Can Chlamydia or Gonorrhea Infect Your Eye? What to Watch For
Quick Answer: STD symptoms after a negative test may mean the test was taken too early, the wrong type of test was used, a different condition is causing symptoms, or you’ve been reinfected. Retesting is often the best next step.
Why This Happens More Than You Think
“I tested negative, but it still burns when I pee.” That phrase shows up in search bars and group chats every day. For many people, especially those testing shortly after exposure, a negative result doesn't always mean you're clear. Here's why.
Every STD test has a window period, the time between infection and when the test can reliably detect it. If you test during this window, your body might not have produced enough markers (like antibodies or DNA fragments) for the test to pick up. That means your test might say “negative” while your body is already working overtime to fight something off.
In a 2023 CDC report, false negatives for chlamydia and gonorrhea were most likely to occur when people tested within five days of exposure, before the infection had time to multiply to detectable levels. And with herpes, many antibody tests can miss infections if taken within the first 6–12 weeks.
People are also reading: Think Pulling Out Is Safe? Not for Herpes, HPV, or Chlamydia
Window Periods: How Early Is Too Early?
If your symptoms started a few days after a risky encounter and you tested within a week, there’s a real chance the test was premature. Here’s how long you should generally wait to get the most accurate results.
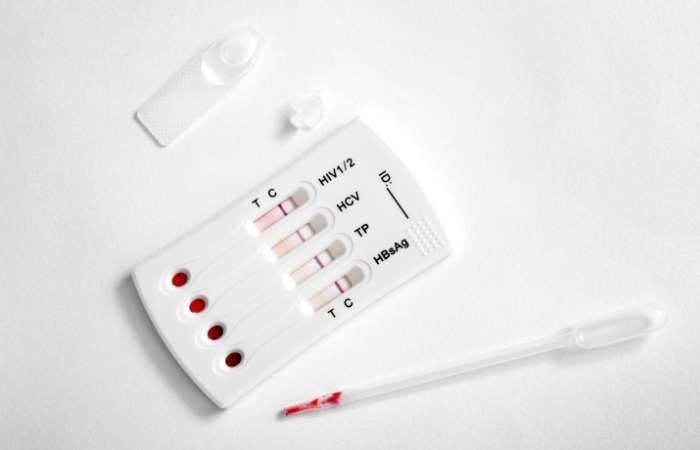
Figure 1. Window periods show when each STD becomes reliably detectable. Testing too soon increases the chance of a false negative.
“I Tested Negative, Then Everything Got Worse”
Niko, 27, had unprotected sex with a new partner while traveling. They felt fine for a few days, then developed a mild burn when peeing and some redness. A rapid test taken on day five was negative. They moved on. Two weeks later, the symptoms were worse, and new bumps appeared. This time, the lab test came back positive for herpes.
“It was a gut punch. I thought I was being responsible by testing early. No one told me I could get a false negative.”
What happened to Niko isn’t rare. Testing early can offer peace of mind, but only if you understand the limits. A negative result doesn’t always mean you're in the clear. It could just mean the test couldn’t detect the infection yet.
Next, we’ll break down whether your symptoms could be tied to a new infection, or if it’s something your first test just missed.
Missed Something the First Time? It Happens
If you tested during the early stages of infection, or used a lower-sensitivity rapid test, there’s a real possibility the test simply missed it. This isn’t always user error. Even high-quality tests have limits, especially when symptoms are new, faint, or unusual. Rapid tests, for instance, often rely on markers that haven’t appeared yet in early-stage infections.
A 2021 NIH study found that antibody tests often missed early herpes infections, especially primary HSV-1 genital outbreaks, in the first month. Trichomoniasis, particularly in males, may evade detection in both rapid and laboratory tests due to the intermittent shedding of the parasite.
If you're still having symptoms days or weeks after a negative test, and especially if those symptoms are worsening, the issue may never have been fully caught. Retesting with a more sensitive method (like a NAAT or PCR test) is often the next best move.
Or…Could It Be Reinfection?
Let’s say you tested negative at the right time, your symptoms went away, and you even got treatment, or your test was negative but reliable. Now your symptoms are back. It’s easy to think the first test must have been wrong. But it’s just as likely that you’ve been reinfected.
