Do I Really Need to Retest for STDs After Treatment or Exposure
Quick Answer: You might still test positive after STD treatment because of leftover DNA, antibodies that stay in your body, the timing of the test, or a new infection. Not just whether you took medicine, but also the type of test, the window period, and how you used it all affect accuracy.
Why This Keeps Happening (And Who This Guide Is For)
This article is for anyone who's ever been stuck in testing limbo, positive again after treatment, unsure whether to trust the result, and spiraling down Google rabbit holes trying to make sense of it all. Maybe you’re using an at-home test and saw a line that looked darker than last time. Maybe your clinic test contradicted your symptoms. Maybe your partner swears they didn’t cheat, but your retest says otherwise. You're not alone, and you're not doing anything wrong.
This guide will walk you through the science and emotional mess of testing "after the fact." We'll unpack what false positives really mean, how long it takes for test results to clear, why retesting after treatment sometimes leads to more confusion, and how to take back control when your results don't seem to match your reality.
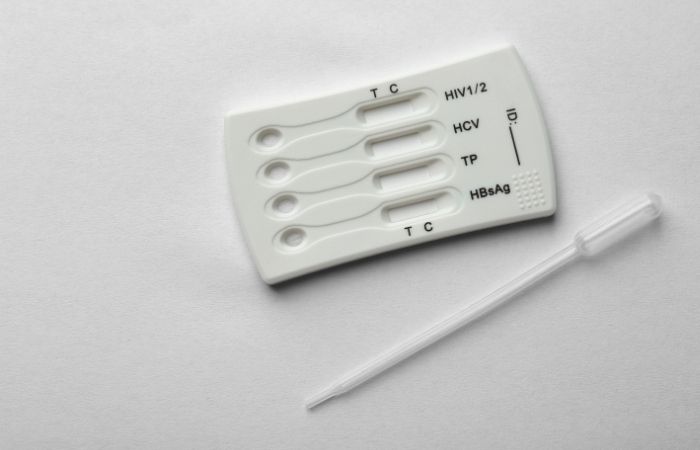
Whether you’re using a discreet Combo STD Home Test Kit or getting tested in a clinic, knowing how these results behave post-treatment is your best defense against panic, and your first step toward clarity.
People are also reading: What That Herpes Test Line Means (Even If It’s Barely Visible)
False Positives vs Reinfection: Not the Same Thing
The term "false positive" gets thrown around a lot in forums, group chats, and late-night internet searches. But here’s what most people get wrong: A false positive doesn’t mean the test is broken. It means the test picked up something that looks like an infection, or part of one, even if you're technically no longer infectious.
Here's the breakdown:
Table 1: Why post-treatment positives happen. Not all "positive again" results mean you're still infected.
Many at-home STD tests (and even clinic-based ones) use nucleic acid amplification tests (NAATs) that detect the genetic material of bacteria like chlamydia or gonorrhea. These tests are extremely sensitive, so sensitive that they can detect leftover fragments of bacterial DNA even after the bacteria are dead. It’s like finding a burnt match and assuming there's still fire.
The Window Period Twist: Timing Is Everything
Now, what if your test says you're negative but you still feel like something is wrong? That could be a false negative, which is where window periods come in. There is a time delay between getting an STD and being able to find it. If you test too soon, you might miss an active infection. If you test too soon after treatment, you might still see signs of it.
Table 2: STD-specific retesting timelines after treatment. Some positives are expected, and don't mean you're infectious.
This is why your doctor (or test instructions) might recommend waiting a few weeks before retesting. It’s not laziness, it’s science. Rushing to retest can backfire and feed fear you don’t need to carry.
“I Thought It Came Back, But It Was the Same Test Again”
Dani, 26, got treated for chlamydia after a routine checkup revealed a positive result. Her partner tested negative, and both agreed to abstain while she completed treatment. But two weeks later, Dani took an at-home test “just to be safe.” A faint line showed up. Her stomach flipped.
“I hadn’t even kissed anyone else. I thought maybe the treatment didn’t work, or he lied about being negative. I felt gross, ashamed, and panicked all over again.”
When Dani reached out to a telehealth provider, the nurse explained what many people don’t know: that DNA fragments can stay in your system for several weeks, especially with NAATs. Because Dani tested just 14 days after treatment, the positive result wasn’t a reinfection. It was the same infection, already gone, but still showing up on highly sensitive tests.
This kind of emotional whiplash is common. And while it’s scary, it’s not your fault. STD testing is a powerful tool, but it has limits. Understanding how your test works, when to use it, and what kind of result it gives can save you from a ton of unnecessary anxiety.
The Role of Human Error: Testing Isn’t Always Plug-and-Play
Especially with rapid at-home tests, accuracy depends not just on the science, but on how you perform the test. Common errors can skew your result in either direction, especially if you're nervous, rushing, or testing outside of recommended conditions (like in your car, at a party, or after drinking).
