Sex Toy Cross-Use: What’s Dangerous, What’s Not, and When to Test
Quick Answer: Chlamydia does not go away on its own. Without antibiotics, it can linger silently, spread to others, and lead to serious complications like infertility, pelvic inflammatory disease, and chronic pain.
Why This Article Matters, Especially for Teens and Young Adults
If you’re reading this because you, or someone you care about, is wondering whether chlamydia will just disappear, you're not alone. It’s one of the most Googled questions about STDs. And it’s no surprise: nearly 60% of chlamydia cases occur in people under 25, and many of them never feel a thing.
This article is for those who aren’t sure if they should worry, who feel too scared or ashamed to tell anyone, or who were told by a friend, “It’ll go away on its own.” We’re here to say: your worry is valid. But you also have options. This guide will walk you through what really happens inside the body when chlamydia goes untreated, why symptoms (or lack thereof) don’t tell the full story, and what to do if you’re afraid you might have it.
We’ll also explore how at-home tests can offer discreet, fast answers, without needing to explain yourself to a doctor or parent. Because knowing what’s happening in your body shouldn’t come with shame.

People are also reading: Why Chlamydia Is Often Missed in Young Women
Why Chlamydia Doesn’t “Just Go Away”
There’s a dangerous myth that chlamydia is a “mild” infection that clears on its own. This belief usually stems from two things: lack of symptoms and misinformation on social media. But chlamydia is a bacterial infection, meaning it requires antibiotics to be eliminated. Unlike viruses, bacteria don’t “burn out” in the body the same way. Left alone, they dig in deeper.
Studies have shown that untreated chlamydia can persist for months, sometimes years. One study from the Journal of Infectious Diseases found that the infection was still detectable a year later in over 50% of untreated participants. Another CDC report confirms: without treatment, chlamydia doesn’t just linger, it climbs. For people with a uterus, it can move into the upper reproductive tract, causing pelvic inflammatory disease (PID).
And here's the trap: because symptoms might fade or never appear, many teens assume the infection is gone. In reality, the damage is still happening, just silently.
The Silent Damage of Untreated Chlamydia
Elena, 19, didn’t realize anything was wrong until she started having sharp cramps during sex. She’d had an odd discharge earlier that year, but it went away on its own. No pain, no fever, so she forgot about it. It wasn’t until a nurse practitioner brought up the possibility of pelvic inflammatory disease that she even connected the dots. A chlamydia test came back positive. By then, she’d already developed scarring in her fallopian tubes.
“I thought it was just a yeast infection or something. If I’d known it could affect fertility, I wouldn’t have waited.”
Here’s what can happen when chlamydia goes untreated, especially in teens and young adults:
Figure 1. Overview of the most common and serious complications of untreated chlamydia.
“But I Don’t Have Any Symptoms…”
This is the number one reason people, especially teens, skip testing. But here’s the reality: up to 70% of women and 50% of men with chlamydia have zero symptoms. That means you can have it, transmit it, and suffer long-term damage… all without a single obvious sign.
When symptoms do occur, they’re often mistaken for something else, like a UTI, yeast infection, or irritation from sex. And because chlamydia can affect the throat, rectum, and eyes (not just genitals), many cases go misdiagnosed entirely.
Some subtle signs of chlamydia include:
Figure 2. Common signs of chlamydia and how they’re often confused with less serious issues.
Can Your Body Clear Chlamydia Without Antibiotics?
This is one of the most dangerous myths still circulating on Reddit, TikTok, and even in some sex-ed classrooms: that your immune system will eventually “fight off” chlamydia without help. The idea sounds hopeful, but it’s not grounded in current science. While a small number of cases might resolve spontaneously, most don’t. And the longer the bacteria stay, the more likely they are to cause irreversible damage.
A study in Sexually Transmitted Diseases journal tracked untreated chlamydia infections over time. Researchers found that while a few immune systems could suppress the infection temporarily, none reliably eliminated it without antibiotics. Worse, those “quiet” periods gave people false reassurance, leading to higher rates of transmission to others.
Let’s be clear: the only medically verified cure for chlamydia is antibiotic treatment, typically azithromycin or doxycycline. There is no natural remedy, herbal cleanse, or immune hack that can eliminate it completely. Without proper meds, it simply hides, and spreads.
The Risk of Believing the Myth
Jordan, 18, had heard that some people’s bodies “naturally clear” chlamydia. He tested positive after a hookup, but he hated the idea of telling his mom or going to the doctor. So he ignored it. Two months later, he ended up in urgent care with intense testicular pain. The diagnosis: epididymitis, a complication of untreated chlamydia that can lead to infertility.
