HIV Rapid Test Errors and Faint Lines: How to Know What’s Real
Quick Answer: The most accurate time to test for hepatitis B is 6–12 weeks after exposure. Some tests may detect the virus earlier, but testing before 21 days often leads to false negatives and may require a retest.
Who This Is For (And Why Waiting Can Feel Impossible)
This guide is for anyone who’s been exposed to blood or sexual fluids, recently or not, and now lives in that anxious in-between space. It’s for people who had unprotected sex during a weekend trip, shared razors with a roommate before knowing their status, or worried about a blood-stained glove at work. It’s also for those who feel fine, but have an unsettling gut feeling. Maybe someone told you afterward they’re not sure about their hep B status. Maybe your partner is vaccinated, but you’re not.
And if you’ve already tested, especially early, and got a negative result, this article will help you make sense of what that means, when to retest, and how hepatitis B testing works behind the scenes. Spoiler: Just because the test says “negative” doesn’t always mean you're in the clear yet.
We’re here to bring clarity without shame. Testing is a form of care, not confession. The only goal here is to help you understand when testing gives you answers you can trust.

People are also reading: Why HPV Rapid Tests Miss Early Infections
Understanding the Window Period vs Incubation Period
Here’s where most people get confused: the difference between incubation period and window period.
The incubation period is how long it takes for symptoms, if any, to appear after exposure. For hepatitis B, that can be anywhere from 6 weeks to 6 months. But most people never show symptoms at all, especially in the early phase. This is one reason hepatitis B spreads so silently.
The window period is different. It refers to the time between exposure and when a test can reliably detect infection. This is critical, because testing during the window period often produces false negatives, not because the test is broken, but because your body hasn’t made enough viral markers yet to be detected.
The virus could be replicating quietly in your system, but until there’s enough surface antigen (HBsAg), core antibody (anti-HBc), or viral DNA in your blood, the test result may come back as negative, even if you’re infected.
Let’s break that timing down further:
Table 1. Timeline of hepatitis B detection markers after exposure. This shows why testing too early can result in false negatives, your body simply hasn’t built up detectable levels yet.
If you test on day 7, it’s like trying to hear an echo before you’ve even yelled. The virus may be there, but the test can't “hear” it yet. That’s the danger of early negatives, they can create false relief.
Exposure Scenarios That Raise Red Flags
Let’s ground this in real situations. Because not all exposures are obvious, and many people aren’t sure what “counts.” Here are some lived examples:
Jake, 28, gay cis male
“I was at a bachelor party, hooked up with someone, and only found out after that he wasn’t sure about his hep B vax. We didn’t use protection. I tested the next morning. Negative.”
Jake’s story is common, and risky. Testing within 24 hours might rule out a pre-existing infection, but it tells you nothing about this new exposure. In his case, he needed to wait at least three weeks before a PCR test would be meaningful, and ideally, 6 to 8 weeks for the most accurate result using HBsAg or anti-HBc markers.
Monica, 36, healthcare worker
“I accidentally stuck myself drawing blood from a patient whose records were incomplete. My clinic tested me for everything that afternoon.”
For Monica, same-day testing provides a useful baseline, but not peace of mind. The exposure just happened. It takes time for the virus to replicate and show up in your blood. She should retest at 6 weeks and again at 12 weeks, even if she stays symptom-free.
Samir, 24, international student
“I found out my college roommate was living with chronic hep B. We shared razors and clippers. I never thought about it until now.”
This type of delayed exposure realization is more common than you think. For Samir, any shared blood-contact item counts as potential exposure. Because the exposure wasn’t a one-time event, and may have happened weeks ago, a test now could be meaningful, especially if it’s been more than six weeks. But if it hasn’t, retesting will still be needed to confirm status.
Testing Methods: What You’re Really Measuring
Not all tests are created equal, and that matters a lot when you’re testing for something with a long window period like hepatitis B. Whether you’re using a rapid home test, going to a clinic, or sending in a sample to a mail-in lab, what you’re actually testing for is either the virus itself or your body’s response to it. And both of those take time to build up after exposure.
Let’s unpack that.
Other tests search for antigens, virus components your body responds to. Antibodies are what your body creates to attempt to destroy an infection. Other tests, usually PCR tests done by a laboratory, search for virus genetic material directly. They may pick up an infection before your body even responds.
