Can You Trust a Home STD Test?
Quick Answer: A negative STD test doesn't always mean you're in the clear, testing too early, choosing the wrong test, or user error can all lead to false reassurance. If symptoms persist, retesting is often the right move.
This Article Is for You If You’re Still in Pain and Still in the Dark
This guide is for anyone who tested negative but feels far from okay. Maybe your partner didn’t test. Maybe you didn’t have symptoms when you first tested, or maybe they started after the fact. Maybe you feel dismissed or brushed off. Maybe you’re scared to go back. Maybe this is the third time this month you’ve Googled “can you have an STD and still test negative?”
You deserve real answers. The kind that explain what testing really means, how false negatives happen, when to retest, and what else your symptoms could signal. We’ll walk you through the entire maze, from timing mistakes to rare infections to practical next steps.
And we’re not here to shame you. This isn’t about what you “should have done.” It’s about what you can do next, and why your body deserves to be believed.

People are also reading: No Clinic Nearby? Here’s How Rural Americans Are Testing for STDs Anyway
Why a “Negative” Doesn’t Always Mean “Nothing’s There”
First, let's bust the biggest myth: STD tests are not lie detectors. They’re tools. Useful tools, yes, but not flawless ones. Every STD test has a window period, a span of time after exposure where the infection may be present but undetectable. If you test during that window, especially too early, your results may come back negative even if you’re infected.
Here’s another curveball: symptoms often show up before the test can catch the infection. That means your body might already be reacting while the test still gives you the all-clear.
Timing, test type, how you took the sample, and even what infection you might have, these all shape whether your result is accurate or misleading.
According to the CDC's STD screening recommendations, tests vary in sensitivity. That’s especially true for home testing. While many at-home STD tests are highly accurate, some infections like trichomoniasis or herpes can be harder to catch early or with the wrong test method.
“It Burned When I Peed, But My Chlamydia Test Was Negative”
Ty, 27, had symptoms he couldn’t ignore, burning during urination and unusual discharge. He ordered a rapid chlamydia test kit online, followed the instructions carefully, and got a negative result. For a few days, he convinced himself he was fine. But the burning didn’t stop, it got worse. “I thought maybe it was dehydration,” he said. “I just didn’t want it to be something real.”
A week later, still in pain, he went to a walk-in clinic. A urine NAAT test confirmed what the rapid test missed: chlamydia. “The doctor said I probably tested too early,” Ty recalled. “I wish someone had told me that before.”
“Getting that positive result actually gave me relief. At least I knew what was wrong.”
Ty’s story is all too common. Early testing, especially within the first 7–10 days of exposure, can miss infections that haven’t multiplied enough to be detected.
Timing Isn’t Just Technical, It’s Emotional
Let’s get real for a second: most people don’t test because they have perfect timing. They test because they’re scared. Maybe the condom broke. Maybe someone lied. Maybe they woke up with a weird tingle or an unfamiliar smell. The idea of “waiting for the right testing window” feels impossible when your anxiety is through the roof.
But that’s exactly where mistakes happen. And it’s not your fault.
Below is a table to help you understand how window periods differ between STDs, and when to trust your results.
