The Truth About Retesting: Why One STD Test Isn’t Always Enough
Quick Answer: Chlamydia doesn’t always cause a burning sensation when you pee, especially in women. Many cases are asymptomatic, making routine testing essential even without obvious symptoms.
Why It Matters: One Symptom, Two Very Different Realities
Janelle, 24, thought it was just a mild UTI. There was no burning, just a dull ache. She brushed it off. Three months later, she was treated for pelvic inflammatory disease (PID), a common complication of untreated chlamydia. Meanwhile, Eric, 27, felt a sharp sting every time he urinated. He assumed it was dehydration, until a routine test confirmed he’d been carrying the infection for weeks.
Burning during urination is one of the most searched STD symptoms on Google. But its presence, or absence, doesn’t tell the full story. In people with penises, urethral inflammation from chlamydia is more likely to be immediately noticeable. In people with vaginas, the infection can sit higher in the reproductive tract with no immediate irritation.
And that’s why this article matters. Because relying on burning pee to “diagnose” yourself at home is a dangerous game, one that can lead to delayed testing, untreated infections, and long-term reproductive consequences.

People are also reading: How to Tell a Hookup You Had an STD After the Fact
What Chlamydia Actually Does to Your Body
Chlamydia is caused by the bacterium Chlamydia trachomatis. It primarily infects mucous membranes in the urethra, cervix, rectum, and throat. It spreads through unprotected vaginal, anal, and oral sex, and can be passed even when the person has no symptoms.
When chlamydia enters the body, it targets epithelial cells, the ones lining your reproductive and urinary tracts. This can trigger an immune response: swelling, irritation, and discharge. If the urethra is affected, the result may feel a lot like a UTI. But if the infection stays in the cervix or throat, there might be zero pain during urination.
According to the CDC, up to 90% of women and 50% of men with chlamydia have no symptoms at all. That’s not a typo. The majority don’t know they’re infected, until complications arise or a partner notifies them.
Burning When You Pee: How It Shows Up in Men vs Women
Let's get down to business. This is what burning while urinating looks like in different bodies and why it happens more often in some than others.
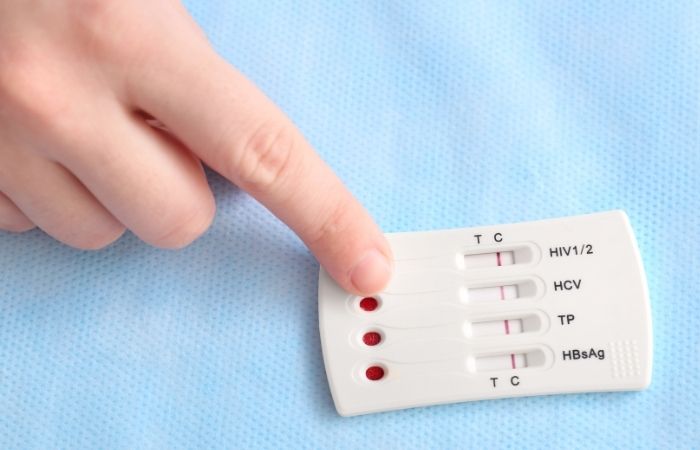
Figure 1. How likely burning urination is with chlamydia by anatomy and why it varies. Note that hormonal changes and anatomy after gender-affirming care may impact symptom presentation and testing recommendations.
When Burning Doesn’t Mean Chlamydia (And When It Might)
The problem with symptom-chasing is this: burning while peeing can mean dozens of different things, or nothing serious at all. It might be a UTI, dehydration, friction, irritation from soap, or even stress-related bladder spasms. But when chlamydia is the cause, it’s often misread as a urinary tract infection, especially in women.
Studies show that over 20% of people treated for UTIs in urgent care settings actually had an underlying STD. Many were never tested because they didn’t report having new partners, or felt too ashamed to bring it up.
This overlap leads to misdiagnosis. The antibiotics for UTIs and chlamydia aren’t always the same. Some will clear both. Others won’t. If your pee still burns after finishing antibiotics, or you never had burning but your partner tests positive, it’s time to test again, no matter how “fine” you feel.
Order a discreet chlamydia rapid test kit if you’ve had any exposure or are unsure what’s causing your urinary symptoms. Results are quick, private, and easy to read at home, no awkward conversations required.
