6 STDs You Can Catch From Oral, Even If It Feels “Low Risk”
Quick Answer: White patches, sore throat, or swollen glands after oral sex may signal oral thrush, gonorrhea, chlamydia, or syphilis. Testing is the only way to know for sure, especially if symptoms persist beyond 3–5 days.
Who This Article Is For (And Why It Matters)
This guide is for anyone who’s looked in the mirror and wondered: “Is this normal?” Whether you’ve just had oral sex for the first time, tried something new with a long-term partner, or are dealing with a mystery sore throat no one can explain, you’re not alone. White tongue and mouth symptoms after oral sex are often dismissed as stress, allergies, or a mild infection, but they can also be early signs of a transmissible STD.
We’re not here to shame. We’re here to decode what your body might be telling you, and how to figure out if that weird taste or patchy tongue is just a passing annoyance, or something you should test for. Because here’s the truth: oral sex can transmit chlamydia, gonorrhea, syphilis, herpes, and even HIV in rare cases. Many of them show up first in the mouth, long before symptoms appear anywhere else.
People are also reading: Feel Totally Normal? That Doesn’t Mean You’re STD-Free
“I Thought It Was Strep, Turns Out It Was Gonorrhea”
Marcus, 28, had just started seeing someone new. After a weekend together, he noticed a sore throat that didn’t go away. “It felt like strep, but I didn’t have a fever,” he said. “Then I noticed these tiny white dots on the back of my throat and this weird breath smell, even after brushing.” He assumed it was just post-hookup fatigue, but five days later, his glands were swollen and swallowing hurt.
“I went to urgent care, and they swabbed for strep. It came back negative. That’s when the nurse asked if I’d had oral sex recently. When I said yes, she added a throat swab for gonorrhea.”
Marcus was shocked when the result came back positive. “I didn’t even know you could get gonorrhea in your throat.” After a single antibiotic injection, his symptoms cleared in 48 hours.
“If they hadn’t asked about oral sex, I would’ve never thought to get tested. I could’ve passed it on without knowing.”
Marcus’s story is common. Up to 90% of oral STDs show no obvious symptoms, or get mistaken for something else entirely.
White Patches, Sore Throat, Swollen Glands: What Do They Actually Mean?
Let’s decode what these symptoms could actually point to. Spoiler: not all of them are STDs, but when they are, you’ll want to know early.
Table 1. Common mouth and throat symptoms after oral sex, and what they could mean. Always test if symptoms persist beyond 3–5 days or feel unusual for you.
Why Oral STDs Get Missed (And Why That’s a Problem)
Oral STDs are notoriously sneaky. They often mimic harmless conditions like allergies or dry mouth. Here’s why so many people overlook them:
First, most clinics don’t automatically test your throat unless you specifically ask, or disclose that you’ve had oral sex. Second, a lot of people assume that condoms only matter for penetrative sex. But you can absolutely get an STD from giving oral, especially if there are cuts, dental work, or irritation in your mouth.
Third, some STDs like chlamydia or gonorrhea can live in the throat without causing pain. But they’re still infectious, and can be passed on through kissing or oral again.
If you’ve recently given oral sex and now have strange mouth symptoms, even if mild, it’s smart to test. You may catch something early and prevent it from spreading.
When Do Oral STD Symptoms Start Showing?
If you’re wondering how fast something could show up in your mouth after oral sex, the answer depends on the infection, and your immune response. Some symptoms can appear in 1–3 days, while others take a week or longer. But here’s the tricky part: many don’t show up at all.
Here’s a breakdown of typical symptom timelines for common oral STDs:
Table 2. Estimated symptom timelines for oral infections after exposure. Lack of symptoms doesn't mean you’re clear, many oral STDs remain silent but still transmissible.
If you're experiencing white tongue or a sore throat within a few days of giving oral, it's worth watching the timeline. If symptoms persist beyond five days or worsen, it's time to test, especially if you're unsure about your partner's status or recent exposure.
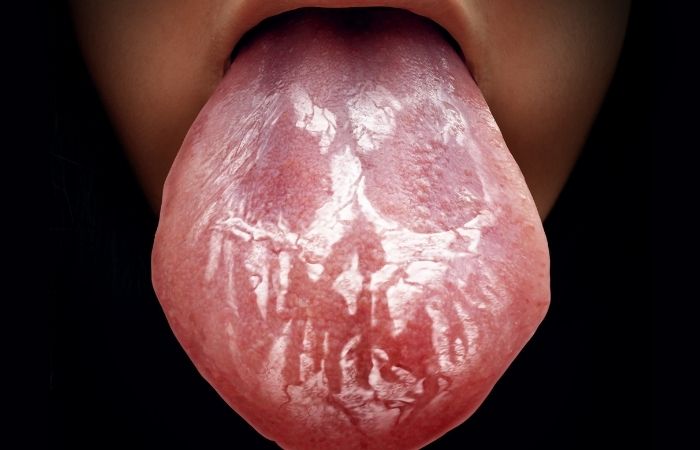
Oral Thrush vs Oral STD: How Can You Tell?
