Quick Answer: Gonorrhea and chlamydia often cause no symptoms in men. Discharge isn’t guaranteed. Burning, testicle pain, or even no symptoms at all are common, so testing is the only way to know.
Why This Article Matters, And Who It's For
This guide is for men who’ve ever googled “STD symptoms with no discharge” or stared into the toilet wondering if that tingle was just irritation, or something worse. Whether you’ve had a one-night stand, recently started dating again, or simply want to stop guessing, this article will help you separate fear from fact.
It’s also for the guys who assume they’re “fine” because they’re not leaking or in pain. Silent STDs can still spread, and cause long-term damage. We’ll unpack what gonorrhea and chlamydia really feel like in men (if anything), what symptoms overlap, what doesn’t show up at all, and when to test even if you think you're in the clear.

People are also reading: My Partner Has HPV. Am I at Risk, And What Should I Do Next
What Men Think Gonorrhea and Chlamydia Feel Like
Most men have a mental checklist of what “having an STD” should feel like: thick discharge, painful urination, maybe a rash or visible sore. That’s partly true, but it’s also dangerously incomplete.
Here’s what the assumptions look like:
Figure 1. Common myths about STD symptoms in men, and the clinical reality.
The truth? Discharge is just one piece of the puzzle. In real-world cases, symptoms are often vague or nonexistent. And by the time signs show up clearly, the infection may have already spread to partners, or deeper into the reproductive tract.
Chlamydia vs Gonorrhea in Men: How the Symptoms Differ (And Overlap)
Let’s break it down. While chlamydia and gonorrhea are caused by different bacteria, they infect the same areas in similar ways, mainly the urethra, rectum, and throat. Here’s how they compare in men:
Figure 2. Symptom comparison: chlamydia vs gonorrhea in men.
Symptoms alone can’t tell you which infection you have, or if you have one at all. Testing is essential. Even more so because co-infections are common. One study found that up to 30% of men diagnosed with gonorrhea also had chlamydia:contentReference[oaicite:1]{index=1}.
If you're wondering whether it's time to get tested, here’s your answer: it is. This at-home combo test kit checks for both infections quickly and discreetly.
Case File: “I Didn’t Think It Was an STD. I Thought It Was a UTI.”
Devon, 34, had just started seeing someone new. A few days after oral and vaginal sex, he felt a dull ache in his lower abdomen and a bit of stinging during urination. He didn’t see any discharge. He assumed it was a urinary tract infection, rare for men, but not impossible. His doctor even prescribed antibiotics for a suspected UTI without testing. Weeks later, his girlfriend tested positive for gonorrhea.
“I felt like an idiot,” Devon said. “I didn’t even know guys could get gonorrhea without symptoms.”
That’s the problem with relying on symptoms, or assumptions. Gonorrhea and chlamydia in men can mimic other things: irritation from lube, post-sex friction, dehydration, or mild prostatitis. And since UTIs are less common in men, misdiagnosis can delay treatment, and increase the risk of passing it on.
In one study, fewer than half of men who tested positive for chlamydia reported any symptoms. Many assumed it was just irritation from soap, a rough hookup, or a “weird pee day.” These are real quotes from Reddit threads, and they echo the same pattern: false reassurance leads to skipped testing.
When the Symptoms Are in Your Head (But the Infection Is Real)
Anxiety can play tricks. The absence of pain feels like proof nothing’s wrong. But that’s not how these infections work. Gonorrhea and chlamydia can incubate for days, or even weeks, without triggering obvious signs. And when symptoms do show up, they might be brushed off as stress or dehydration.
There’s also the reverse problem: psychosomatic symptoms. Men who fear they’ve caught something may suddenly notice tingling, itching, or phantom aches that mimic STD symptoms but aren't linked to infection. Only testing can cut through that fog.
Here’s a breakdown of how symptom timing typically plays out:
Figure 3. Symptom onset timing and asymptomatic rates in men.
Notice how much overlap there is. Even if you know when exposure happened, you can’t tell which STD you might have, or whether you’re one of the many men who won’t feel a thing.
What If It’s Just a Rash, Itch, or Feeling "Off"?