“If I’d just taken the pills when I had the chance, I could’ve avoided all of this.”
This belief, that chlamydia will fade like a cold, can lead to:
- Delays in testing: People skip or postpone getting checked, thinking they’re safe.
- Partner transmission: If you don't treat an infection, it can spread to other people without them knowing, making things worse.
- Health problems that last a long time: The longer chlamydia stays in the body, the more tissue it can hurt.
- False negatives: If you test too early during incubation, you might miss the infection, which could spread more if you don't do a follow-up test.
This is why all reliable medical sources, from the CDC to the NHS, stress the need for immediate treatment, even if symptoms have gone away or never appeared in the first place.
How Testing Works (And Why Timing Matters)
Testing for chlamydia is simpler than you think. You don’t need a pelvic exam or blood draw. Most tests use either a urine sample or a swab (vaginal, rectal, or throat, depending on exposure). The gold standard is a NAAT test, short for nucleic acid amplification test, which detects even tiny amounts of chlamydia DNA.
This is the same method that at-home kits use now. When you order a kit from a trusted source like STD Test Kits, you'll get clear instructions, a sample container, and an envelope that doesn't show what you're sending back. You get results quickly, and no one else can see them.
But here’s the catch: testing too soon can lead to false reassurance. Chlamydia has an incubation period, the time between exposure and when the infection becomes detectable. This is different from symptoms, which might never appear.
Figure 3. Chlamydia detection timeline to help readers plan testing and retesting with confidence.
“I Tested Negative… So Why Do I Still Feel Off?”
This happens more often than you think. A negative result doesn’t always mean you're in the clear, especially if you tested early. The incubation period can cause false negatives, and test accuracy also depends on proper sample collection. If you peed too soon, didn’t swab deeply enough, or used the wrong site (vaginal vs throat vs rectal), results may miss the mark.
One reader, Leila, 16, tested negative on day six after a hookup. She still felt off, minor cramps, some discharge, but told herself she was overthinking it. At her friend’s urging, she retested two weeks later. This time, the chlamydia test was clearly positive.
This is why experts often recommend retesting at least two weeks after exposure, especially if you tested early or still have symptoms. You can order a discreet chlamydia test kit here, no clinic visit required.

People are also reading: How Super Gonorrhoea Spreads (Even If You Use Protection)
What Treatment Actually Looks Like (Spoiler: It’s Simple)
If you’re scared of what treatment might involve, don’t be. Unlike some infections that require injections or complicated regimens, chlamydia is usually cleared with a short round of antibiotics. The most common options are:
- Doxycycline: 100mg twice daily for 7 days
- Azithromycin: A single 1g dose (less common now due to resistance)
There’s no hospital stay, no IV, and no surgery. If you test positive through an at-home kit or clinic, a provider will either prescribe medication remotely (via telehealth) or give you a pharmacy pickup script. Some clinics even offer expedited partner therapy (EPT), where your partner gets treated without needing their own visit first.
Treatment is most effective when started promptly. After antibiotics, symptoms (if present) usually clear within a week, but the infection itself can take a bit longer to fully resolve. That’s why guidelines recommend abstaining from sex for 7 days after finishing meds, to prevent reinfection or passing it to others mid-treatment.
Do You Need to Retest After Treatment?
It depends. If you’ve completed treatment, felt better, and didn’t resume sex with a partner who might still be infected, you may not need to retest. But there are exceptions, and a lot of people fall into them.
According to the CDC treatment guidelines, teens and young adults under 25 are advised to retest 3 months after treatment, regardless of whether symptoms returned. Why? Because reinfection is common, especially if partners weren’t treated or if new exposures occur. You might feel fine, but the bacteria could be back.
Other scenarios where retesting makes sense:
- You’re still having symptoms 3 weeks post-treatment
- You started a new relationship after getting treated
- You didn’t finish your antibiotics correctly
- Your partner didn’t (or wouldn’t) get treated
In these cases, using an at-home Combo STD Test Kit can offer peace of mind and privacy, especially if going back to the clinic feels overwhelming or awkward.
Partner Treatment: Why It’s Non-Negotiable
Kai, 17, got treated for chlamydia right after a hookup went wrong. But he didn’t tell his girlfriend because “she didn’t have any symptoms.” Three weeks later, she had severe pelvic pain and landed in the ER. Not only had he unintentionally reinfected himself during sex post-treatment, he’d also passed it to her, worsening the consequences.
