available to readers in both cities and rural areas.
Reviewed by: Dr. Helena Marks, MPH, DO | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.