How Accurate Is a Syphilis Rapid Test?
Quick Answer: A negative STD test result taken too early can miss an infection due to the “window period”, the time your body needs before a test can detect the STD. Retesting is often necessary to confirm results.
This Article Is for Anyone Who’s Ever Thought, “But What If It’s Wrong?”
STD testing is powerful. It saves lives, prevents transmission, and gives people the clarity they deserve. But it’s not magic. It has limits, and one of the biggest ones is timing. Whether you’re someone who just got tested after a risky night, a cautious partner doing routine screening, or someone experiencing confusing symptoms despite a negative result, this article is for you.
You’ll learn how STD tests actually work, why your first result might not be reliable, what “window period” really means, and what kinds of infections are most likely to sneak past an early test. We’ll also cover when to retest, what to do if your symptoms persist, and how to protect both your health and your peace of mind.
We’re not here to shame. We’re here to explain what’s real, because false negatives happen, and knowing when to test again is a form of self-protection, not paranoia.
People are also reading: STD Scare After Sharing a Towel? What to Know Before You Panic
What Is a False Negative STD Test?
A false negative means you were tested for an STD, got a negative result, but the infection was actually present, you just didn’t catch it yet. This can happen with many common STDs including chlamydia, gonorrhea, syphilis, and HIV. The test didn’t lie, it just wasn’t timed right.
Here’s the deal: no test can detect an infection the instant you’re exposed. Your body needs time to either replicate the pathogen (like bacteria or virus particles) or create an immune response (like antibodies). This delay is what we call the window period, and it’s different for every infection and test type.
Think of it like taking a pregnancy test the day after sex. It’s not that the test is bad, it’s that your body hasn’t had time to register anything yet.
Window Periods vs. Incubation Periods (And Why It Matters)
Let’s break it down: the window period is how long it takes before a test can detect an infection. The incubation period is how long it takes for symptoms (if any) to show up. And they’re not always the same.
For example, you might start showing signs of herpes within 4 days of exposure, but the antibodies that most tests look for don’t peak until 12 weeks later. That’s a recipe for confusion, and false reassurance.
Figure 1. Window vs. incubation periods vary widely between infections, timing your test correctly matters.
“I Trusted the Test. Then I Got the Call.”
Lina, 26, tested for STDs five days after a condom slipped during sex with a new partner. “I wanted answers fast. I had discharge, I was panicking. The test came back negative, and I tried to believe it,” she says. “But something didn’t feel right.”
“A week later, I got a call. My partner had tested positive for chlamydia. I retested immediately and it came back positive too.”
This is why early testing can be misleading. Not wrong, just premature. Lina did everything right. But the test wasn’t ready to catch the infection yet. It wasn’t her fault. It wasn’t the lab’s fault. It was just a matter of biology and time.
Some Tests Are More Likely to Miss an Early Infection
Not all STD tests detect infections the same way, or with the same sensitivity. The test type matters just as much as the timing. If you’re wondering why you tested negative but still feel off, the test itself might be part of the problem.
Here’s how common test methods compare when it comes to early detection and false negatives:
Figure 2. Some STD test types are more reliable early than others, but all require timing and context.
If you test too soon, especially with a rapid or antibody-only test, there’s a real chance you’ll walk away with a clean result that isn’t the full truth yet. That doesn’t mean the test is bad, it means your body hasn’t hit the detection threshold.
Mail-In, Rapid, or Clinic: Which Is Best for Catching an Early Infection?
Each testing method has its place, but when you’re worried about a recent exposure, accuracy and timing matter more than convenience.
Here’s how they compare when false negatives are a concern:
Figure 3. If your first test was a rapid, consider a follow-up lab-based NAAT or combo kit for better accuracy.
When Timing Really Matters: Risky Scenarios That Can Skew Results
False negatives don’t happen randomly. They tend to show up in specific types of scenarios, ones that involve early panic testing, unclear exposure windows, or recent treatment. Here's when to slow down and plan your testing window more carefully:
Same-day testing after unprotected sex. You want answers right now, but no test can detect infection within hours. You’ll need to wait at least a week (for chlamydia/gonorrhea) or longer for HIV or syphilis.