Reinfection doesn’t mean the test failed, it means exposure happened again. This could be through a new partner, or even the same partner who hasn’t been treated. Chlamydia and gonorrhea reinfections are particularly common; a 2020 CDC review found that up to 20% of people treated for chlamydia tested positive again within six months, usually due to untreated partners or condomless sex with new partners.
Don’t beat yourself up. This is about biology, not morality. You can catch the same STD again, even shortly after clearing it. That’s why retesting after treatment is part of CDC guidelines for certain infections.
Post-Treatment Symptoms: Not Always a New Infection
Here’s another scenario: You were treated, say, a round of antibiotics for chlamydia, and you're still having symptoms days or weeks later. Your mind jumps to a new infection or treatment failure, but sometimes your body just needs time.
Antibiotics don’t always bring instant relief. Some people experience post-infectious inflammation, which can feel identical to the original infection. For example, urethral tissues may remain irritated for days after bacteria are cleared. Similarly, women may still have spotting, discharge, or pelvic pain due to cervical inflammation or bacterial imbalance post-treatment.
And if you took medication but had sexual contact too soon, before the full treatment window cleared the infection, there’s a risk you transmitted or re-acquired the infection without realizing it. The CDC recommends abstaining from sex for seven days after completing chlamydia or gonorrhea treatment to prevent reinfection or partner transmission.
“We Both Got Treated. But I Got It Again.”
Ana, 24, tested positive for chlamydia after routine screening. She told her partner, who also got tested and treated. They avoided sex for a week as instructed, but on day eight, Ana noticed new discharge and itching. A second test came back positive again.
“I felt stupid, like we did something wrong. But the doctor said it happens all the time, even one day too soon can be enough.”
In Ana’s case, reinfection wasn’t about blame, it was about timing. Even when both partners follow protocol, early resumption of sex can risk incomplete bacterial clearance. It’s frustrating, but common.
If you’ve been treated, or your partner has, and new symptoms are appearing, retesting is not overkill. It’s self-care.

People are also reading: How Soon Do Cold Sores Start After Herpes Exposure?
Confusing Symptoms That Aren’t STDs (But Feel Like It)
Here’s where things get complicated. Not every burn, itch, bump, or discharge is caused by an STD, but that doesn’t make it imaginary. Vaginal yeast infections, bacterial vaginosis (BV), urinary tract infections (UTIs), and even hormonal shifts can mimic STD symptoms exactly.
In men, non-gonococcal urethritis (NGU), often caused by irritation, bacteria other than chlamydia/gonorrhea, or even vigorous sex, can produce discharge or burning. In women, BV can cause fishy odor and discharge but won’t show up on STD tests. And herpes can be present with no visible sores, or with symptoms mistaken for ingrown hairs or razor burn.
If you tested negative for common STDs but your symptoms continue, consider asking your provider about other conditions that require different types of testing (vaginal pH test, urine culture, pelvic exam, etc.).
Next, we’ll walk through how to decide whether to retest, wait it out, or explore other causes, and how to take action without spiraling into fear.
Should You Retest? A No-Shame Decision Tree
If you’re here wondering what your next move should be, take a breath. You don’t need to figure it all out at once. Here’s a simplified way to think through your next step, without judgment, panic, or paralysis.
Scenario 1
You tested less than 7 days after a possible exposure and now have symptoms.
- Retest after the window period. The first result may have been too early to catch anything.
Scenario 2
You tested 2–3 weeks after exposure and your symptoms have changed or worsened.
- Retest with a lab-grade or multi-STD test kit. You may have been exposed to more than one infection or used a lower-sensitivity test the first time.
Scenario 3
You were treated but resumed sex too soon, or your partner wasn’t treated.
- Get retested. Reinfection happens, even when you're careful.
Scenario 4
Your symptoms don’t match any STD you were tested for.
- Consider non-STD causes. UTIs, yeast, BV, hormonal changes, or irritation may be involved. Ask your provider about broader diagnostics.
Scenario 5
You have new symptoms after a new partner.
- Test again, and talk openly. Many infections are silent at first. A combo test panel may be best.
The bottom line: If something still feels wrong, it’s okay to investigate again. You’re not being paranoid, you’re listening to your body.
Which Test Is Best for Round Two?
