My STD Symptoms Vanished. Was I Cured, Or Just Lucky?
Quick Answer: You’re very unlikely to get an STD from a towel. Most STDs need direct skin-to-skin or sexual contact to spread. But some skin infections and rare exceptions exist, testing is only needed if symptoms appear or exposure was higher risk.
Why This Fear Happens (And Who It Hits the Hardest)
This kind of worry usually strikes in the quiet moments, after a hookup, during a trip, or when you’re staying with friends or a partner. For Sam, 27, the fear hit after borrowing a towel from a housemate during a weekend away. "It smelled fine. But later, I realized it might've been used after sex. My skin started tingling just thinking about it."
These moments are often wrapped in shame and uncertainty. Maybe you were raised with strict hygiene rules. Maybe you’re newly sexually active. Or maybe you’ve had an STD scare before and never want to feel that again. This article is for you, the anxious researcher, the overthinker, the cautious partner, who just wants clear, judgment-free answers.
We’ll walk through what can and can’t survive on towels, what kinds of infections might show up, how long different pathogens live on fabric, when testing makes sense, and what your next steps should be.

People are also reading: Oral Thrush or Oral STD? What That White Tongue Really Means
Can You Get an STD from a Towel?
Most sexually transmitted diseases (like gonorrhea, chlamydia, HIV, and syphilis) do not survive long outside the human body. They need moisture, heat, and direct mucosal contact to spread. A dry towel in a room-temperature environment? Not their ideal habitat.
However, a few exceptions exist, especially when the towel is freshly used and damp. Some infections that might linger on towels or shared linens include:
Figure 1. Some skin and parasitic infections may spread through shared towels, but traditional STDs almost never do.
So no, you’re not going to get HIV from a towel. But something itchy, like molluscum or a fungal rash? That’s a different story. Which brings us to a key question, how long do these bugs actually survive on fabric?
How Long Can STDs and Skin Infections Live on Towels?
Here’s the breakdown based on research from the CDC, peer-reviewed journals, and expert reviews:
Figure 2. Environmental survivability varies by organism, but time, moisture, and direct contact matter most.
Bottom line? Most organisms die fast outside the body. But towels that are freshly used and still moist can carry very low, but not zero, risk for certain conditions. Let’s now walk through whether and when you should actually consider getting tested.
When to Test (And When Not To)
If you shared a towel and are now spiraling, pause. In almost every case, you do not need STD testing from towel exposure alone. The risk for classic STDs like chlamydia, gonorrhea, syphilis, and HIV is virtually nonexistent without direct sexual contact or blood exposure.
But what if your towel sharing happened after sex? Or you used a towel immediately after someone else with an active outbreak? In those edge cases, testing may be reasonable, but still not urgent unless symptoms appear.
Use this simple guideline:
Figure 3. General testing decision logic after shared towel exposure.
STD or Something Else? Skin Symptoms That Confuse People
This is where most panic spirals begin. You shared a towel, then a few days later, you notice itching, redness, or a bump. Your brain fills in the blanks: STD.
But here's the catch: the most common skin problems that happen after sharing towels aren't STDs. They could be fungal infections, allergic reactions, or irritation from rubbing against something wet. Still, they look so much like STDs that even doctors can be fooled at first glance.
Here are some examples of common misdiagnoses:
Figure 4. Non-STD skin symptoms that often trigger STD fear.
If you’re unsure, it’s okay to test. But it’s also okay to wait a few days and see if symptoms resolve with hygiene and over-the-counter antifungal creams. You’re not dirty. You’re not reckless. You’re human, and human skin reacts to a lot of things.
“I Got a False Positive After Panicking”
Jordan, 34, tested for trichomoniasis two days after sharing a towel at the gym that he later realized was damp. He was terrified, Googled everything, and convinced himself something was off when he started feeling itchy.
“It was nonstop. I kept checking myself, googling images. I found this one picture of a guy with herpes and thought, ‘That’s it. I have it.’”
He used an at-home test early, and got a faint line that scared him. But a lab confirmation a week later was completely negative. His rash? It turned out to be from laundry detergent in the towel, not an STD.
This is why timing, symptom observation, and emotional calm matter before rushing to test. False positives and unnecessary anxiety are real risks, too.
Your Options If You Still Want to Test
Even if the science says “you’re probably fine,” anxiety doesn’t always listen to science. Sometimes the peace of mind is worth the test. And that’s okay.