“I didn’t realize how bad it could get just because I was scared to talk about it.”
Here’s the truth: chlamydia is highly contagious even when asymptomatic. Treating only one partner is like cleaning half a wound. Reinfection rates are highest among teens and young adults not because antibiotics fail, but because only one person gets treated.
If your partner refuses testing or won’t seek care, you still have options. Many telehealth services offer partner prescriptions, and some health departments provide anonymous notification tools like TellYourPartner.org. You don’t have to do it alone, or awkwardly.
At-Home STD Testing: Why It’s a Game-Changer for Teens
For many teens and young adults, walking into a clinic feels like walking into judgment. You don’t want questions, paperwork, or raised eyebrows. You just want to know what’s happening in your body, and what to do next.
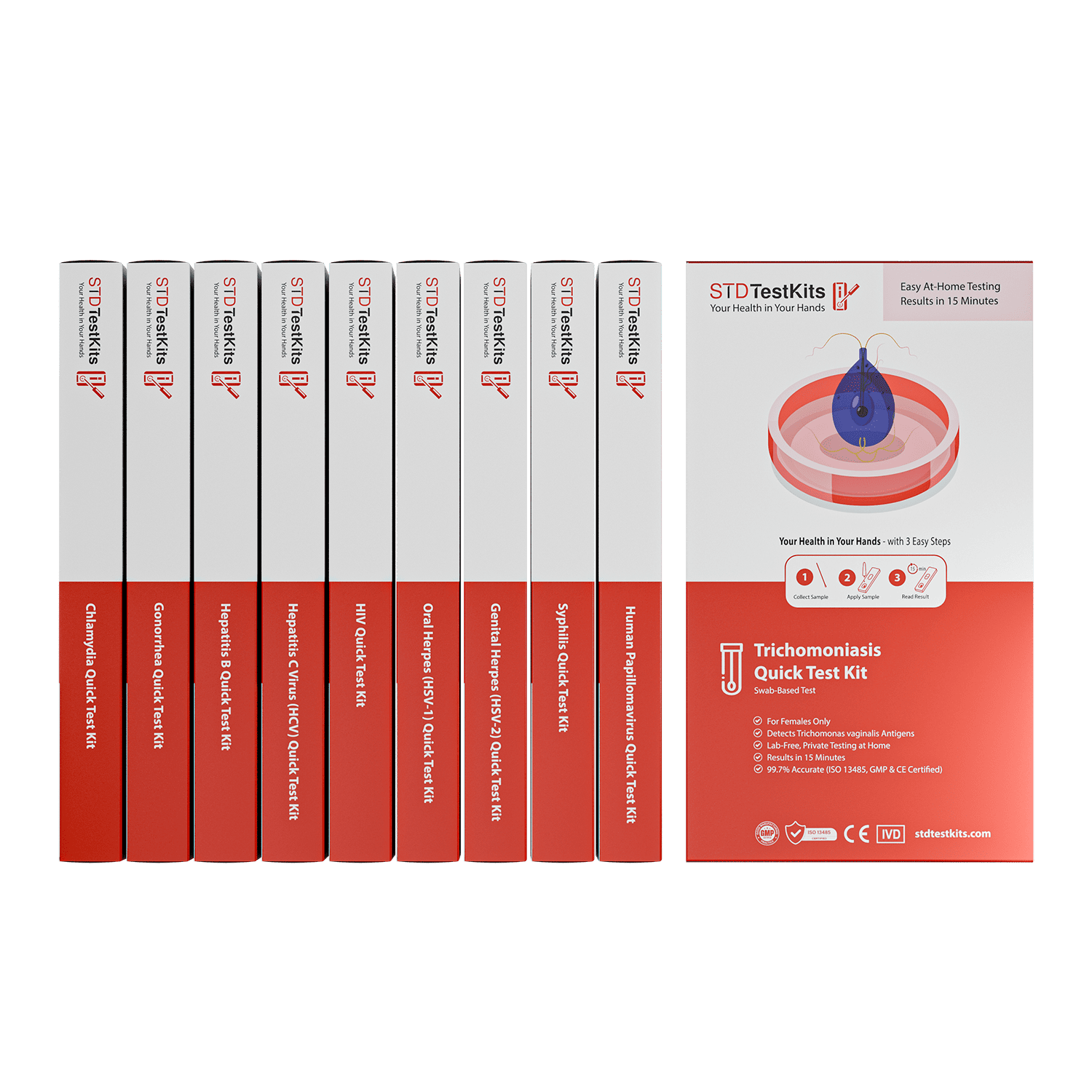
That’s why at-home testing is so powerful. With STD Test Kits, you can:
- Order discreetly online (no need to ask a parent)
- Test in the privacy of your home, on your schedule
- Get results fast, often within minutes (for rapid kits) or a few days (for lab mail-ins)
- Choose single STD kits or Combo Kits that check for multiple infections at once
Whether you’re dealing with a possible exposure, retesting post-treatment, or just want peace of mind, you can order your chlamydia rapid test kit here. No insurance required. No awkward waiting room. Just answers.