- You’re symptomatic but it’s only been 3 days. Early symptoms like burning or discharge may appear before your body produces enough bacteria, virus, or antibodies to test positive. False negatives are common in this zone.
- You were treated with antibiotics before testing. If you took antibiotics post-exposure (e.g., for a UTI or unrelated infection), they may suppress bacterial STDs enough to cause a negative result, even if the infection was present.
- You’re testing during a “check-in” phase with a new partner. Great idea, but make sure it's timed properly. If you had a new exposure within the last 2 weeks, retesting at the right time gives a more reliable picture.
Don’t Panic, Just Retest
Look, we get it. You saw that negative result and felt relieved, until your brain started whispering, “What if it’s wrong?” The good news is: this isn’t a mystery you have to live with. You just need to time it right, and test again.
If your first test was taken too early or was a low-sensitivity test, we recommend following up with a lab-backed, combo STD test that covers the most common infections with better accuracy. You can order a discreet at-home combo kit here, no clinic, no judgment, just clarity.
Worried you’re in the window period? Use the Window Period Guide to check if now is the best time to retest, or if you should wait for peak accuracy.
The Emotional Side of False Reassurance
There’s a specific kind of mental trap that happens after a negative test result. You want to believe it. You want it to be final. But something lingers, maybe it’s symptoms, maybe it’s guilt, maybe it’s just knowing the test came too soon.
This is where people start second-guessing everything. You feel silly for testing too early, but also frustrated that no one warned you. You wonder if your partner will believe you. You question whether your body is trustworthy. That’s not just medical confusion, that’s emotional fallout.
Let’s be clear: this isn’t your fault. Most people aren’t told how window periods work. Clinics don’t always explain the need for retesting. And the fear of STDs can make even the most rational person panic-test in the middle of the night.
If that’s you, you’re not alone. Getting a negative result that doesn’t feel trustworthy doesn’t make you paranoid. It makes you smart, and aware that your body deserves clarity, not rushed relief.
What to Say to a Partner When You’re Retesting
Let’s say you tested negative, but now you’re planning to test again, what does that mean for your partner(s)? Should you tell them? Should they test too?
Here’s what we recommend:
If you’re waiting to retest
Let your partner know that your first test might have been too early, and that you’re planning a follow-up. Suggest they test as well, especially if there was condomless contact. Use timing as the anchor, not blame. Try:
“I tested early after we hooked up, but I just learned some STDs take longer to show up. I’m testing again next week, and you might want to too.”
If symptoms appear while you wait
Pause sexual contact until you get answers. It’s not about punishment, it’s about protecting both of you. If you feel awkward, say:
“Something’s feeling off, and I’d rather be safe than sorry while I figure it out. Let’s take a short break and I’ll keep you in the loop.”
If your partner pressures you to stop testing or “trust the first result”
That’s a red flag. Respect goes both ways, and your decision to retest is about safety, not suspicion. You don’t need to justify wanting the truth.

People are also reading: Oral Thrush or Oral STD? What That White Tongue Really Means
FAQs
1. Why did my STD test come back negative even though I have symptoms?
Because tests aren’t magic wands, they have limits. If you tested too early, your body may not have produced enough bacteria, virus, or antibodies yet. It doesn’t mean your symptoms are in your head. It means you probably need to retest when the timing’s better.
2. How soon is too soon to test after unprotected sex?
Think of it like baking, pulling the cake out too early means it looks fine on the outside but isn’t fully done inside. For STDs, that means at least 7 days for chlamydia or gonorrhea, and 3+ weeks for things like HIV and syphilis. Test too soon, and you might miss it.