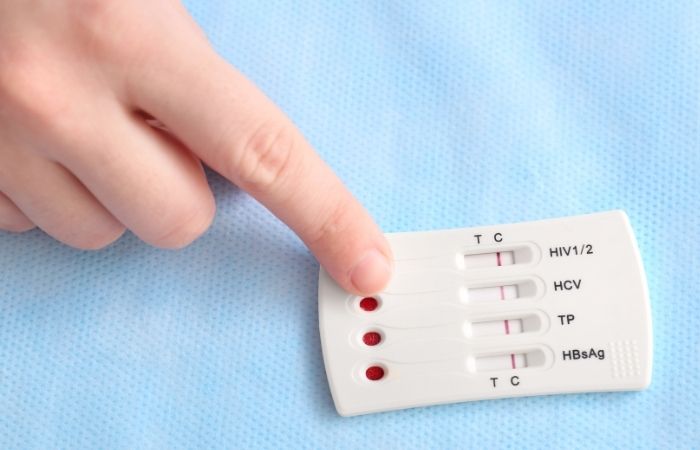
If it’s been a few days since the towel scare and you’re still anxious, you can try a discreet, fast at-home test kit. You’ll want to time it right, this combo kit checks for the most common infections and can give answers in minutes.
Remember: most rapid STD kits check for antibodies or antigens, not active skin conditions like fungal rashes or molluscum. But they’re great if you had a hookup, feel unsure, or want baseline peace of mind.
Whether it's a bump or a question mark, this FDA-approved home test can help you breathe easier.
Cleaning, Disinfecting, and Real Hygiene That Matters
Shared towels are more of a hygiene worry than a classic STD threat. Damp fabric can host bacteria, yeast, and skin pathogens longer than dry surfaces because they thrive in moisture. That’s why gyms, public pools, and dorm bathrooms are notorious breeding grounds for rashes and fungal infections, just not classical STDs like chlamydia or HIV.
Here’s what you should actually do when towels are involved:
Cloths and towels carry moisture long after use, and moist environments are the enemy of clean skin. Whether it’s a workout towel or a beach towel, the best prevention is personal use and proper laundering.
How to Think About Risk Like a Pro
Let’s take the guesswork out of “Do I need to test after this?” and replace it with science and strategy.
Experts often use a risk checker or quiz to help decide what level of testing is appropriate, especially after uncertain exposures. These tools ask about direct contact, symptoms, condom use, partner status, and timing. The goal isn’t to induce panic; it’s to clarify whether your situation is genuinely high‑risk or just anxiety‑driven.
To give you an idea of how risk assessment works: a scenario that might recommend testing includes ANY direct genital contact (sex, oral/genital contact), a known positive partner, or shared needles, not the indirect transfer that comes from a towel. That’s fundamentally different from the towel panic that brought you here.
Why Testing Timing Matters (Window Periods Explained)
If you do decide that testing makes sense, for example, because of a sexual encounter or other exposure, then timing matters. Every STD has a “window period,” the time between exposure and when a test can reliably detect infection.
Testing too early can lead to a false negative, not because the test is bad, but because your body hasn’t had time to show enough markers yet. Here’s a simplified overview of window periods for common STDs many readers search for:
Figure 5. Window periods vary by infection and type of test. Testing too early risks false reassurance.
Every STD is different. For example, antibody tests in HIV may not show up until 6–12 weeks post‑exposure on some platforms, while nucleic acid tests (NAAT) for bacterial STDs like chlamydia or gonorrhea become accurate sooner.
So if your exposure involves a situation that actually matters (not towels), planning your test based on these windows will give you the most accurate answers.
Stigma‑Free Hygiene and Boundary Conversations
Let’s be honest: sharing towels isn’t sexy to talk about. But being open about how you manage personal items with partners and roommates is part of respectful, adult hygiene. Setting boundaries like “I prefer fresh towels only” or “let’s keep different towels for body and face” doesn’t make you paranoid, it makes you informed.
Talking about hygiene doesn’t mean you assume someone is “dirty.” It simply means you care about both your health and theirs. And that applies to shared bathrooms, laundry practices, and yes, towels.
If you’re nervous about broaching the subject with a partner or friend, here’s a simple script you can adapt:
“Hey, I’m trying to be careful about hygiene since I’ve had some scares in the past. Would you mind if we each used our own towels and kept them separate?”
Safe Testing Options for Low‑Anxiety Answers
If you’re still feeling uneasy, even after understanding risk and timing, that’s okay. Peace of mind is a valid reason to test. And you don’t have to walk into a clinic to do it. Discreet at‑home tests allow you to check for multiple infections in minutes or a few days, without public interaction.