Why Chlamydia Needs Real Treatment
Chlamydia isn’t the kind of infection you can “wait out.” Even if it seems mild, or invisible, it’s often doing quiet harm beneath the surface. Without antibiotics, it can affect your fertility, your relationships, and your long-term health. That’s not a scare tactic. That’s what the science shows.
And you don’t need a parent, a partner, or a doctor’s permission to take action. With affordable, private testing options and simple treatments available, you can handle this. You can stop the cycle. You can heal without shame.
FAQs
1. Can chlamydia really go away on its own?
Nope. That’s one of the riskiest myths out there. Chlamydia is a bacterial infection, it doesn’t just “poof” and vanish. Even if your symptoms fade (or never show up), the bacteria can still be active inside your body, quietly messing with your reproductive system.
2. I feel fine. Should I still get tested?
Yes. Please. Chlamydia is sneaky, around 70% of people with vaginas and 50% with penises don’t get symptoms. Feeling fine doesn’t mean you're in the clear. Think of it like a slow leak in your tire: just because the car’s still rolling doesn’t mean you’re safe to drive cross-country.
3. What happens if you ignore it?
It keeps going. It spreads to your partners. And over time, it can scar your fallopian tubes or testicles, mess with fertility, and trigger painful conditions like PID or epididymitis. We've seen 17-year-olds with pelvic pain so bad they thought it was appendicitis. Spoiler: it was chlamydia, untreated for months.
4. How soon can I test after hooking up?
The sweet spot is around 14 days post-exposure. You *can* test earlier (especially if symptoms hit), but it might be too soon for an accurate result. If you test at day 5 or 7 and it’s negative, plan to retest later to be sure.
5. Can I get chlamydia more than once?
Absolutely, and it’s way more common than people think. Getting treated once doesn’t mean you’re immune. If your partner wasn’t treated too, or if you have unprotected sex with someone new, it can come right back around.
6. Can I give it to someone even if I have no symptoms?
Yep. This is the silent part that makes it so frustrating. You can feel 100% fine and still pass chlamydia during oral, vaginal, or anal sex. That’s why testing is about protection, not punishment.
7. Do I really have to tell my partner?
It’s awkward, we know. But yes, you should. The longer they go untreated, the more damage chlamydia can do. If the conversation feels impossible, try anonymous tools like TellYourPartner.org or talk to a provider about EPT (expedited partner therapy), where they can get meds without a visit.
8. How does treatment work? Is it intense?
Honestly, it’s chill. Most people take a week of antibiotics, doxycycline is the go-to these days. No needles, no hospital, no judgment. Just take your meds, avoid sex for 7 days, and you’re good.
9. I tested negative. Could it still be chlamydia?
It’s possible, especially if you tested too soon or didn’t swab the right area (yes, throat and rectal chlamydia exist). If you’re still feeling off, trust your gut. Retest at the two-week mark or grab a combo kit to check for other STDs too.
10. Are there any natural cures that actually work?
As much as we love herbal tea and wellness TikTok, no. There’s no evidence that garlic, apple cider vinegar, or oregano oil can cure chlamydia. Save your time (and your plumbing). Stick with antibiotics, they’re boring, but they work.
You Deserve Answers, Not Assumptions
Thinking “it’ll just go away” is a gamble you shouldn’t have to take with your body. Whether you’re dealing with symptoms, worried about a recent hookup, or just want peace of mind, there’s one truth we’ll never stop repeating: testing is care, not a confession.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. NHS – Chlamydia Information
2. Planned Parenthood – Chlamydia Overview
4. Chlamydial Infections – STI Treatment Guidelines (CDC)
5. Spontaneous Resolution of Genital Chlamydia trachomatis Infection – PMC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Dr. M. Kwan, MPH | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.