HIV From Oral Sex: Is Giving or Receiving Riskier?
Quick Answer: Sex toy cross-use can carry STD risk when fresh bodily fluids or direct skin contact are involved and the toy wasn’t cleaned or covered. Many infections don’t survive long on surfaces, but testing is recommended based on timing, type of contact, and symptoms.
Why Sex Toy Cross-Use Feels So Confusing
Most people were never taught how to think about sex toys in terms of infection risk. Sex education focuses on bodies touching bodies, not objects moving between them. So when a toy enters the picture, especially across partners, there’s no clear mental rulebook.
The confusion often comes from mixing emotional shock with medical uncertainty. A sense of betrayal can make every possibility feel more dangerous than it actually is. At the same time, minimizing the risk entirely can leave real infections undetected.
The truth lives in the middle. Some risks are real. Many fears are exaggerated. And both deserve to be addressed without shame.
STDs don’t spread because an object was “shared” in a general sense. They spread through very specific pathways: fresh bodily fluids, skin-to-skin contact, and exposure of mucous membranes like the vagina, anus, or urethra.
A sex toy can become a transmission bridge only if it carries those elements from one body to another in a short window of time. That’s why timing, cleaning, and type of use matter more than the fact that the toy exists at all.
If a toy was used externally, cleaned thoroughly, or reused days later, the medical risk is often far lower than people assume.

People are also reading: India’s Game-Changer: What a New HIV Prevention Shot Means for At-Home Testing
When Sex Toys Can Increase STD Risk
Sex toys don’t automatically increase STD risk just because they exist. The risk comes from a specific chain of events: internal use, exposure to fresh bodily fluids or skin, and then reuse before those materials are removed or rendered inactive. When those conditions line up, a toy can function less like an object and more like a temporary extension of the body.
The highest-risk situations almost always involve toys that were used vaginally or anally and then reused immediately on another person without cleaning or a barrier. Timing matters. Minutes matter. In those narrow windows, infections that live in fluids or on skin still have an opportunity to transfer.
Most STD anxiety around sex toys comes from imagining pathogens lingering indefinitely on surfaces. That’s not how most infections behave. What changes the equation is immediate reuse, before fluids dry, before soap disrupts organisms, and before air exposure reduces viability.
In these moments, toys can carry microscopic amounts of vaginal or rectal fluid directly from one mucous membrane to another. That’s the same pathway many STDs already use during sexthe toy simply acts as the intermediary.
This is why context matters more than labels like “shared” or “used.” A toy used days ago, cleaned, and stored is a fundamentally different exposure than a toy passed hand-to-hand mid-encounter.
Only certain STDs realistically match the conditions created by sex toy cross-use. These are primarily infections that spread through genital fluids or close mucosal contact.
Table. STDs most relevant to sex toy cross-use and the conditions that increase risk.
Why Herpes Is Different (and Often Overestimated)
Herpes doesn’t behave like bacterial STDs. It doesn’t need fluids to spread, and it doesn’t survive well on inanimate surfaces. What it does need is skin-to-skin contact with an area that’s actively shedding viruswith or without visible sores.
This means toy-based transmission is possible but uncommon. The higher-risk scenario would involve a toy making direct contact with an active lesion or shedding skin and then being reused immediately on another person’s mucous membranes.
If time passed, if the toy was cleaned, or if no active outbreak was present, the likelihood drops sharply. Herpes anxiety often lingers long after the biological risk window has closed.
Material Matters More Than People Expect
Not all sex toys behave the same way. Non-porous materials like medical-grade silicone, stainless steel, and glass are far easier to clean and do not trap fluids internally.
Porous materials can retain microscopic amounts of fluid, which slightly increases risk when combined with immediate reuse. That doesn’t mean infection is likelyit means cleaning and barriers matter more.
This is why condoms on toys, especially during partner changes, are a practical risk-reduction tool rather than an overreaction.
Sex toy–related STD risk is not about moral judgment, ownership, or whether something “counts as cheating.” It’s about exposure mechanics. When internal use, fresh fluids, and rapid reuse intersect, testing becomes a reasonable next step.
When those elements aren’t present, fear often outweighs biology.
The goal isn’t to eliminate every theoretical risk. It’s to understand which situations actually deserve your attentionand which ones don’t.
What Usually Does NOT Pose a Serious Risk
Many people assume that any prior use of a toy automatically equals infection risk. That’s not how most STDs behave outside the body.