The problem is that those early-detection PCR tests aren't easy to find outside of hospitals or specialty clinics. Most public and private STD testing sites, as well as most at-home kits, look for HBsAg or anti-HBc markers. So you're still at the mercy of the window period.
The test you choose is important, but when you take it is even more so. To make things clearer, here's a breakdown:
Table 2. Common hepatitis B testing methods, timing, and reliability. Choosing a sensitive test too early still risks a false negative if the body hasn’t built up enough signal to be detected.
The bottom line? If you're under the 3-week mark, testing is unlikely to give you accurate results, unless you're in a hospital setting using a specialized DNA test. For most people, the 6–8 week range is the sweet spot where accuracy starts to peak, regardless of test type.
“But I Feel Fine”, The Danger of Silent Infections
One of the most dangerous myths around hepatitis B is that if you don’t feel sick, you must not be infected. The truth? Up to 70% of newly infected adults show no symptoms in the early weeks or months. And even when symptoms do appear, they’re often vague: fatigue, low appetite, mild fever, or stomach upset, easily mistaken for stress or a common bug.
Consider this: in one CDC analysis, almost two-thirds of people diagnosed with acute hepatitis B said they never had obvious signs of illness. Many of them only discovered the infection when applying for work-related health screening, preparing for immigration, or seeking care for something unrelated.
Here’s a quiet reality: hepatitis B doesn’t need your permission to cause damage. It can quietly inflame your liver while you live your normal life, unaware. That’s why timing matters so much. You may feel “safe” because you feel fine, but if you test too early and don’t retest, you could carry a silent infection forward without knowing.
And yes, that includes people who only had one hookup, one night, one slip.

People are also reading: When Is the Right Time to Get Tested for HPV?
The Negative Test That Wasn’t
Ella, 31, Brooklyn:
“It was a Tinder thing. We met for drinks, hooked up, and I didn’t think about it again until three days later when I found out he had been diagnosed with hepatitis B years ago. I freaked. I booked an urgent care test right away and was told I was fine. Negative. I moved on.”
Three months later, Ella started feeling off. Low energy. Strange yellow tint to her eyes. Bloodwork during a routine annual exam showed elevated liver enzymes, and a positive hepatitis B result. The early test she took had been too soon to detect the infection. The virus had been there the whole time, building silently.
This isn’t a horror story, it’s a common one. The moral? A negative result only matters when the timing is right. If you test too early, you may need to retest later. Otherwise, you risk trusting a result that wasn’t equipped to catch the infection yet.
If you’ve recently tested negative and the timing was within the first few weeks after exposure, don’t beat yourself up, but don’t stop there. Put a reminder in your phone to test again in 6 to 8 weeks. Testing isn’t just a one-time act. Sometimes it’s a two-step process.
False Negatives: How Common Are They?
Let’s get into the data. According to a 2023 NIH study, false negatives for HBsAg testing are most likely when performed within the first 21 days of exposure. The test sensitivity during this phase can be as low as 40%, depending on the individual's viral load. By week six, sensitivity jumps above 90%, and by week twelve, most tests reach near-total accuracy for surface antigens.
That’s a huge difference. Testing at day 10 and getting a negative result doesn’t mean “you’re safe.” It means “we might not be able to see it yet.” This is especially important for people with suppressed immune systems, pregnant people, or those on certain medications, as their immune responses can be delayed or blunted, further extending the window period.
In short: testing too soon is not just a waste of time, it can create a dangerous sense of safety.
If you’ve recently had a risk exposure and tested negative before the 6-week mark, the most reliable move is to retest at week 8 to 12. That’s where nearly all cases will show up, if infection occurred.
And if you’re panicking and need immediate answers? PCR testing through a clinic might be able to detect the virus sooner, but even then, it’s not foolproof. Your body and the virus don’t follow your calendar.
When to Retest (And Why It’s Not Overkill)
It’s normal to want one test to give you peace of mind. You test, it says negative, and you want to move on. But hepatitis B isn’t always that simple, especially if you tested during the early part of the window period. Retesting isn't about paranoia; it's about precision. Think of it as confirming the answer with better lighting.
Here’s how to know if you should test again:
If your initial test was taken within the first 3–4 weeks after a potential exposure, it may have missed the infection. Even if you used a high-quality rapid or lab-based test, there’s still a chance the virus hadn’t built up enough markers to be detected. Retesting at 6–8 weeks improves your odds of catching a recent infection by a huge margin.