Many men ignore mild urethral irritation, chalking it up to rough sex, masturbation, or clothing. But even subtle symptoms can indicate infection. Here are real user-reported signs that turned out to be chlamydia or gonorrhea after testing:
- A “slight tightness” during urination that came and went
- Unexplained testicle ache after ejaculation
- A tingling feeling at the tip of the penis, especially in the morning
- Morning-only discharge that dried before it was noticed later
- Redness around the urethral opening without pus
The bottom line? STD symptoms don’t always scream. Sometimes they whisper. Or hide altogether.
Real Talk: Why Men Delay Testing (and Why It Backfires)
There’s a lot of cultural baggage around STDs. For men, it often looks like this: “I feel fine, so I must be fine.” Or worse: “If I get tested, it means I did something wrong.” That shame-based logic is part of what lets infections spread undetected.
We’ve heard every reason: It’s inconvenient. It’s awkward. It feels like overreacting. But here’s what happens when you don’t test:
- You may infect partners without knowing it
- You might not get treated until symptoms get worse or complications arise
- You could risk long-term issues like epididymitis or infertility (yes, it’s rare, but real)
And if you do eventually test positive, you’ll probably wish you’d known sooner. The good news? You don’t have to wait in a clinic or explain yourself to anyone. You can order a combo test kit and handle it from home.
STD or Something Else? What It Could Be (and What It’s Not)
When you’re dealing with vague symptoms, burning, irritation, or just a sense that something’s off, your mind jumps to worst-case scenarios. But just as often, it jumps to the wrong explanation. Here’s where a lot of men misdiagnose themselves:
Figure 4. Common misdiagnoses when STDs present with subtle or no discharge in men.
The problem is, most of these conditions can’t be reliably told apart without testing. You can’t guess your way out of it. That’s why guidelines from the CDC and NHS recommend regular testing for sexually active individuals, especially if you’ve had a new partner, multiple partners, or unprotected sex.
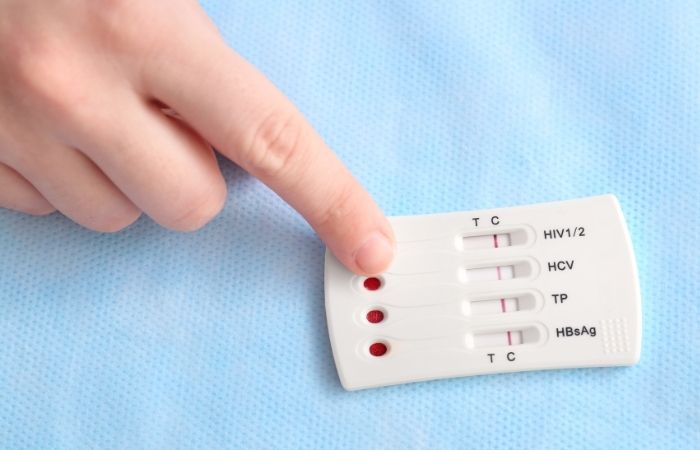
At-Home STD Testing for Men: What to Know
You don’t need to wait for symptoms to get tested, and you definitely don’t need to feel embarrassed about it. With today’s at-home STD tests, you can screen for both chlamydia and gonorrhea from the privacy of your own bathroom.
Here’s how it works:
- Choose a combo test kit that checks for both infections.
- Follow the included instructions, usually a urine sample or swab.
- Get results within minutes for rapid kits, or a few days if using a mail-in lab kit.
Every kit comes in discreet packaging, no labels, no branding. It’s designed for peace of mind, not judgment.
Privacy tip: Many users ship tests to a friend’s house, PO box, or use vacation addresses. You’re in control of your timeline and your data.
People are also reading: Can You Get HPV Without Cheating?
When to Test: Timeline After Exposure
If you’ve had a recent exposure, oral, vaginal, or anal, you might be tempted to test the next day. But testing too early can lead to false negatives. Here’s what you need to know about timing:
Figure 5. Recommended testing windows after sexual exposure.
If you tested early and got a negative but still have symptoms, or just a gut feeling, retesting at day 14 or later can offer confirmation. Don’t let one result be your final answer if something still feels off.