HIV, for example, is extremely fragile once exposed to air. It does not survive well on surfaces and is not efficiently transmitted via objects. Syphilis also does not live long outside the body and is very unlikely to spread through a toy.
If the toy was washed with soap and water, allowed to dry fully, or used long after the other encounter, the likelihood of transmission drops sharply.
STD risk from sex toys is less about who used them and more about when. Fresh fluids create potential risk. Dried surfaces almost never do.
This is why someone can feel intense anxiety days later even though the biological window for transmission has long passed. Fear doesn’t follow the same rules as pathogens.
Understanding timing helps you decide whether testing is necessary or whether reassurance is medically justified.
When Testing Makes Sense
If there is sharing of the toy without cleaning and protection, especially if there is penetration and the act is repeated soon, testing is advised. Even if there are no symptoms such as an odd-smelling discharge, pelvis tenderness, burning during urination, sores, and bleeding.
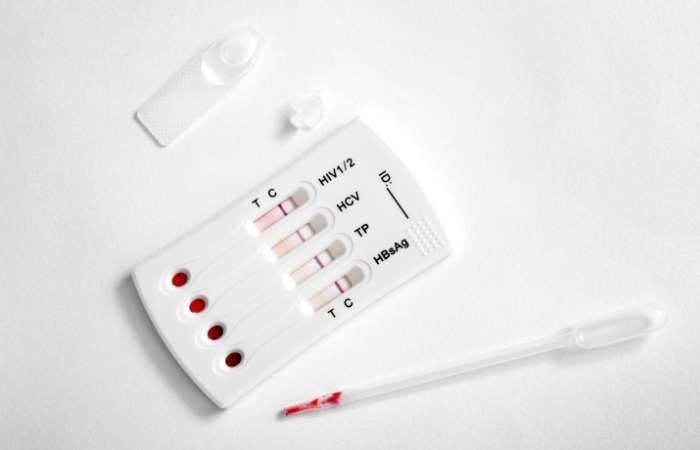
Even if one does not have symptoms, testing can bring about relief. This is the case since many STDs are often without symptoms. One cannot just wait for the signs to manifest. There are discreet ways of carrying out testing, one of which is STD Test Kits.
What might happen when you take the test during the window period is that you could be misled by the results. “No infection” is what you might feel when you get a negative test result when you first take it. “Not detectable yet” could be the accurate interpretation when you first take the test.
A combo STD home test kit is often the most efficient option in these situations because it screens for multiple infections at once.
Going forward, it’s reasonable to set clear boundaries around toy use. Using condoms on toys, cleaning them thoroughly, and allowing full drying time dramatically reduces risk. These practices aren’t about punishment or mistrust. They’re about basic sexual health, just like using protection or getting tested between partners. You’re allowed to care about your body without justifying it to anyone.
What to Test For After Sex Toy Cross-Use
Once the initial panic fades a little, most people land on the same grounded question: what do I actually need to test for? The answer isn’t “everything,” and it isn’t “nothing.” It depends on exposure mechanicswhat kind of contact happened, how soon the toy was reused, and whether barriers or cleaning were involved.
Strategic testing matters here. Over-testing can amplify anxiety without adding clarity, while under-testing can leave infections quietly untreated. The goal is to match the test panel to the biology of the exposure.
Not all STDs behave the same way outside the body, and not all of them align with toy-based transmission. Some infections require direct skin-to-skin contact. Others need blood-to-blood exposure. Others still don’t survive long once fluids dry.
Sex toy cross-use primarily raises concern for infections that live in genital fluids and can transfer quickly between mucous membranes. That’s the filter that should guide testing decisions.
Bacterial STDs that live in vaginal or rectal fluids are the most relevant when toys are shared without cleaning or condoms. These infections don’t need dramatic symptoms to spreadthey just need a brief opportunity.
Chlamydia and Gonorrhea are the most commonly implicated. Both are frequently asymptomatic, especially early on, which is why testing is recommended even if your body feels completely normal.
Trichomoniasis is less talked about but still relevant, particularly when vaginal contact or porous toys are involved. It often flies under the radar unless it’s specifically tested for.
Table. Core STDs to prioritize after sex toy cross-use.
Certain diseases cause considerable fear but don’t easily fit into toy-based modes of transmission. The tests for such diseases are largely based on other factors of exposure.
HIV is not viable outside the body, and it is inefficient when transmitted via objects. Syphilis can be transmitted only by contact with an open sore and is not viable for long on surfaces.