This is the million-dollar question. Many people panic when they see white patches on their tongue or inner cheeks and assume it's an STD. Others assume it’s just oral thrush and treat it with over-the-counter antifungals, only to find it keeps coming back.
Here’s how to start sorting it out:
Oral thrush (candida) is a yeast infection, not an STD, but it can develop after antibiotic use, illness, or after oral sex if the body’s defenses are down. It typically causes:
- Thick, white coating on tongue and cheeks that may scrape off
- Burning or metallic taste
- Dry mouth or cracks in corners of lips
Oral gonorrhea or chlamydia may cause:
- Mild sore throat that doesn’t go away
- White or yellowish spots on the tonsils
- Bad breath or unusual taste
Syphilis may start with:
- Painless sore or ulcer (chancre) in the mouth
- Swollen lymph nodes in the neck
- Later, rash or fever if untreated
If you’ve never had oral thrush before, or the white patches aren’t going away with standard treatment, get tested for oral STDs. Especially if you gave unprotected oral to someone new within the past 2–3 weeks.
Can You Really Get an STD from Giving Oral?
Yes, giving oral sex without protection can expose you to a range of STDs. Here’s what people often don’t realize:
Your mouth is lined with delicate tissue. Microscopic tears from brushing, flossing, or even spicy food can create entry points for bacteria and viruses. STDs don’t care if it’s “just oral.”
The following are commonly transmitted through oral sex:
- Gonorrhea – very common in the throat, often asymptomatic
- Chlamydia – can infect the throat, though less common
- Herpes (HSV-1 or HSV-2) – can be spread even without visible sores
- Syphilis – early lesions often occur in the mouth
- HPV – especially strains linked to throat cancer
In rare cases, HIV transmission via oral sex is possible, especially if open sores or bleeding gums are involved, but it’s much less common compared to other STDs.
So yes, it’s possible. But it’s also very preventable, with regular testing, barrier use (like dental dams or condoms), and recognizing when symptoms mean it’s time to act.

People are also reading: Why Does My STD Keep Coming Back? (And What to Do About It)
Testing for Oral STDs: What Are Your Options?
Think your sore throat might be more than just a cold? You don’t have to guess. Testing options for oral STDs include:
1. Throat Swab NAAT (Nucleic Acid Amplification Test): This is the gold standard for detecting oral chlamydia and gonorrhea. It’s painless, quick, and can be done at a clinic, or with some mail-in kits.
2. Blood Tests: Used to detect syphilis, HIV, and sometimes herpes antibodies. Best when done after the typical window period (14–90 days depending on infection).
3. At-Home Rapid Test Kits: Available for many STDs, including herpes, HIV, and syphilis. Some do not cover throat infections specifically, so look for options that allow oral sample collection or follow up with a clinic if throat symptoms persist.
If you’re feeling overwhelmed, don’t worry. You can start with a combo STD test kit that screens for multiple infections from home, quickly, discreetly, and without judgment. Order a combo STD test here.
Peace of mind is often just one test away.
Myths About Oral Sex and STDs That Keep People in the Dark
One of the biggest reasons oral STDs get missed? The myths people still believe. Even among sexually active adults, there’s massive confusion about what’s “safe” and what’s not. Let’s clear up a few of the most dangerous myths:
“Oral sex is safe sex.” Not exactly. It’s lower risk for HIV compared to penetrative sex, but not low risk for chlamydia, gonorrhea, herpes, or syphilis. These all transmit through skin, saliva, or mucosal contact, exactly what oral sex involves.
“If I don’t have symptoms, I’m fine.” False. Up to 90% of people with oral gonorrhea have no symptoms. Silent infections are still contagious, and can spread between partners through kissing or more oral sex.
“Only people with lots of partners get STDs.” Wrong again. STDs don’t discriminate by partner count. All it takes is one encounter without protection, especially with an asymptomatic carrier.
“You can’t get an STD from giving oral if they didn’t finish.” Also false. Semen, vaginal fluids, pre-cum, and even skin-to-skin contact carry infection risks, even if there’s no ejaculation.
It’s not about being reckless or dirty, it’s about biology. Understanding these myths helps you protect yourself and your partners without shame or blame.
While You Wait for Results: What to Do (and Not Do)
If you’ve ordered a test or are heading to a clinic, the waiting can feel like torture. Here’s what to do while you wait, and what to avoid:
- Don’t self-diagnose or Google obsessively. Online images can be terrifying and misleading. Your symptoms might not look textbook, and that’s okay.
- Do take photos if possible. If you notice sores, white patches, or changes, document them. Oral symptoms can fade quickly. This helps clinicians (or you) track progress.
- Avoid sexual contact until you get results. If you’re dealing with a possible STD, even without symptoms, it’s best to pause sexual activity to protect others and avoid reinfection.
- Rinse gently but don’t overdo it. Mouthwash or salt water can help, but don’t scrub or scrape white patches, they could worsen irritation.
