Can You Trust Your STD Results? Here’s When to Worry
Quick Answer: You may need to retest for an STD if your first test was taken too early, if you were recently treated, or if you had new exposure. Retest windows range from 2 weeks to 3 months depending on the infection.
Why This Guide Exists (And Who It’s For)
This guide is for anyone who thought they were in the clear, only to second-guess their results. It’s for the ones who had a wild weekend, the ones who got ghosted after a hookup, and the ones quietly Googling “burning but negative STD test” at 3 AM. Maybe you were exposed again after treatment. Maybe your symptoms won’t go away. Maybe your gut says, “Something’s not right.”
Retesting isn’t a punishment, it’s part of caring for yourself and your partners. Many STDs don’t show symptoms at all. Others have long window periods where the infection won’t show up on tests right away. This guide walks you through when retesting makes sense, how long to wait, and what to do if you're still unsure. We’ll also break down false negatives, treatment effects, privacy options, and what to expect next.

People are also reading: Is It Genital or Oral Herpes? Here’s How to Tell the Difference
Why a Negative STD Test Isn’t Always the Final Answer
Let’s get real, testing negative feels like a relief. But it doesn’t always mean you're in the clear. Every STD has its own “window period,” which is the time between exposure and when it becomes detectable. If you test during this window, your result might come back negative, even if you're already infected. That’s called a false negative, and it happens more often than people think.
For example, chlamydia and gonorrhea typically show up on tests after 7–14 days. But HIV may take up to 3 months to be fully detectable depending on the test type. Syphilis antibodies can take weeks to form, and herpes blood tests might miss recent infections entirely. Timing is everything. That’s why retesting, when done properly, isn’t just cautious. It’s accurate.
And even if your test was technically accurate, what if you were exposed again after that test? Any new sexual encounter resets the clock. Your old result doesn’t cover new risk. That’s why many health professionals recommend retesting after new partners or high-risk exposure, even if you’re symptom-free.
How Treatment Affects Retesting
Here’s where things get tricky. Let’s say you tested positive for chlamydia, got antibiotics, and followed the treatment exactly. Do you need to test again? In most cases, yes. The CDC recommends retesting for chlamydia and gonorrhea about 3 months after treatment, even if your symptoms go away. Why? Because reinfection is common, especially if your partner wasn’t treated too.
For infections like syphilis and HIV, follow-up testing is often part of routine care, even after treatment or stabilization. Some infections may show up on tests even after you’re cured, which can be confusing. For example, syphilis antibodies remain in your system for life. That’s why test interpretation and timing matter.
Antibiotics can also muddy the waters. If you took meds before testing, maybe for a UTI or acne, you could accidentally suppress an infection just long enough to get a false negative. This is why doctors often ask what medications you’ve taken recently. If you were treated before a test, and especially if your symptoms persisted, a retest is a good idea.
If you're unsure when to retest after treatment, this at-home combo test kit can help you recheck discreetly when the timing is right.
When to Retest: Timing Matters More Than You Think
Here’s the tough part, knowing when “soon” is too soon. Retesting right after exposure or treatment might feel proactive, but if it’s done too early, the test can’t catch the infection. You’ll feel reassured, but you won’t actually have an accurate result.
The following table outlines common STDs and when retesting makes sense after treatment, exposure, or a first negative result:
Figure 1. Suggested retesting windows for common STDs after treatment or early testing. These are averages, always confirm with a healthcare provider when possible.
Testing earlier than these windows may still detect an infection, but if the result is negative, it’s not a guarantee. That’s when a follow-up test becomes your best friend.
Exposure Scenarios That Warrant a Retest
Let’s talk real-life situations, the messy, human stuff that doesn’t fit neatly into a doctor’s visit. Maybe your condom broke with someone new. Maybe you didn’t know your partner had an STI until weeks later. Maybe you were drinking, forgot some details, and now something just doesn’t feel right.