Why “No Burning” Doesn’t Mean “No Chlamydia”
It’s a dangerous myth, especially for women and people with vaginas. If there’s no burning, no discharge, and no visible sign of trouble, many assume they’re safe. But chlamydia is notorious for hiding. According to a study in Sexually Transmitted Infections, nearly 70% of chlamydia infections in women are asymptomatic. That means the infection can silently move from the cervix into the uterus, fallopian tubes, or ovaries, sometimes causing irreversible damage before it’s ever discovered.
For men, it’s more likely to show symptoms, but not guaranteed. Some report a slight irritation they mistake for soap burn. Others feel nothing until a partner tells them to get tested. That’s why relying on pain (or lack of it) isn’t just risky, it’s actively misleading.
And yes, even if your partner had symptoms and you don’t, you can still be infected. Chlamydia doesn’t manifest equally. That’s why testing regularly, after any new partner or unprotected exposure, is essential regardless of what your body seems to be telling you.
Burning After Sex: What Else Could It Be?
Maybe you don’t have chlamydia. Maybe you tested, and it was negative. But something still burns after sex. Here are some other common causes to consider, and why they matter.
Figure 2. Common reasons for pain after sex. Keep in mind that some non-STD conditions can cause similar pain, but testing is still important to rule out infections that don't show up in tests, like chlamydia or trichomoniasis.
What If the Burning Comes and Goes?
This one trips people up constantly: intermittent burning. It stings in the morning but not later. Or it shows up after sex, then vanishes for days. What does it mean?
Burning that comes and goes could be the result of several overlapping factors: mild dehydration, low-level inflammation, irritation from condoms or toys, or yes, an early-stage STD. Many people report waxing and waning symptoms during the first few weeks of infection. That’s why a single “good day” shouldn’t be taken as proof you’re in the clear.
If your symptoms fluctuate or feel mild, it’s even more important to test. A combination STD test kit can screen for chlamydia and other common infections in one go, saving you from the cycle of guessing and Googling.
“I Had Zero Symptoms, But I Was Positive”
Daniel, 31, was in a monogamous relationship until recently. After a new partner, he started researching STD testing. “I felt fine,” he said. “No burning, no discharge, nothing weird.” But he tested anyway. The result? Positive for chlamydia. His partner had no idea either, she was symptom-free, too.
“It was a wake-up call,” Daniel says. “We both assumed we'd know if something was wrong. I was lucky I caught it early, before it turned into something worse.”
This story isn’t rare. It’s exactly why providers urge people to test between partners, even if everything seems normal. Symptoms aren’t reliable. The infection doesn’t wait for pain to start doing damage.
STD Test Kits offers private testing options you can use from home. Whether you’re in between partners, dealing with confusing symptoms, or just want peace of mind, testing puts you back in control.
People are also reading: Scared to Have Sex Again After an STD? Here’s the Real Talk You Need
Why Gender Shapes How Chlamydia Feels
To understand why the symptoms are so different between men and women, we first have to discuss anatomy. In people with penises, the urethra is longer and more exposed to the outside environment. With that said, during sexual transmission of chlamydia through the urethral tip, it irritates the lining of the urethra. Burning sensations, itching, or discharge often appear rather quickly, sometimes even within a week.
But for people with vaginas, the urethra is shorter and sits close to the vaginal and anal openings. Chlamydia usually infects the cervix first, not the urethra. That means many don’t feel the telltale burn unless the infection spreads to the urethra or bladder. This is also why chlamydia is often mistaken for a yeast infection or UTI, especially if there’s abnormal discharge or pelvic pressure.
What’s more, many women don’t even know where their urethra is or what sensations count as “not normal.” Combine that with social messaging that tells them to ignore pain during sex, and you have a perfect storm of missed infections and silent suffering.
The medical system contributes too. Studies have shown that cis women and nonbinary patients are less likely to be offered STD testing when presenting with burning pee than men, because providers often assume a UTI is the most likely cause. That assumption can delay accurate diagnosis by weeks or months.
How Long After Sex Can You Feel Burning from Chlamydia?
Let’s talk timing. Chlamydia’s incubation period, the time between exposure and the first symptoms, is typically 1 to 3 weeks. So if you feel burning just a few hours or a day after a hookup, it’s likely something else (like friction or a UTI). But if discomfort starts 7–14 days later, that’s the danger zone for chlamydia-related symptoms.
Of course, many people never feel symptoms at all. That’s why the World Health Organization and CDC both recommend screening for chlamydia at least once a year if you're sexually active, and more often if you’ve had new partners, symptoms, or a known exposure.
If you suspect exposure and are in the 1–3 week window, it’s safe to test now, but if you test too early and it's negative, retest after two weeks to be sure. Order your test kit with timing in mind. Don’t wait for symptoms, wait for accuracy.