If you’re immunocompromised, due to HIV, chemotherapy, or another condition, your immune system might not produce detectable antibodies or surface antigens as quickly. In these cases, some providers recommend retesting again at 12 weeks post-exposure to be sure.
If you’re pregnant or planning to become pregnant, retesting matters for both you and the baby. Vertical transmission (mother-to-child during birth) is one of the most serious routes of hepatitis B spread globally, and timely detection makes prevention possible.
And finally, if you’re still having unprotected sex with a potentially infected partner, or sharing items like razors or toothbrushes, your exposure risk is ongoing. In those cases, one negative test just marks the beginning of an ongoing monitoring process.
This timeline table can help clarify your next best step:
Table 3. Hepatitis B retesting timeline based on exposure. Waiting until your immune system has produced detectable markers is the key to avoiding false reassurance.
If your test was early and you still feel uncertain, it’s not “worrying too much” to test again. It’s called responsible follow-through, and in some cases, it can catch an infection before symptoms ever show up.
Where and How to Test (And How to Keep It Private)
Not everyone has easy access to a sexual health clinic, and not everyone wants to walk into one with their face exposed to the receptionist. That’s where at-home testing becomes more than convenient, it becomes empowering.
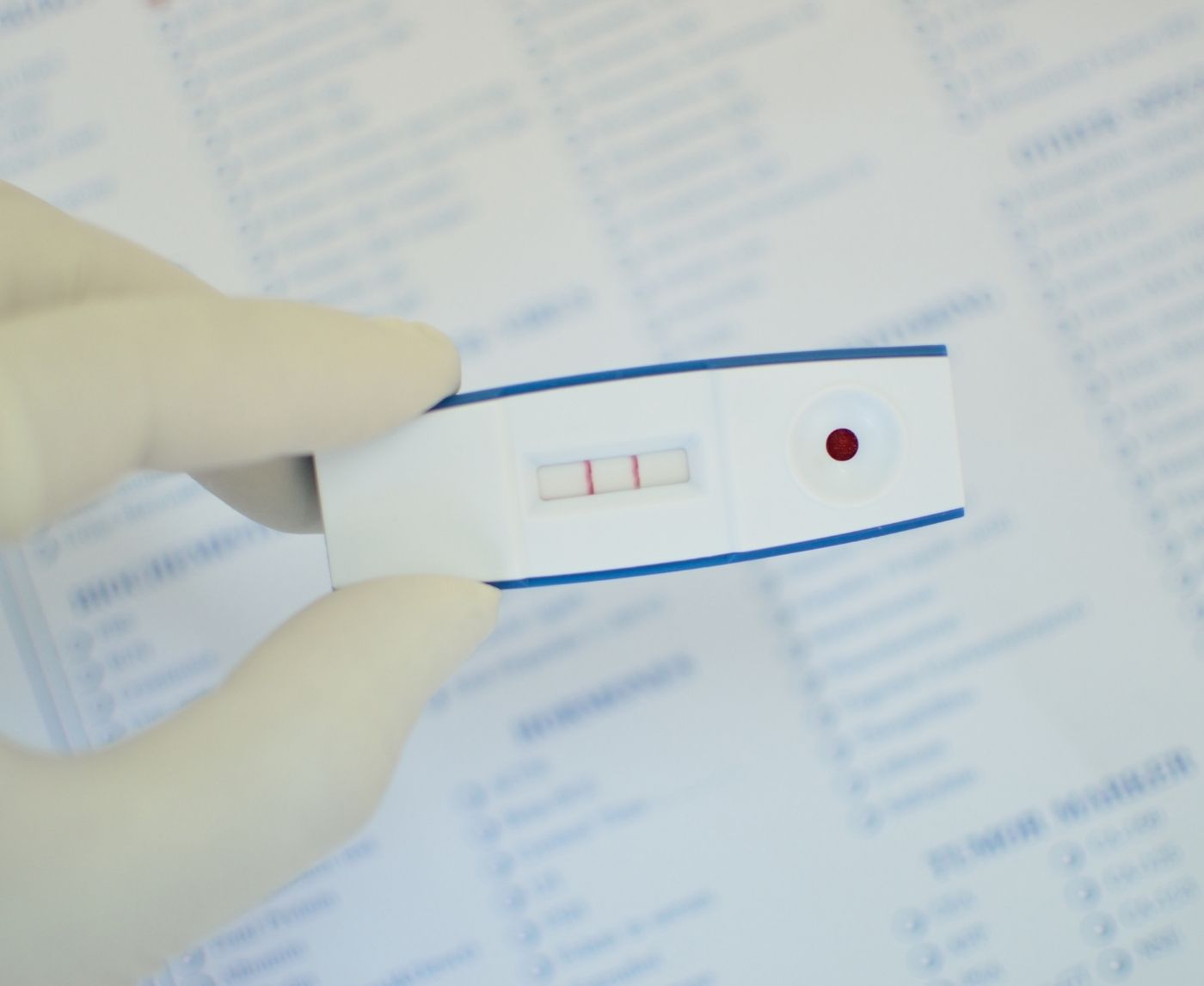
Modern STD Test Kits offer discreet shipping, no labels, and can be done in private. These rapid kits for hepatitis B detect the presence of surface antigens (HBsAg) and provide results within minutes, ideal for people who are past the 6-week mark and want a fast, confidential answer.