Here’s the truth: many people retest not because they’re reckless, but because things changed. Trust shifts. Symptoms show up late. Partners aren’t always honest, or informed. And even if they were, timing still matters. If you were tested right after a hookup, but the STD’s window period hadn’t passed, your result may have been premature.
Take Evan. He had unprotected sex with a casual partner on a Friday night. By Sunday, he was already in a clinic, anxious for answers. His tests came back negative. But by Day 10, he noticed a slight burning during urination. He retested two weeks after exposure. This time? Positive for chlamydia. He hadn’t been reckless, just early.
If you’re reading this thinking, “That could be me,” consider where you are in the timeline. It’s okay to retest for clarity. In fact, it’s smart.
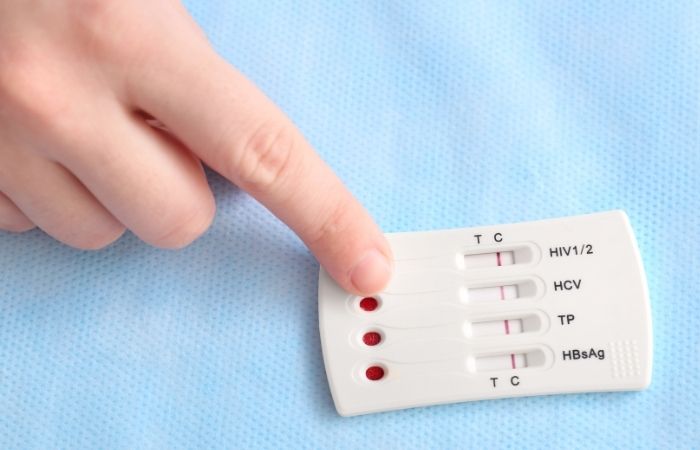
Not All Tests Are the Same: Rapid vs Lab Retesting
Not every test catches infections with the same speed or accuracy. Rapid at-home tests (like lateral flow devices) give fast results, but they may miss low viral loads or early-stage infections. They’re excellent for ongoing reassurance or for checking after the recommended window. But if you're in the early days post-exposure, you might need a more sensitive test, like a lab-based NAAT or PCR test.
Here’s how different tests stack up when you’re considering a retest:
Figure 2. STD test types compared for follow-up testing. Match the method to your timing and needs.
Bottom line? Retesting with a more sensitive method, or after more time has passed, can give you the confidence that your negative is truly negative. Don’t guess. Match the test to the timeline.
Can You Test Too Early? Yes, And Here’s What That Means
We all want answers fast. But testing before the infection can be detected doesn’t just waste time, it can give you a false sense of security. And for something like HIV, where early detection affects treatment success, that’s a big deal.
The “window period” is the most important (and most misunderstood) concept when it comes to retesting. It's different from the "incubation period," which is when symptoms might show. You can be contagious and test negative. You can feel fine and still be positive. That’s why follow-up testing exists.
If you're not sure whether you tested too soon, here's a simple rule of thumb: if it's been less than 14 days since your last exposure, and your result is negative, consider retesting at the 3-week and/or 3-month marks depending on the infection. The goal isn’t to scare you, it’s to catch what the first test might have missed.
Want a clear, science-backed way to calculate when to test again? Try our STD Window Period Calculator, it breaks down ideal timing based on your exposure date and test type.
Partner Exposure and Retesting Loops
One of the biggest reasons people need to retest? Their partner never got treated, or got reinfected. Even if you’ve done everything right, it only takes one untreated partner to start the cycle again.
That’s why the CDC recommends retesting for chlamydia and gonorrhea 3 months after treatment, even if you’re symptom-free. This isn't about blame. It’s biology. And for anyone who’s recently reconnected with an old partner or had multiple partners within a short time, retesting can help reset the baseline of your health.
If you’ve recently taken antibiotics but didn’t test, or if your partner took meds without seeing a doctor, your first test might miss low-level infections. The solution? Retest after the correct window or use a more sensitive kit. If you’re not sure where to start, STD Test Kits offers discreet, doctor-trusted options that don’t require a clinic visit.