It doesn’t mean they are impossible SIEIT means they are not of major concern in most cross-use scenarios involving sex toys.
Table. STDs that are typically lower priority after toy exposure.
Where Herpes Fits In
Herpes sits in a gray zone. It doesn’t spread through fluids the way bacterial STDs do, and it doesn’t persist on surfaces. But it can spread through direct contact with shedding skin.
Testing for herpes after toy cross-use is usually symptom-driven. If sores, tingling, or new irritation appear, testing makes sense. Without symptoms, routine screening often creates more confusion than clarity.
This is one of the few areas where waiting to see how your body responds is often more useful than immediate testing.
For most sex toy cross-use scenarios involving internal contact and unclear cleaning, a focused panel that includes chlamydia, gonorrhea, and trichomoniasis provides the highest yield.
This approach balances medical accuracy with emotional sanity. It addresses the infections that realistically match the exposure without turning a moment of uncertainty into a months-long testing spiral.
Testing is not about proving something went wrong. It’s about giving your nervous system an answer it can trust.
Why Symptoms Aren’t a Reliable Guide
One of the most frustrating realities of STDs is that the absence of symptoms doesn’t equal the absence of infection. Many people wait for their body to “signal” danger, but that signal often never comes.
Chlamydia and gonorrhea frequently stay silent, especially in people with vaginas. When symptoms do appear, they can be subtle and easy to dismiss as irritation, stress, or hormonal changes.
Testing is not an admission of risk, it’s a way to replace guessing with certainty.
Every STD has a window period, the time between exposure and when a test can reliably detect infection. Testing too early can lead to false negatives, which is why timing matters as much as the test itself.
For most bacterial infections linked to toy cross-use, accuracy improves significantly around 10 to 14 days after exposure. Earlier testing can still be useful, but follow-up may be needed.
Understanding window periods helps you decide whether to test now, later, or both.
People are also reading: Why Do Some People Never Show STD Symptoms?
A Practical Testing Timeline
Testing can give you a baseline if you are within the first week after exposure, but it should not be seen as the final answer. At this point, a negative result could just mean that the infection hasn't reached levels that can be seen yet.
Most standard tests for chlamydia, gonorrhea, and trichomoniasis are accurate between days 10 and 14. Most doctors recommend this window.
Testing should happen right away if any symptoms show up, no matter when they do.
One option is to get tested at a clinic, but a lot of people put off getting care because they don't have time, are worried about privacy, or are too emotional. That delay can make anxiety last longer than it needs to.
Using STD Test Kits to test at home lets you do it on your own time and in private, which is great when you're still talking about your relationship. After using toys with someone else, a combo STD home test kit is often the best option because it checks for more than one infection at a time.
If your first test comes back negative
A negative result is good news, but the situation is important. If the test was done early in the window period, a second test may still be needed to make sure the first one was correct.
This doesn't mean that the test didn't work or that something went wrong. It just shows how infections spread and how tests work.
Retesting is a plan, not something you do in a hurry.
If your first test comes back positive
When you see a positive result, it can feel like the floor is falling out from under you. Even if you knew it was possible, the confirmation can make you feel scared, angry, and full of questions all at once.
Take a deep breath. Most STDs that could be passed on by using sex toys with someone else are either treatable, manageable, or both. A positive result doesn't mean you're guilty; it just gives you information so you can act.
If the result causes betrayal trauma
For a lot of people, the medical problem is only half of the problem. Finding out that someone used your toys without your permission or knowledge can trigger betrayal trauma, especially if it goes against what you agreed to.
Even after the test is over, your nervous system may still be on high alert. That doesn't mean you're crazy or overdramatic. It means that something about your safety or trust was broken.
One step is medical clarity. It often takes longer to get emotional clarity.
Treatment Is Often Simple
A short course of medicine is usually all that is needed to treat bacterial infections like Chlamydia, Gonorrhea, and Trichomoniasis. Treatment works, is common, and is easy to get.
When it comes to viral infections like herpes, management is all about controlling symptoms and lowering the risk of spreading the virus. A lot of people live normal, healthy lives without any ongoing symptoms.
A positive test doesn't mean your health will always be bad. You caught it early enough to do something about it.
Rebuilding Trust With Yourself First
After situations like this, people often doubt their own judgment more than they doubt their partner. They replay what they “should have noticed” or told themselves they were imagining. Testing, setting boundaries, and seeking information are acts of self-trust. They’re ways of saying: my body matters, and I will respond when something feels off.