If you're thinking about retesting, don't just do the same thing again. Pick a test that works with your schedule, your symptoms, and your level of exposure. Here is a breakdown to help you choose the best method:
Figure 2. Choosing the right test depends on your exposure, timeline, and whether this is a retest or new concern.
You Deserve Answers, Not Anxiety
If your head keeps spinning, peace of mind is one test away. Whether you’re dealing with a possible reinfection, lingering symptoms, or just uncertainty, retesting puts you back in control.
This at-home combo test kit checks for the most common STDs discreetly and quickly, no waiting rooms, no judgment, just real answers in your own hands.
Don’t stay in limbo. You know your body. If something still feels off, trust yourself.
FAQs
1. Can I really test negative and still have an STD?
Yes, and it’s more common than most people realize. Think of it like this: your test is a snapshot, not a movie. If you test too soon, your body might not have built up enough “evidence” for the test to catch. It doesn’t mean you’re paranoid. It means you’re paying attention.
2. My symptoms came back after treatment, did the meds not work?
Not necessarily. Some symptoms stick around even after the infection’s gone. For example, your urethra or cervix might still be irritated after the bacteria are killed off. But if things feel worse, or just weird in a new way, it’s smart to retest. Reinfection happens more than anyone wants to admit.
3. Could this be a brand new infection?
If you've had sex since your last test, even with someone you trust, yep, it’s possible. Reinfection doesn’t mean you did something wrong. It just means life kept happening. STDs don’t come with flashing lights or warning beeps. Sometimes, they just… show up again.
4. When should I retest after a scare or new partner?
Depends on what you’re testing for. For chlamydia and gonorrhea, wait 7–14 days. For HIV, 2–6 weeks depending on the test type. Herpes? That one takes patience, antibody tests usually need 12+ weeks. If you’re not sure, use a combo panel that covers the major ones.
5. Can anxiety mess with my body enough to mimic STD symptoms?
Oh, absolutely. Anxiety is a shapeshifter, it can give you pelvic pain, itching, burning, weird discharge, even muscle aches. But here’s the thing: don’t assume it’s “just stress” until you’ve tested. Rule things out so your brain can chill.
6. What if it’s not an STD at all?
Then you're still doing the right thing by asking. Yeast, BV, UTIs, even shaving irritation or hormonal shifts can feel alarmingly STD-like. If your tests are clean but your symptoms aren’t gone, ask about a pelvic exam or urine culture. Your body’s still trying to tell you something.
7. Is it okay to use a home test the second time around?
Totally. In fact, a lot of people feel more comfortable retesting at home. Just make sure you're using a reputable test that fits your window period. A combo panel is a solid bet when you're not sure what you’re dealing with.
8. There was a faint line on my rapid test, does that count?
Yep. Even a faint line usually means the test found what it was looking for. It's not like a pregnancy test where “sort of positive” can mean “maybe.” With STD tests, a line’s a line. Time to follow up with a confirmatory test if you’re unsure.
9. I don’t want to freak out my partner. How do I bring this up?
Try honesty without blame. Something like, “Hey, I got tested recently, but I’ve still got some symptoms. I’m retesting just to be safe, and I wanted you to know.” You’re not accusing them, you’re protecting both of you. And if they care, they’ll get it.
10. Could antibiotics make my test come back negative even if I’m not cleared?
They can, actually. If you start antibiotics before testing, they might lower the bacterial load just enough to sneak past the test. That’s why it’s ideal to test before you take meds, or wait 3–4 weeks after treatment to check that everything’s truly cleared.
You Know Your Body, Trust That
If your head keeps spinning, you're only one test away from peace of mind. Retesting gives you back control, whether you're worried about getting sick again, still having symptoms, or just not knowing what to do.
Don't keep playing the guessing game. Take the test again with a private kit, talk to a doctor, or look into other testing options. You are not the only one who wants answers, and you are not wrong for wanting them.
This FDA-approved combo test kit can check for the most common STDs from the privacy of your home, fast, accurate, and judgment-free.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. CDC 2021 STD Treatment Guidelines
2. STD Diagnosis and Treatment – Mayo Clinic
3. Syphilis in Alberta, 2017–2020 | Canada Communicable Disease Report
4. Syphilis Outbreak Information | Alberta Health Services
5. Syphilis Tests – MyHealth Alberta
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: L. Singh, MPH | Last medically reviewed: December 2025