For example, a home combo STD test can screen for chlamydia, gonorrhea, syphilis, HIV, and more with high accuracy once the appropriate window periods have passed. This way, you’re in control of your health on your schedule.
People are also reading: What Happens If You Don’t Treat Chlamydia or Gonorrhea?
FAQs
1. Can I actually catch an STD from a towel, or is that just internet fear?
It’s mostly fear. STDs like chlamydia, gonorrhea, and HIV need direct body-to-body contact, moist mucosal stuff, not a dry towel. Think skin-to-skin, not terry cloth-to-skin. That said, some skin infections like fungal rashes or molluscum contagiosum can technically hang out on damp fabric for a bit. But it’s rare. Really rare.
2. What about herpes? Doesn’t that live on surfaces?
Not in any meaningful way. Herpes is a fragile virus, think drama queen with a short fuse. It breaks down quickly outside the body. Unless the towel was immediately used on an open sore and then directly rubbed on your mucous membranes… you’re in the clear. It’s not lurking in your beach towel from last week.
3. I used a towel at someone else’s house and now I’m itchy. Should I panic?
Nope. Your skin might just be mad about detergent, leftover soap, friction, or even humidity. Itching doesn’t mean STD. It means your body is reacting to something. Keep it clean, wear loose clothes, and give it 24–48 hours. If the itch turns into a rash or bumps, then it’s worth checking in, still not necessarily an STD, though.
4. Could pubic lice live on a towel?
Yeah, they could. Those little suckers (literally) can hang out on fabric for a day or two. But pubic lice are way more commonly spread through close, hairy-body contact, not from sharing a hand towel after washing your face. And they’re visible, treatable, and honestly more annoying than dangerous.
5. How long do germs from STDs last on fabric?
It depends on the germ. Trichomonas microbes can live for 30 to 45 minutes on a moist towel. Fungi and molluscum contagiousum remain alive longer, especially in a wet locker room or sauna. However, the vast majority of bacteria and viruses that cause STDs will quickly perish in the dry air of your own bathroom.
6. Do I need to get tested if I used a hotel towel?
If that’s your only concern, just a towel, then no, testing isn’t needed. But if you also had sex during that trip, or you're feeling off, then testing might still make sense. It's about the full exposure picture, not just the towel drama.
7. Can sharing towels with my partner be risky if we’re both clean?
Nah. If you’re both recently tested and symptom-free, towel sharing is more of a “whose side of the bathroom is this?” debate than a health hazard. Just don’t reuse the same towel if someone’s got a rash, yeast infection, or weird mystery bumps, because those are more likely to spread than any actual STD.
8. Why do people still think you can get STDs from towels or toilets?
Because fear is sticky. And because no one teaches us the difference between skin infections and actual sexually transmitted diseases. Spoiler: STD stands for sexually transmitted. A damp towel doesn’t count as sex. But it might explain a funky rash if someone else used it on their junk.
9. What if I feel fine but still can’t stop worrying?
That is fair. Anxiety does not always care about logic. If testing is what gets you into bed tonight, do it. Go buy a home combination test kit, wait for the proper window of opportunity, and lay your worries to rest. Health care is more about infection, but it is also about clarity.
10. How do I know when to actually test?
Great question, and there’s a quiz for that. Head over to our STD Risk Checker to figure out your next move. If your towel scare was part of a bigger picture, like a new hookup or a symptom, you’ll know exactly when and what to test for. Otherwise? Take the win and skip the panic.
You Deserve Facts, Not Fear
If you’re reading this with anxiety in your chest and a search tab full of worst-case scenarios, pause. Take a breath. Towels aren’t the threat we’ve been made to believe. Most of the time, the panic is louder than the science. But your peace of mind matters too.
Whether you're reacting to a towel, a rash, or an "I don't know" moment, getting clear answers can stop the mental spiral. Try a discreet combo STD home test if you need certainty, because clarity shouldn’t require shame or a clinic visit.
And remember: health doesn’t mean never worrying. It means knowing when to worry, and when to let go.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Sexually Transmitted Diseases (STDs) – Symptoms & Causes | Mayo Clinic
2. STI Transmission Myths – Health Promotion Ireland
3. Can I Get Any STDs Through Clothing? | MedicineNet
4. Trichomoniasis and Nonsexual Transmission via Fomites – PMC
6. Can You Get Herpes from a Dirty Towel? | Healthline
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: L. Spencer, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.