You don’t need to rush into decisions about the relationship while your nervous system is still processing.
There is no medically correct relationship outcome after sex toy cross-use. Some people repair trust with clearer agreements and safer practices. Others decide the rupture is too deep. Pausing to gather information, medical and emotional, is not avoidance. It’s assessment.
Your timeline doesn’t need to match anyone else’s expectations.
After treatment for bacterial STDs, retesting may be advised to ensure clearance, especially if symptoms persist or reinfection is possible.
If your first test was early in the window period, follow-up testing helps lock in accuracy and peace of mind.
Retesting isn’t about mistrust. It’s about closing the loop.
If sex toys remain part of your life, alone or with partners, risk reduction strategies matter. Using condoms on toys, cleaning thoroughly between uses, and having explicit agreements around sharing are effective and reasonable.
These practices don’t require moral framing. They’re simply health habits, like handwashing or testing between partners.
Safety and pleasure are not opposites.
FAQs
1. Can you actually get an STD from a sex toy someone else used?
Yes, but that’s not an automatic process and that’s not magic. Its transmission will need new bodily fluids and direct skin contact, and that is contingent upon the toy being reused right away with actual skin contact and/or new bodily fluids, which means if time passed by or the toy is washed and dried, the chances go down quickly.
2. If the toy was cleaned, am I in the clear?
Often, yes. Soap and water do a lot of heavy lifting here. That said, if you’re not sure how well it was cleaned, when it was reused, or whether penetration was involved, testing is still a reasonable move, not because you’re doomed, but because uncertainty is exhausting.
3. How soon after sex toy cross-use should I test?
Most bacterial infections like chlamydia and gonorrhea are best detected around 10 to 14 days after exposure. Testing earlier can still be useful, especially if anxiety is high, but a follow-up test may be needed to lock in accuracy.
4. What if I feel totally fine no symptoms at all?
That’s common. Annoyingly common. Many STDs don’t announce themselves with fireworks. No pain doesn’t mean no infection, especially early on. Testing isn’t about reacting to symptoms; it’s about getting ahead of what might be quiet.
5. Can herpes really spread through a sex toy?
It’s possible, but not common. Herpes spreads through skin-to-skin contact, not surfaces. The higher-risk scenario would be immediate reuse during active sores or viral shedding. If time passed or the toy was cleaned, the risk is much lower than people fear.
6. Should I be worried about HIV from a shared toy?
This one causes a lot of panic, so let’s be clear: HIV does not survive well outside the body. Transmission through sex toys is considered extremely unlikely. If this is your main fear, that’s understandable but medically, it’s not a common concern here.
7. Do I need to confront my partner before getting tested?
Nope. Testing is a medical decision, not a relationship referendum. You’re allowed to get information quietly, privately, and on your own timelineespecially if emotions are still raw.
8. What test makes the most sense after toy cross-use?
In most cases, a multi-STD test is the most efficient option. It screens for the infections that actually align with this kind of exposure, without turning your life into a series of appointments.
9. Am I overreacting by testing over “just a toy”?
No. You’re responding to unclear exposure with clarity. That’s not overreacting, that’s self-respect. Your body doesn’t need to earn care by meeting some imaginary threshold of risk.
10. What if testing brings up more emotional stuff than medical stuff?
That’s normal. Sometimes the test is easy and the feelings aren’t. Getting answers can help separate what’s happening in your body from what’s happening in your relationship and that separation alone can be grounding.
Before You Decide Anything Else, Take Care of Your Health
Sex toy cross-use can blur lines between medical risk and emotional hurt. It’s normal if your thoughts feel tangled right now. What matters is that you don’t ignore your body while trying to make sense of everything else.
Testing doesn’t force a relationship decision. It simply gives you information, quietly, privately, and on your terms.
If you want discreet clarity, this at-home combo STD test kit screens for the most common infections without clinic visits or uncomfortable conversations.
How We Sourced This: We built this guide using current public health guidance, peer-reviewed research on STD transmission and surface survival, and real-world sexual health education. Around fifteen reputable sources informed this article; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Planned Parenthood – STD Basics
2. NHS – Sexually Transmitted Infections
3. About Sexually Transmitted Infections (STIs) | CDC
4. Sex Activities and Risk Including Shared Sex Toys | NHS
5. Preventing HIV with Condoms (Including with Sex Toys) | CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist with a focus on STI prevention, testing accuracy, and patient-centered sexual health education.
Reviewed by: J. Alvarez, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.