People are also reading: Hepatitis B vs C: Which One You Should Worry About More, and Why
Need Privacy? Retesting Doesn’t Have to Be a Scene
We get it, going back to a clinic or explaining to a partner why you’re retesting can feel awkward. That’s why at-home options matter. You shouldn’t have to jump through hoops or feel embarrassed to double-check your health.
Today’s at-home kits are accurate, confidential, and arrive in plain packaging. No labels, no awkward pharmacy lines. Results stay with you, unless you choose to share them. If you’re planning to travel, live in a remote area, or just want more control over your health, testing from home gives you freedom. You can even set reminders to retest on your own schedule.
One reminder, though: if you're testing for HIV, syphilis, or herpes, and you're in a high-risk group, make sure to use kits that specify their window period. Some may miss early infections, especially for antibody-only tests.
What If the Retest Comes Back Positive?
Let’s talk about the moment no one wants to face, but many do. You thought you were in the clear. Then you retested. And now it’s positive. Whether it’s chlamydia, gonorrhea, HIV, or another infection, that result can hit like a gut punch, even if you felt prepared.
First, breathe. You didn’t do anything wrong. Most STDs are treatable. Some are even curable in one dose. And the earlier you catch them, the easier they are to manage. Testing isn’t a moral test, it’s a health decision. If your retest comes back positive, it means you did the right thing by double-checking.
Here’s what typically comes next: a healthcare provider may recommend a confirmatory test, especially for HIV or syphilis. Then treatment, if needed, antibiotics for bacterial infections, antivirals for viral ones. If your first test was too early and the second test caught the real result, you’re not “late”, you’re right on time.
Let’s look at Jordan’s story. He tested negative after a hookup with someone he met while traveling. No symptoms, all clear. But something kept bothering him, just a weird gut feeling. He retested a month later and found out he had gonorrhea. No judgment. Just relief that he caught it before symptoms kicked in or it spread to a new partner. That retest? It mattered.
Retesting = Responsibility, Not Paranoia
We live in a world where shame still clings to STDs. But let’s be clear, retesting isn’t something to feel embarrassed about. It’s a form of care. It means you’re paying attention to your body. It means you care about your partners. It means you're not afraid to face reality, even if it’s uncomfortable.
And if you're feeling overwhelmed? That’s normal too. The anxiety before a retest can be brutal. But the peace of mind that comes after? That’s worth everything.
Whether you’re retesting because of symptoms, a new exposure, or after treatment, you deserve clear answers. And if your partner is hesitant to retest, send them this article. Normalize it. Talk about it. Reclaim it.
If your last result left you with more questions than peace, don’t wait. Order a discreet combo test kit that checks for the most common STDs. No clinic lines, no awkward questions, just clarity.
How Retesting Protects Partners (and Your Future Self)
Retesting isn’t just for you, it’s for the people you care about, too. STDs often spread not because of intent, but because of delay. A false negative here, a missed window there. Then it jumps from person to person quietly, sometimes with no symptoms at all.
If you’re starting a new relationship, retesting gives you a clean slate. If you're rekindling things with an old partner, it offers reassurance. If you're poly, open, or dating casually, regular testing (and retesting when needed) is the most respectful move you can make.
You don’t have to announce every test you take. But you’ll feel better knowing you’re not passing on something you didn’t even know you had. And if the person you're sleeping with says they "just tested", it's okay to ask when and what for. Not all tests are the same. Not all testing is recent. Be kind, but be informed.
If you’re unsure what to say, start with this: "Hey, I like to keep things upfront. I recently got tested but want to double-check a few things, just to be safe. It’s nothing against you, I’d do this no matter what."
That kind of honesty? It builds trust. Not just with them, but with yourself.
When in Doubt, Retest (Here’s Why)
If you’ve read this far, you probably still have that nagging feeling, should I retest? Here’s your answer: if you’re even asking the question, it’s probably worth it. You don’t need a symptom to justify a follow-up. You don’t need a new partner. Sometimes, peace of mind is the only reason, and that’s enough.