Some of the most common mistakes include:
- Testing too early: Within the window period, which may give a false negative
- Retesting too soon after treatment: Which can create confusing “still positive” results
- Misreading faint lines: Not all lines mean a true positive; intensity matters, but so does time
- Contaminated sample: Touching the swab tip or storing the kit improperly
- Expired kits: Always check the date; degraded materials reduce reliability
Even clinics can make errors, though rare, mix-ups in processing, labeling, or result interpretation do happen. This is why confirmation testing and clinical context matter.
“But There’s a Line!”, What Faint Results Might Actually Mean
One of the most common sources of panic with at-home rapid tests is the infamous faint line. Some people see a barely-there second line and assume the worst. Others misread control lines or stare at the test 45 minutes later instead of within the recommended 10–15 minute window.
Here’s the truth: a faint line can mean a weak positive, or it can be a ghost line caused by drying reagents, expired kits, or leftover fragments from a cleared infection. It’s not as simple as “any line = positive.” That’s why every at-home STD test comes with timing instructions and a result window you need to follow exactly.
If you're unsure, treat that test as an indicator, not a diagnosis. That means you can either:
- Use a fresh test from a new kit the next day
- Book a lab test or confirmatory clinic test
- Wait 7–14 days to reduce false signal risk
And if you’re using a multi-test kit like the Combo STD Home Test Kit, you have the flexibility to check more than one infection at once, ideal when symptoms are vague or multiple risks are involved.
Time to Pause: What Should You Do Right Now?
If you’ve tested positive again and aren’t sure why, here’s your immediate plan:
- Check the calendar: If it's been fewer than 3 weeks since treatment, your test may still pick up dead cells
- Reconsider exposure: Has there been unprotected sex or new partners since treatment?
- Check your symptoms: Are you actually feeling something new, or just testing for reassurance?
If you're second-guessing everything, stop and breathe. There's no harm in retesting, but doing it too soon can create more confusion. If you're unsure, talk to a provider, or use a time-based decision tree. For example: if it's been over 3 weeks since treatment, symptoms are back, and your partner wasn’t retested, you might be dealing with a reinfection. But if none of those apply, you're likely seeing the body’s cleanup process in action.
When to Retest After Treatment (And When Not To)
Not every positive result needs a retest, and not every retest needs to happen immediately. The biggest mistake people make after STD treatment is testing too early, out of fear. But the CDC and most sexual health experts agree: wait at least three weeks before you retest for most bacterial STDs like chlamydia or gonorrhea. For trichomoniasis, you can test a bit sooner, around 2 weeks. For viral STDs like herpes, retesting isn’t always helpful unless symptoms flare up again.
Why wait? Because antibiotics kill the bacteria, but your body may still shed DNA that tests can pick up. A test taken too early doesn’t show that the infection came back, it shows that your immune system hasn’t finished cleaning up the aftermath.
Here’s a simple guideline:
- Chlamydia: Retest after 21 days minimum
- Gonorrhea: Retest after 14–21 days
- Trichomoniasis: Retest after 14 days
- Syphilis: Use follow-up titers, not standard tests
- Herpes: Retest only if symptoms recur or were unclear
Still unsure when to test? Check out our Testing Window article for more clarity.

People are also reading: Think You’re Immune to STDs? Not Without These Vaccines
Partner Status Matters: The Reinfection Loop
One of the most overlooked causes of a second positive result is partner mismatch. If you got treated but your partner didn’t, or if you resumed sex before their treatment took effect, it’s very possible to pass the infection back and forth. This isn’t about blame. It’s about biology.
Even one unprotected encounter with an untreated partner can cause a legitimate reinfection. And here’s the kicker: many bacterial STDs cause no symptoms in men, so your partner might feel totally fine while still transmitting chlamydia, gonorrhea, or trich.
This is why partner testing (and sometimes retreatment) is part of the protocol. Not because you did anything wrong, but because STDs don’t always show up equally in all bodies. They can hide in asymptomatic carriers, and then come back to surprise you.
“He Said He Got Treated. I Believed Him.”
Sandra, 31, was treated for trichomoniasis after a routine test. Her provider recommended that her partner get treated at the same time, and she passed along the info. “He said he picked up the meds,” Sandra recalls. “So I didn’t ask more questions.”
“I felt fine. No symptoms. But six weeks later, my pap came back with inflammation again. I retested, and it was still positive.”
When she confronted her partner, he admitted he hadn’t filled the prescription. He didn’t want to “make it a big deal.” Sandra’s case wasn’t a testing error, it was a reinfection. But because she waited long enough between treatments, the retest clearly showed a true positive.