If you’re earlier than that, or want a deeper look (such as checking for core antibodies or viral DNA), a mail-in lab test or clinic PCR option may be better. But no matter what you choose, timing is still the most important variable. Even the best test in the world won’t detect something your body hasn’t built up yet.
If your head is spinning and you're not sure which test to pick, remember this:
You’re allowed to pause. You’re allowed to wait for the right time. And when that time comes, you deserve answers that mean something.
Don’t stay in guessing mode. This discreet combo test kit includes hepatitis B and other common STDs, all from one sample. You test at home, in your space, on your schedule.

People are also reading: Faint Lines, False Negatives, and Trichomoniasis: What You Need to Know
Symptoms or No Symptoms: You Still Need Timing
Maybe you’ve started feeling off. You’re tired, your appetite’s weird, your urine’s darker than usual. These might be early symptoms of hepatitis B, but they might also be nothing. Or something else entirely. The frustrating part is that symptoms don’t override the window period.
Even if you have symptoms, if you test too early, your test could still miss the infection. This is especially true with antibody-based testing, which depends on your immune system doing its job on a specific timeline. The same goes for people with zero symptoms. You can be silently infected and still test negative during the window.
That’s why the best strategy is a combined one: test at a medically appropriate time, pay attention to your body, and always follow up if something doesn’t feel right, even if the first result said “negative.”
The test doesn’t know your story. But you do. If something doesn’t sit right in your gut, listen. Wait a few weeks, and test again. You’re not overreacting, you’re being responsible.
What If Your First Test Was Negative, But Now You’re Scared?
Let’s say you tested at 10 days. Negative. But now it’s week five, and you’re still worried. Or maybe you got new symptoms. Or maybe the person you were with just told you they’ve had hepatitis B in the past and didn’t think to tell you sooner.
Here’s the move: get tested again. The second test is not a sign of distrust, it’s a sign of wisdom. Your original result wasn’t wrong; it was just early. This next test is your safety net. And it might be the one that actually gives you a clear answer.
You don’t need to explain this to anyone. You don’t need to justify why you’re testing again. Your health is your business. Your fear is valid. Your choice to follow through, even if it’s awkward or expensive or inconvenient, is what protection looks like in real life.
What If You Test Positive?
First: breathe. A positive result for hepatitis B is not the end of anything, it’s the beginning of a clear, informed next step. Millions of people live full, healthy lives with hep B. Many clear the virus naturally. Others manage it with simple monitoring or medication. Either way, you're not alone, and you're not doomed.
The first step is confirming your result. Depending on the test type, a follow-up test might be recommended, especially if you used a rapid antigen-only kit. Confirmatory testing usually includes additional markers like anti-HBc IgM and sometimes viral load measurement (HBV DNA) to determine if the infection is recent, active, or chronic.
Next, connect with a healthcare provider, telehealth, community clinic, your PCP, or a local sexual health center. You’ll likely be guided through more blood work to assess liver function, infection phase, and whether treatment is needed.
Andres, 40, tested positive on a home test and sat in his car in shock. He’d only gotten tested to “prove he was fine” for a new partner. That moment of fear turned into a follow-up doctor visit, and he learned his case was inactive and didn’t need treatment, just monitoring.
“It actually gave me peace of mind,” he later said. “At least now I know.”