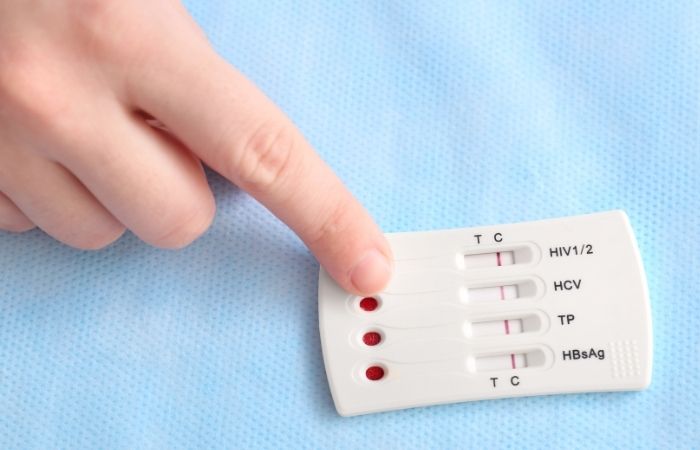
3. Can I trust a negative result from a rapid test?
If it’s been a few weeks since exposure, probably. If it’s only been a couple days? Not really. Rapid tests are great for convenience, but they’re not always great at catching early infections. Think of them like a snapshot, not the whole movie.
4. Wait, what exactly is the window period again?
It’s the awkward in-between phase where your body has been exposed, but hasn’t produced enough stuff for a test to catch it. Every STD has a different window. So yes, you could be infected and still test negative… for now. That’s the danger zone for false reassurance.
5. Can a false negative put someone else at risk?
Yeah. And that’s the tricky part. You might feel “cleared,” start hooking up again, and pass something on without knowing. That’s why we push retesting, not to scare you, but to protect everyone involved. Including you.
6. Do antibiotics mess with test results?
They can. Especially if you took them right after exposure. For example, antibiotics might suppress gonorrhea or chlamydia enough to dodge detection. So if your test comes back negative after a Z-pack, but something still feels off? Follow that gut and retest.
7. Should I stop having sex if I think my test was too early?
If you want to be responsible, yes, at least until you can retest. You don’t have to hole up like a monk. Just avoid high-risk stuff (like unprotected sex) until you’re in a better testing window. It’s a short pause for long-term peace of mind.
8. I tested negative for herpes, but I still have bumps. Now what?
That’s not unusual. Most herpes tests don’t check for the virus directly, they check for antibodies, which take time to build up. If you’ve got active sores, ask for a PCR swab test instead. Timing + method = better answers.
9. Can I test immediately after my first test?
You can, but unless enough time has passed, it won’t tell you anything new. The test will likely still say “negative,” and you’ll still be left guessing. Use our Window Period Guide to figure out when it’ll actually count.
10. How do I find out what kind of test I took?
Good question, because test type changes everything. If you tested at a clinic, call and ask. If it was at-home, check the box or the product page. If you're not sure? Go for a comprehensive combo test that covers all the big names with lab-grade accuracy.
Your Body Deserves a Second Look
We don’t say this to scare you. We say it because the science is real: first tests can miss things. Especially when taken too soon. Especially if the test wasn’t the most sensitive. Especially if symptoms don’t match the result.
You don’t have to live in limbo, or worse, push down your instincts just to “trust the test.”
If your last test didn’t feel final, you can do something about it. Try a discreet combo STD home test built for the most common bacterial and viral STDs. These rapid tests are designed to give quick answers, without clinic delays or awkward phone calls.
Need help deciding if now is the right time? Check out our window period guide to time your next move with confidence.
You don’t owe anyone silence. And you definitely don’t owe an STD a second chance to go undetected.
How We Sourced This Article: We combined current guidance from leading medical journals and diagnostic experts with plain-language breakdowns from STD counselors and community health providers. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
3. Sexually Transmitted Infections Treatment Guidelines, 2021 | CDC
4. Screening for Genital Herpes | CDC Testing | CDC
5. HIV Testing Fact Sheet | NIH HIVinfo
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to stop, find, and treat STIs. He combines clinical accuracy with a straightforward, sex-positive attitude and is dedicated to making his work available to more people, both in cities and in rural areas.
Reviewed by: L. Spencer, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.