What If You Took Antibiotics for a UTI, But Still Have Burning?
This happens more than you’d think. A provider assumes it’s a UTI, prescribes nitrofurantoin or trimethoprim-sulfamethoxazole, and the symptoms go away, or sort of go away. But the underlying infection may still be there.
Some antibiotics prescribed for UTIs don’t treat chlamydia effectively. Others may temporarily suppress symptoms without fully clearing the bacteria. If the burning returns or shifts, or if your partner tests positive for chlamydia, you’ll need a proper diagnostic test and targeted treatment, usually doxycycline for 7 days.
We’ve seen users delay true diagnosis by weeks because of partial relief from the wrong antibiotic. If you’ve taken antibiotics but didn’t test for STDs, you’re not done yet. Confirm your status with a test built for chlamydia, not just for urinary bacteria.
FAQs
1. Does chlamydia always burn when you pee?
Nope, and that’s where a lot of people get tripped up. For some, it feels like peeing acid. For others? Nothing. No burn, no sting, no warning sign. That’s especially true for folks with vaginas, where the infection might hit the cervix first and skip the urethra altogether.
2. If I don’t feel any symptoms, does that mean I’m in the clear?
Not even close. Chlamydia is stealthy, up to 90% of women and 50% of men never feel a thing. You can carry it for weeks or months without knowing, which is how it keeps spreading. No symptoms ≠ no infection.
3. How soon after sex would chlamydia start burning?
If it’s going to burn, it usually starts 7 to 21 days after exposure. Not the next morning. If you’re feeling the fire within hours, it’s probably something else, like friction, irritation, or a UTI. But two weeks later? That’s prime chlamydia territory.
4. So if I feel burning, it must be chlamydia?
Not necessarily. Burning pee is like the fever of sexual health, super vague. Could be a UTI, trichomoniasis, soap irritation, a yeast infection, or just not drinking enough water. That’s why guessing is risky and testing is clarity.
5. Can UTI meds cure chlamydia?
Sometimes, but not reliably. Some antibiotics hit both infections, others don’t. If you were prescribed something like nitrofurantoin and your symptoms didn’t fully go away, or came back, you could be dealing with an STD underneath it all.
6. What if my partner tested positive and I feel fine?
You could still be infected. Chlamydia doesn’t need to make you miserable to be real. If you’ve had unprotected sex, even once, testing is your move, not because you feel guilty, but because you care about your body and your partner.
7. Can I get chlamydia from oral sex?
Yep. It’s less common than genital-to-genital transmission, but chlamydia can live in the throat and get passed that way, especially if you’re giving oral to someone with an active infection. And surprise: throat chlamydia usually has zero symptoms.
8. I tested negative, but the burning’s still happening. What now?
First, check when you tested. If it was too early (like less than a week after exposure), retest after 14 days. If your timeline was solid, consider other causes: yeast, BV, allergies, even stress. But don’t stop digging, your body’s trying to tell you something.
9. How can I tell if it’s a UTI or an STD?
You really can’t, just by feel. They both cause burning, urgency, pressure. Sometimes a UTI is just a UTI. But if you’ve had new sexual partners, skipped condoms, or your symptoms aren’t clearing up with treatment? Test for STDs too. Always better to know.
10. Is it awkward to tell someone I might have chlamydia?
Sure, it can be. But it’s also incredibly brave. A simple “Hey, I just got tested and something came up” can protect them and start a whole new level of honesty. If you’re nervous, use an anonymous partner notification service or test together. No shame, just facts.
You Deserve Answers, Not Assumptions
Here’s the truth: pain doesn’t always show up when there’s an infection. And absence of pain doesn’t mean absence of risk. Chlamydia is a master of staying silent, especially in women, and burning pee is just one part of a much bigger picture.
If you've had unprotected sex, feel uncertain, or even just want peace of mind, testing is care. Not confession. Not judgment. Just clarity.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. World Health Organization – Chlamydia Fact Sheet
2. Planned Parenthood – Chlamydia Overview
3. Mayo Clinic – UTI Symptoms and Causes
4. Chlamydia Screening & Treatment Guidelines | CDC
5. Chlamydia: Symptoms, Causes & Testing | Mayo Clinic
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on the prevention, diagnosis, and treatment of STIs. He synthesizes his clinical expertise with a no-nonsense, sex-positive approach and is dedicated to extending access to readers in urban and off-grid settings alike.
Reviewed by: S. Romero, FNP-C | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.