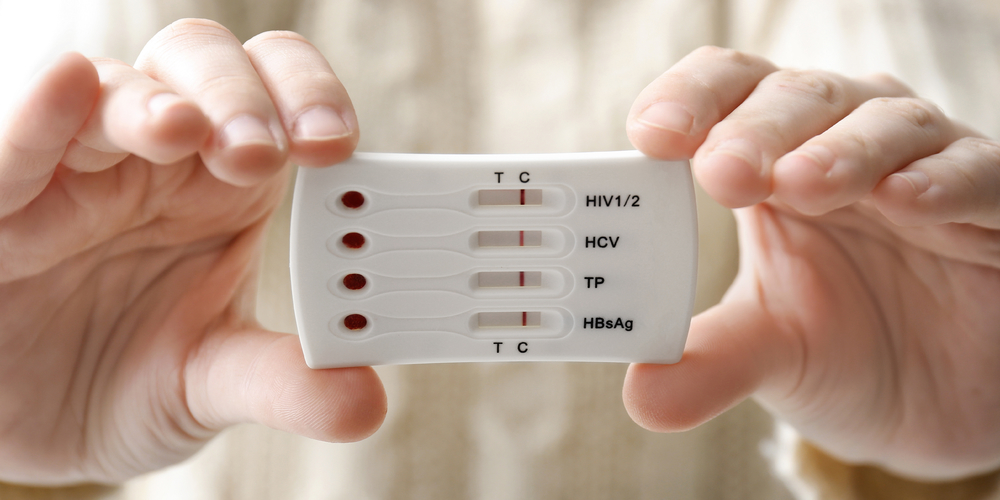
Figure 1. Window periods for common STDs. Testing too early can lead to false negatives, especially for herpes and syphilis.
If you’re still experiencing symptoms after a negative test, especially within 10 days of exposure, retesting isn’t just wise, it’s often necessary.
False Negatives Are Real, and More Common Than You Think
Let's be clear: false negatives are not uncommon. It doesn't mean that your test was broken or that you did something wrong. It means the infection was there, but the test couldn't find it yet. That could happen if:
- You took the test during the window period.
- You took the wrong test for the STD.
- The sample didn't get enough virus or bacteria.
- The infection is in a place that wasn't swabbed, like the throat or rectum.
For instance, a quick test for gonorrhea might show that you have the disease in your urine but not in your throat. If you have an outbreak, a blood test for herpes might come back negative because it takes weeks for antibodies to form. And in some cases, home kits with low sensitivity may not be able to find low viral loads at first.
Tests in the lab aren't always right. A 2020 review by the NIH found that the accuracy of STD tests can change a lot depending on the type of test, the quality of the sample, and the site of the infection. What does it all mean? One negative test doesn't mean you're in the clear, especially if your symptoms are still loud.
Which Tests Are More Likely to Miss an Infection?
Different tests come with different levels of sensitivity. Sensitivity is the test’s ability to correctly identify those with the infection, so low sensitivity = more false negatives.
Here’s a breakdown comparing popular STD test methods:
Figure 2. Sensitivity differences between STD test types. Choosing the right test and testing at the right time dramatically affects your results.
When in doubt, combining test methods (like urine + swab, or antigen + antibody) improves detection rates. This is why combo kits and follow-up testing matter.
“It Took Two Tests to Find the Real Problem”
Sierra, 32, started feeling itchy and sore a few days after a weekend trip with a new partner. She used a mail-in kit that screened for chlamydia, gonorrhea, and HIV, all negative. But something still felt off. “I started doubting myself,” she said. “Like maybe I was just anxious.”
She visited a local clinic 10 days later, and the clinician did a pelvic exam. The swab came back positive for trichomoniasis, a common STD not always included in standard kits. “I felt betrayed by the first test,” Sierra said. “But I also realized it wasn’t about the test being bad. It was about what it didn’t cover.”
“Getting that second test saved me from weeks of symptoms and anxiety.”

People are also reading: Why So Many Women Aren’t Believed About STD Symptoms
When Should You Retest After a Negative Result?
If you tested early and your symptoms are ongoing, the general rule is: wait 10–14 days, then test again. But here’s a more specific breakdown:
- Tested within 7 days of exposure? Retest at 14–21 days
- Symptoms started after your test? Retest immediately and include a broader panel
- Still symptomatic 10+ days post-exposure? Retest with a high-sensitivity test (NAAT or lab)
- Had recent antibiotics? They may suppress detection, retest 3–4 weeks after finishing meds
Use a test that matches your symptoms and exposure route. For example, if you had oral sex but only tested your urine, consider a throat swab. If you’re having discharge but used a fingerstick kit, get a swab instead.
Not sure what to use? Our homepage has discreet combo kits and rapid testing options, including ones that detect infections others miss. Order a combo STD test kit here and get results fast, privately, and confidently.