Your story doesn’t end with a test. It begins with the choice to care for yourself, your partners, and your future health. Knowing is better than not knowing. And doing something about it? That’s power.
FAQs
1. Can I test for hepatitis B the next day?
Technically, yes, you can take a test anytime. But should you? Not really. If you test the day after a risky hookup or needle prick, odds are the virus hasn’t had time to show up in your blood yet. You might feel like you're “doing the right thing,” but an early test often gives you a false sense of safety. You’ll likely need to test again in a few weeks for anything to be conclusive.
2. When is the best time to test for hepatitis B after exposure?
Think of 6 to 8 weeks as the golden zone. That’s when most standard tests (like HBsAg and anti-HBc) become accurate enough to trust. Some people test at 4 weeks and catch it, but that depends on your immune system and the type of test used. If you’re testing earlier, plan a second round, just to be sure.
3. What if I feel totally fine, should I still get tested?
Yes, and here’s why: hepatitis B often doesn’t throw obvious symptoms, especially in the early stage. You could have the virus quietly working on your liver while you’re out living your life like nothing’s wrong. No fever, no rash, no nausea, nothing. That’s what makes it sneaky. Silence doesn’t equal safety.
4. Isn’t the incubation period the same thing as the window period?
Close, but no. The incubation period is how long it takes for symptoms (if any) to appear. The window period is how long before a test can reliably detect the virus. You can be well within your window period, feeling great, and still be infectious, even if your test says “negative.” Tricky, right?
5. How accurate are those home hepatitis B test kits?
Pretty solid, if you use them at the right time. Rapid HBsAg kits (like the ones we offer) are over 90% accurate when taken 6+ weeks after exposure. Before that, though? Accuracy drops fast. A fancy test used too early is still just a fancy blindfold.
6. I tested negative at 3 weeks. Am I in the clear?
Not yet. Three weeks is too early for most people. Even if your test was negative, your body may not have produced enough antigens or antibodies yet. The real confirmation comes around weeks 6 to 12. It’s like checking if cookies are baked when they’ve only been in the oven for five minutes, give it time.
7. Can I get hep B from oral sex?
It’s not the most common route, but it’s not impossible either, especially if blood is involved (cuts, sores, gum disease). Vaginal and anal sex are higher risk, but if there was any blood-to-blood contact, transmission risk goes up. So yeah, oral is lower risk, but not zero.
8. If I get vaccinated right after exposure, will it protect me?
Maybe, if you act fast. There’s something called post-exposure prophylaxis (PEP) for hepatitis B, basically a combo of the vaccine plus immune globulin (HBIG). It works best when given within 24 to 48 hours. If you're reading this days later, talk to a provider ASAP. Timing is everything.
9. I’m pregnant, does that change the testing timeline?
It might. If you're pregnant, early detection matters even more to prevent passing the virus to your baby during birth. The testing timeline is similar, but your doctor may monitor you more closely or test at multiple points. Don’t wait, this is one of those times when knowledge truly is power.
10. If I test positive, does that mean I’ll have hepatitis B forever?
Not necessarily. If you caught it as an adult, there’s a good chance your immune system will clear it on its own. But some people develop chronic hepatitis B, which sticks around. Either way, the next step is a follow-up test to see what kind of infection you’re dealing with, and what to do about it.
You Deserve Answers, Not Assumptions
False negatives happen. Not because you did something wrong, but because hepatitis B plays the long game. It hides. It waits. It builds up quietly. And testing too early is like checking a cake before it’s had time to rise, you’ll get no result, and maybe make bad decisions based on that.
The good news? Now you know better. You know when to test. You know why waiting matters. And you know where to turn if you need to test again.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. WHO – Hepatitis B Fact Sheet
2. Mayo Clinic – Hepatitis B Overview
3. Hepatitis B Foundation – Understanding Diagnostic Tests
4. CDC — Clinical Overview of Hepatitis B
5. CDC — Screening and Testing for Hepatitis B Virus Infection
6. CDC — Viral Hepatitis in STI Treatment Guidelines
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to stop, diagnose, and treat STIs. He combines clinical accuracy with a straightforward, sex-positive attitude and wants to make it easier for people in both cities and rural areas to read his work.
Reviewed by: Marissa Tang, MPH | Last medical review: October 2025
This article is meant to give you information, not medical advice.