Retesting is how we stay informed. It’s how we stay connected to our own bodies. It’s how we protect people we care about, even when things get messy. And with at-home options that are discreet, fast, and medically backed, there’s no reason not to know for sure.
If it’s been a few weeks since your last test, or something feels off, or you just want to be thorough, go for it. You’re not being extra. You’re being responsible.
Want help figuring out which test is right for your situation? Visit the STD Test Kits homepage for discreet, lab-grade kits you can use at home. Fast shipping. No judgment. Just answers.
FAQs
1. Can you really get a negative test result and still have an STD?
Yep. Happens more than you’d think. If you test during the “window period” , that awkward limbo before the infection shows up on tests , your result can come back negative even if you’re already infected. It’s not your fault. It’s just biology playing hide and seek. Retesting is how you catch it once it comes out of hiding.
2. How long should I wait before retesting after treatment?
For infections like chlamydia or gonorrhea, the golden rule is: retest around the 3-month mark. That gives your body time to clear the infection and avoids mistaking leftover bacteria for reinfection. Plus, if your partner didn’t get treated or you had sex again, you’ll want to double-check anyway. No shame in a retest , just smart follow-through.
3. My test said negative, but something still feels off. Should I trust my gut?
Listen , your body usually knows when something’s not right. If you’re still having symptoms (burning, discharge, weird bumps, even just a vibe that won’t quit), retest. False negatives happen. Or it could be something else entirely. Either way, your discomfort deserves answers, not second-guessing.
4. I took antibiotics before testing , could that mess with my results?
It can. If you took antibiotics recently (even for something random like a sinus infection or acne), they might suppress bacteria just enough to mess with your test. It’s like cleaning up before the inspector comes , not everything shows. If you were on meds and tested during or right after, it’s worth retesting when you're clear.
5. Do I need to retest if the only thing we did was oral?
Oral sex isn’t risk-free , especially with STDs like gonorrhea, herpes, and syphilis. If it was unprotected, and especially if it was with a new or unknown-status partner, retesting’s a good move. STDs don’t care if you call it “just oral.”
6. I already tested for HIV. Why do they want me to do it again?
Because HIV can take time to show up on tests , up to 90 days, depending on the type. If your first test was within a few weeks of exposure, it’s just too early to be 100% sure. Think of the follow-up as confirmation, not overkill. Peace of mind > panic loops.
7. How often should I be testing if I’m, you know… active?
If you’re having sex with new or multiple partners, aim for every 3–6 months. If you’re in a monogamous situation, once a year might do , but check in with your risk and your instincts. And anytime something changes (new partner, condom slip, symptoms), reset the clock and consider retesting.
8. If my partner tested negative, why should I retest?
Timing, babe. Maybe they tested too soon, or their test didn’t cover everything. Maybe they got exposed after their test. You’re not being dramatic by retesting , you’re being thorough. Your health doesn’t ride on someone else’s test result.
9. Does pregnancy change how often I should retest?
It does. Pregnant people usually get screened early, but if you’re at higher risk , new partner, symptoms, past infection your provider might test again in the third trimester. Certain STDs can affect birth outcomes, so it's not just about you anymore. It’s protective, not punishing.
10. I’m not sure which test to take , is there a one-size-fits-all option?
Honestly? The combo test kit is your best bet if you're looking to cover the basics. It screens for the most common STDs in one go, no guesswork. Especially useful if you're retesting and not sure what the exposure was , or if you just want to start fresh and be thorough.
You Deserve Answers, Not Assumptions
Retesting isn’t overreacting, it’s smart, informed, and protective. Whether your last test was early, your partner’s status is unclear, or something just doesn’t feel right, a second test could give you the peace of mind you’ve been waiting for. No one regrets catching something early, but plenty regret missing it.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
Centers for Disease Control and Prevention – STD Treatment Guidelines
Retesting for STIs After Treatment: Rates and Guidelines
Window Periods in Common STD Testing
Teen Vogue – What to Know About STD Testing
Healthline – When to Retest After an STD
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Darlene Ocampo, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.