Peace of Mind Is One Retest Away
Testing isn’t a one-and-done event, it’s a process. It’s okay to get a second test. It’s okay to want answers your body already knows. You’re not being dramatic. You’re paying attention.
Re-testing isn't about paranoia. It’s about power. When you listen to your symptoms and take action, even after a negative result, you’re doing the opposite of ignoring your health. You’re owning it.
When It’s Not an STD, But It Still Hurts
Here’s the hard truth: not every itch, burn, or discharge means an STD. But that doesn’t mean your symptoms aren’t real, or serious. There’s a whole world of conditions that can look, feel, or behave like STDs but aren’t caused by a sexually transmitted infection. Below are some of the most common culprits behind “STD-like” symptoms when your test is negative:
Figure 3. Conditions that mimic STD symptoms. A negative test doesn’t mean you’re imagining things, it may mean the cause isn’t an STD.
Getting tested is always the right move, even if the result points you in another direction. Your symptoms deserve investigation, whether the cause is an infection, inflammation, allergy, or hormone shift.
“They Said It Was Anxiety, But It Was BV”
Jasmine, 23, was told by two different providers that her irritation and odor were “probably from stress.” One even implied she was overreacting. But she couldn’t ignore the persistent symptoms. After another negative STD panel, she took a deep breath and went to a Planned Parenthood clinic where the nurse ran a vaginal swab for bacterial vaginosis. It was positive.
“I felt both furious and relieved. I knew it wasn’t all in my head.”
Medical gaslighting is real, especially for women, queer folks, and people of color. Being told “you’re fine” when your body is screaming “you’re not” is one of the most invalidating things that can happen. If that’s been your experience, we see you. You are not difficult. You are paying attention.
How to Advocate for Yourself in a Medical Setting
If a provider dismisses your symptoms or refuses further testing, you have every right to push back, or switch clinics. Here’s how to reframe the conversation:
- “I understand my test was negative, but my symptoms are still active. Can we explore other causes like BV, UTI, or yeast?”
- “Could this be an infection in a site that wasn’t tested, like my throat or rectum?”
- “I’ve read that some STDs require retesting after the window period. Can I be retested next week?”
- “I’d like to try a more sensitive test like NAAT or expand the panel to include trichomoniasis.”
Want to stay out of the clinic? Many at-home test kits now include broad-spectrum panels and higher-sensitivity options. Order a combo test kit here to retest with better timing and peace of mind. Your body’s truth deserves better than a rushed dismissal.
Should You Pause Sex or Tell a Partner If You Tested Negative?
This is a tricky one. Technically, if your test is negative, there’s “no confirmed infection.” But ethically, if you’re still symptomatic or unsure about your testing window, it’s smart, and respectful, to let partners know you’re figuring things out. You don’t need to sound alarms, but you do need to prioritize safety.
Here’s how you might say it:
“Hey, I got tested after we hooked up and the result was negative, but I’m still having some symptoms and I’m getting retested just in case. Wanted to keep you in the loop in case you want to test, too.”
That’s it. No drama. No accusations. Just care.
And if you’re not sure how to explain the wait for retesting, try this: “Most STD tests need at least 2 weeks after exposure to be fully accurate. I'm just trying to time it right.”
Protecting your partners is part of protecting yourself. And sometimes, that means hitting pause until you know more. Not out of shame, out of strength.

People are also reading: That UTI Might Be Chlamydia, Here’s How to Know for Sure
FAQs
1. I tested negative, but my symptoms are still screaming. What gives?
Honestly? Timing might be the issue. Most STD tests aren’t instant truth machines, they need time after exposure to detect anything. If you tested too soon, especially within the first week, there’s a solid chance it just didn’t pick it up yet. Your body, though? It knows something’s off. Listen to it. Retest if you’re still feeling weird.