And remember: you’re doing the right thing. Testing isn’t overreacting, it’s proactive, powerful, and protective.
How to Talk to a Partner About Oral STD Risk
This might be the most uncomfortable part, but it’s also one of the most important. If you’ve recently had oral sex and now have concerning symptoms, telling your partner can feel terrifying. Here’s how to make it less so:
Start with honesty, not accusation. You can say:
“Hey, I noticed some mouth symptoms after we were together. I’m not saying anything for sure, but I’m getting tested just in case, and I think it’s smart if you consider it too.”
Frame it as a mutual health conversation, not a blame game. You’re not pointing fingers, you’re protecting both of you.
If you do test positive, many clinics and at-home test providers offer anonymous partner notification tools. Some even send a message without revealing your name, letting the other person know they’ve been exposed and should test.
And if they react with anger or shame? That says more about them than about you. You’ve done the brave thing by choosing health over silence.
FAQs
1. Can you really get an STD just from giving oral?
Yeah, you can. It’s one of those uncomfortable truths most sex ed skipped. Bacteria like gonorrhea and chlamydia love the throat. You might not feel a thing, but you can still pass it on. No finish, no problem? Not exactly. It’s about skin, saliva, and contact, not just climax.
2. I have a white tongue after oral sex, do I need to panic?
Breathe. A white tongue could be a dozen things: thrush, syphilis, spicy food aftermath, or just waking up dehydrated. But if it's new, weird, or sticking around longer than a few days, especially with a sore throat or swollen glands, it’s worth testing. Panic? No. Proactive? Always.
3. My sore throat won’t quit. Could it be gonorrhea?
If it’s been more than five days and regular stuff isn’t working (no fever, strep test was negative), then yes, oral gonorrhea is on the table. Most cases fly under the radar because people don’t think to swab the throat. If you gave oral recently, especially unprotected, get checked.
4. Does oral herpes make your breath smell?
It can. Herpes lesions in the mouth or throat can cause bad breath, especially if you’re also dealing with inflammation or open sores. But halitosis is tricky, it can come from tonsil stones, dry mouth, or the garlic fries you had last night. Context is everything.
5. Is thrush an STD or nah?
Not officially. Oral thrush is a yeast thing, candida overgrowth. But it can show up after oral sex, especially if you’ve had antibiotics or a weakened immune system. It’s not about being dirty or infected; sometimes your mouth's just off-balance. Still, recurring thrush can be a red flag worth checking out.
6. What does oral syphilis even look like?
Honestly? It’s sneaky. Primary syphilis in the mouth usually shows up as a small, painless sore, on the tongue, lips, or inner cheek. People mistake it for a canker sore or bite mark and don’t think twice. Then it disappears… and the second stage hits. Don’t ignore a mystery ulcer.
7. Can kissing pass oral STDs?
Some, yes. Herpes is the big one, it spreads easily through kissing, even without visible sores. Syphilis too, if there’s a sore present. Gonorrhea? Possibly, especially in high-prevalence areas or if there’s deep tongue action and shared fluids. Passion is great, just be aware.
8. I got tested, but no one swabbed my throat. Am I good?
Not necessarily. Unless you specifically ask for an oral/throat swab, most clinics only check genitals or blood. That means an oral infection could still be flying under the radar. Next time, tell them you gave oral and want a throat swab. Yes, you have that right.
9. Do I have to tell my partner if it’s just oral chlamydia?
If you tested positive, yes, because they might have it too, and not know. Oral chlamydia can live silently and still spread. Framing it as, “Hey, I found out I had something and I wanted to tell you so you can be safe too” can go a long way. No blame, just care.
10. It feels awkward to test for something that might be nothing. Should I bother?
Listen, awkward is temporary. Regret is worse. If something feels off, or you’re in that spiral of “what if,” just test. You’ll either get peace of mind or a clear plan. That’s power. That’s care. That’s the whole damn point.
Taking the Next Step: Testing That Respects Your Privacy
Maybe you don’t want to go to a clinic. Maybe you live somewhere rural. Maybe the idea of sitting in a waiting room makes your stomach flip. That’s okay, you still have options.
We offer FDA-approved at-home tests for multiple STDs, including those that show up in the mouth. These tests are fast, private, and designed for people exactly like you, people who care, who ask questions, and who want clarity without shame.
Order a Combo STD Test Kit to screen for common oral and genital infections from home.
Whether it’s a white tongue or a lingering doubt, you deserve answers. Don’t sit in worry. Take back control, on your own terms.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
3. Oral thrush – Symptoms & causes | Mayo Clinic
4. Oral thrush – Diagnosis & treatment | Mayo Clinic
5. Symptoms of Candidiasis (including oral thrush) | CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to stop, find, and treat STIs. He combines clinical accuracy with a straightforward, sex-positive attitude and is dedicated to making his work available to more people, both in cities and in rural areas.
Reviewed by: L. Tran, FNP-C | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.