This is why honest partner communication matters. And if you’re not sure your partner followed through, protect yourself by retesting at the right time. If you're in a new or non-monogamous relationship, consider rechecking even if you’re both asymptomatic. The goal isn’t control, it’s confidence.
So What Can You Trust?
Trust the test, when it's used correctly, timed appropriately, and interpreted in context. But also trust yourself. If something feels off, advocate for a retest. If you're asymptomatic but scared, you have every right to use a reliable at-home kit to check your status again. Just make sure you're not chasing ghosts caused by impatience or misunderstanding.
And remember: a positive test doesn’t define your worth. It’s a data point. One that can help you protect your health, talk honestly with your partners, and get care without shame.
FAQs
1. Why would I test positive again after I already got treated?
Because STD tests don’t measure “clean.” They measure fragments, antibodies, or live infection, depending on the type. If you test too soon after finishing antibiotics, especially with chlamydia or gonorrhea, your test might pick up leftover bits and call it positive. Doesn’t mean the meds failed. It means the test is still seeing the crime scene tape, even if the suspect’s long gone.
2. How long should I actually wait to retest?
Think 3–4 weeks minimum. That gives your body enough time to clear out the debris, and it gives the test something clean to read. For trich, it can be closer to 2 weeks. Herpes? You don’t usually need to retest unless you’ve got new symptoms or your original diagnosis wasn’t clear.
3. I saw a faint line. That’s positive, right?
Not always. Faint lines live in a weird gray area, sometimes they’re real, sometimes they’re ghost lines, and sometimes they show up because the test sat too long on your bathroom counter. If it’s within the time window and looks legit, treat it seriously. But when in doubt, test again. Don’t let a blur send you spiraling.
4. Can I get reinfected even if I did the treatment right?
Yes. And it happens more than people realize. You can be 100% textbook with your meds, but if your partner didn’t get treated (or got re-exposed themselves), they can pass it right back to you. It’s not always about trust, it’s about timing and biology. Reinfection is a loop, not a judgment.
5. Do at-home tests mess up more often than clinic tests?
They can if they’re used wrong. But when done properly and within the right window, rapid at-home tests are surprisingly solid. The key is following the instructions like your sanity depends on it. Because let’s be honest, it kind of does when you’re spiraling over a pink line at 1AM.
6. Why did I test negative first, then positive later?
That’s a classic window period move. Early tests can miss infections that haven’t fully taken hold yet. So your body might be incubating the STD, but the test just isn’t picking it up, yet. That’s why retesting after exposure or treatment isn’t paranoia. It’s smart.
7. If the test says positive, does that mean it’s 100% right?
No test is perfect. Some, like NAATs, are ultra-sensitive and can trigger positives on trace amounts of dead bacteria. Others rely on antibodies that stick around long after you’re no longer contagious. Always read your results in context, how long it’s been, how you feel, and who you’ve been with matter just as much as the lines on a stick.
8. My partner tested negative. I tested positive. What gives?
This one stings, and it’s common. You could be at different stages of the infection, or one of you could’ve cleared it naturally. Some STDs hit differently depending on anatomy too. Trust the science, but also trust your gut. Ask questions. Confirm if needed. This doesn’t always mean someone lied.
9. Do I need to test again if I don’t have any symptoms?
Honestly? Symptoms aren’t a reliable compass. Plenty of STDs cruise under the radar. If you’ve had a recent exposure, a past infection, or any doubt at all, test. Testing isn’t about fear. It’s about peace of mind.
10. What if I can’t tell if I’ve been reinfected or never fully cleared it?
You’re not alone there. It’s confusing even for clinicians sometimes. Look at timing: if it’s been more than a month and your partner didn’t get treated, reinfection’s likely. If you tested again too early, it might just be residue. Either way, a retest, at the right time, can clear things up faster than your group chat ever will.
You Deserve Answers, Not Assumptions
If you’ve tested positive after treatment, don’t panic. It doesn’t always mean the infection is back, or that your partner betrayed you. It might just mean you tested too early, used a hyper-sensitive test, or misread a faint line.
Your sexual health journey is yours. Testing is a tool, not a trap. Use it wisely, understand its quirks, and always give your body time to catch up to your intentions. If you're ready for a clean slate, a fresh test, or confirmation after treatment, you can start here:
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. CDC – 2021 STI Treatment Guidelines
2. Chlamydial Infections – STI Treatment Guidelines (CDC)
3. Syphilis – STI Treatment Guidelines (CDC)
4. Gonococcal Infections Among Adolescents and Adults – CDC
5. Retesting After Treatment to Detect Repeat Infections – CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease doctor who specializes in preventing, diagnosing, and treating STIs. He combines clinical accuracy with a straightforward, sex-positive approach and wants to make it easier for people in both cities and rural areas to read his work.
Reviewed by: Maria Thompson, RN, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.