2. Could I have an STD that doesn’t show up on the test I used?
Yep. Big time. Not all tests cover everything, and some infections (like trichomoniasis or oral gonorrhea) require specific types of swabs or panels. If you only tested urine but had oral sex? You might have missed something. Same goes for anal exposure. Location matters. Ask for a broader panel, or grab a kit that does more than just the basics.
3. But what if it’s not an STD at all?
That’s also super possible. Burning, itching, discharge, those aren’t STD-exclusive. Yeast infections, BV, UTIs, allergic reactions, hormonal shifts… they can all mimic classic “STD” symptoms. So if you keep testing negative, consider seeing a provider who can swab, culture, or dig deeper. You’re not being paranoid. You’re being thorough.
4. How soon is too soon to test?
If it’s been less than a week since the sketchy hookup or condom fail, you’re probably testing too early. Most STDs need a few days (some even weeks) to build up enough in your system to show up on a test. Wait at least 10–14 days for chlamydia and gonorrhea, longer for herpes and syphilis. Early testing isn’t wrong, it’s just part one.
5. Do antibiotics mess with STD tests?
Short answer: they can. If you took antibiotics recently, whether for a sinus infection or a UTI, they might knock back bacteria enough to skew your test results. Especially with chlamydia or gonorrhea. That doesn’t mean you’re cured, it just means the test might not catch it. Retest 3–4 weeks after finishing meds.
6. Is it awkward to tell someone, “Hey, I tested negative but I’m still retesting”?
It doesn’t have to be. You can keep it chill and factual: “I tested, it came back negative, but I’m still having some symptoms. Just being cautious and getting a follow-up test.” No drama, no blame. You’re being responsible, not rude. And anyone who reacts badly to that? Might not be partner material anyway.
7. Why did my doctor brush me off?
Ugh. Sadly, that happens way too often, especially if you’re young, femme-presenting, queer, or just don’t “look sick.” Some providers assume a negative test means end of story. But you know your body better than anyone. If a provider won’t listen, find one who will. Sexual health clinics and telehealth platforms tend to be way better at this.
8. Can I keep having sex while I wait to retest?
Here’s the thing, if you’re still symptomatic or unsure about timing, it’s smart to hit pause or use extra protection. That’s not fear, it’s respect. For yourself and your partners. And if you do have sex? Let them know you’re still figuring things out. That honesty goes a long way.
9. What’s the most accurate kind of test I can take right now?
Go for a NAAT (nucleic acid amplification test). It’s the gold standard for chlamydia, gonorrhea, and trichomoniasis. If you want fast and discreet, grab a lab-backed combo kit with swab + urine options. The more angles you test from, the fewer surprises later.
10. Do I really need to test again if I already did it once?
If your symptoms are still hanging around or started after the test? 100% yes. Think of the first test as a preview. The follow-up is the full movie. It’s not paranoia, it’s being a damn good detective about your own body.
You Deserve Answers, Not Assumptions
One negative test result doesn’t make your symptoms disappear. And it doesn’t mean you’re making things up. You did the brave, responsible thing by testing, and you’re doing it again by asking, “What now?”
The truth is, testing has limits. But your gut? Your symptoms? Your story? They matter. Whether this is an undetected STD, something else entirely, or a mystery your body is still unraveling, don’t settle for silence.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources. Every external link in this article was checked to ensure it leads to a reputable destination and opens in a new tab, so you can verify claims without losing your place.
Sources
CDC Guidelines: STD Screening Recommendations
NIH Study: Accuracy and Limitations of Rapid STD Testing
Planned Parenthood: STD Basics and Testing Information
Mayo Clinic: STD Testing Overview
VICE Health: “I Tested Negative, But I Still Had an STD”
Reddit Thread: Negative Test, Still Have Symptoms
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who focuses on preventing, diagnosing, and treating STIs. He combines clinical accuracy with a straightforward, sex-positive attitude and is dedicated to making his work available to more people in both cities and rural areas.
Reviewed by: Jenna Marquez, NP | Last medically reviewed: September 2025
This article is for informational purposes and does not replace medical advice.