Your Next Move: Answers, Not Anxiety
When it comes to chlamydia or gonorrhea, silence isn’t safety. These infections don’t always shout. Sometimes they show up with no discharge, no pain, no warning, and still do damage.
But you don’t have to live in limbo. Testing puts you back in control. And today, that’s easier and more private than ever. Don’t wait until your partner gets a call, or until your symptoms get louder.
FAQs
1. I don’t see discharge, am I still supposed to be worried?
Yep. Discharge isn’t some golden rule of STDs. In fact, chlamydia often shows up with zero discharge at all. And even gonorrhea, which is more likely to cause it, can fly under the radar, especially early on. So no goo doesn’t mean no problem. If you had unprotected sex, it's still worth getting checked.
2. How soon after sex would symptoms start if I caught something?
It depends. Gonorrhea can start showing signs in as little as 2–5 days. Chlamydia tends to take its sweet time, sometimes 1 to 3 weeks. But here’s the kicker: lots of guys never get symptoms at all. That’s why relying on “feeling fine” can backfire fast.
3. It stings a little when I pee, but only sometimes. Could that be an STD?
Absolutely. That “sometimes” is exactly what trips people up. STDs like gonorrhea and chlamydia don’t always scream. Sometimes they whisper. Burning that comes and goes, feels minor, or only shows up in the morning? Still counts. Don’t wait for it to get worse.
4. I thought I had a UTI. Turns out, it was gonorrhea. How common is that?
More common than you think, especially since UTIs in cis men under 50 are pretty rare. Doctors sometimes misdiagnose early STD symptoms as UTIs when they skip testing. If you’ve got burning, urgency, or pelvic weirdness, STD testing should always be on the table.
5. Do I really need to test if I don’t have symptoms?
Yes. 100% yes. Most of the time, when men pass STDs to partners, they had no clue they were infected. That’s how silent infections work, they keep moving unless you stop them. Testing isn’t overkill. It’s ownership.
6. I tested 5 days after sex. Negative. Am I in the clear?
Not necessarily. Early testing is fine if you’re anxious, but bacteria like chlamydia might not be detectable that soon. The sweet spot is 10–14 days post-exposure. If you tested early, plan to test again. Peace of mind is worth a second look.
7. Can these infections just go away on their own?
Nope. They don’t pack up and leave just because you’re not symptomatic. Chlamydia and gonorrhea stick around until they’re treated, and they can do real damage over time. Antibiotics knock them out fast, but ignoring them doesn’t.
8. I used a condom. Doesn’t that protect me?
Mostly, yes, but not completely. Condoms lower risk big time, but they’re not bulletproof. STDs can spread from skin contact, oral sex, or areas the condom doesn’t cover. You did the right thing, but if you’ve got symptoms (or a gut feeling), testing is still smart.
9. Could a sore throat be from oral sex?
Actually, yes. Both gonorrhea and chlamydia can infect the throat, especially from unprotected oral. Most guys don’t get sore throats from it, but some do. It’s usually mild, if anything, but it’s another reason to include throat testing when you can.
10. What if I test positive, how do I tell my partner?
With honesty and zero shame. STDs don’t mean you’re dirty or reckless. They mean you’re human, and now you’re handling it. Start with: “I got tested and something came back positive. I want you to be safe too.” Keep it simple. You don’t have to do it alone, anonymous text services exist if you need backup.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
2. About Sexually Transmitted Infections (STIs) | CDC (many STIs are asymptomatic)
3. Getting Tested for STIs | CDC (importance of testing when signs are silent)
4. Know the Facts About STIs | CDC (you can’t tell by symptoms alone)
5. STD Symptoms Overview | Mayo Clinic (some infections are mild or asymptomatic)
About the Author
Dr. F. David, MD is a board-certified infectious disease doctor who focuses on preventing, diagnosing, and treating STIs. He combines clinical accuracy with a straightforward, sex-positive approach, and he wants to make it easier for readers to get to know him in both urban and rural areas.
Reviewed by: Sophia Ruiz, RN, MPH | Last medically reviewed: December 2025





