Her Pap Came Back Abnormal. What You Need to Know as a Man
Quick Answer: Yes, you can get HPV without cheating. The virus can lie dormant for years without symptoms, meaning it may have come from a past partner, even a decade ago. This makes “blame timelines” unreliable and misleading.
What Is HPV, and Why Is It So Common?
HPV is the most common sexually transmitted infection in the world, affecting nearly everyone who’s ever had sex. There are more than 100 types of HPV, and about 40 of them affect the genital or oral areas. Some cause genital warts, others are linked to cervical cancer and other types of cancers, but most types cause no symptoms at all and clear on their own.
According to the CDC, almost everyone will contract at least one strain of HPV at some point, usually within the first few years of becoming sexually active. But the virus doesn’t always show up on tests right away. In many cases, it stays completely silent.
That silence is where the confusion, and the heartbreak, often starts.

People are also reading: Can You Get HPV Without Cheating
How Long Can HPV Stay Dormant in the Body?
One of the most misunderstood things about HPV is that it can remain dormant in the body for years, sometimes decades. Dormant means the virus is present but inactive, causing no symptoms and often undetectable by standard tests. It can become active again due to stress, immune changes, hormonal shifts, or simply without any obvious trigger.
In one landmark study published in Sexually Transmitted Diseases Journal, researchers confirmed that HPV can be “reactivated” years after the original exposure, especially in people over 30. In practical terms, this means you might test positive now for a virus you were exposed to 5, 10, or even 20 years ago.
This makes it nearly impossible to pinpoint “who gave it to who”, and even harder to use HPV test results as evidence of recent infidelity.
“We’ve Been Together 9 Years, Why Now?”
Marisol, 34, found out she had HPV after a routine Pap smear. She and her husband had been together nearly a decade, and she had never tested positive before.
“I immediately thought he cheated. I even confronted him. He was stunned, and honestly, so was I.”
After speaking with her OB-GYN, Marisol learned about HPV’s latency. Her doctor explained that she could’ve carried the virus since her early twenties, and it simply became detectable now. Her husband also might’ve had it silently, without knowing, there’s no routine test for HPV in men.
“We had a hard talk, but in the end, it made us stronger. The test wasn’t a betrayal, it was a biological echo.”
Marisol’s story isn’t rare. In fact, it reflects what doctors see every day: HPV doesn’t follow moral timelines, and its biology isn’t designed to be a lie detector.
How Is HPV Transmitted?
HPV spreads through skin-to-skin contact, most commonly during vaginal, anal, or oral sex, but not exclusively. It doesn’t require ejaculation or even penetration. Genital contact alone can transmit the virus, and condoms don’t fully protect against it (though they do reduce risk).
You can get HPV from:
Table 1. Common transmission routes for HPV and associated risk levels.
Because of how easily HPV spreads, and how long it can hide, most people are exposed long before they’re ever tested. That’s why it often appears in monogamous relationships without new exposure.
Why HPV Doesn’t Work Like an “Affair Detector”
Unlike chlamydia or gonorrhea, where infections typically show up within a few weeks and can be linked to recent sexual activity, HPV doesn’t play by the same rules. Its long latency period means it can quietly persist in the body without ever producing symptoms, and then suddenly appear on a Pap smear or DNA test years later.
That’s why using HPV test results to judge a partner’s fidelity is both emotionally risky and scientifically shaky. The virus’s timeline is so inconsistent that even doctors can’t reliably determine when it was acquired. As Planned Parenthood puts it: “HPV can be present without symptoms and stay in your body for a long time. You or your partner may have had it for years without knowing.”
If it’s your first positive test, it doesn’t mean your partner is cheating, it may mean the virus finally reached detectable levels after years of staying quiet. Or it could have reactivated due to stress, illness, or immune system changes. This is especially common for people over 30, when dormant HPV infections are more likely to resurface.
Can Men Be HPV Carriers Without Knowing?
Yes, and this is a huge part of the puzzle. Currently, there is no FDA-approved HPV test for men unless there are visible symptoms like genital warts. This means most men who carry the virus will never know it, and may unknowingly pass it to partners.
HPV in men is often asymptomatic, and even when it causes symptoms, they’re usually mild or go unnoticed. That’s why it’s entirely possible for someone in a monogamous relationship to be a silent carrier, especially if they were exposed before the current relationship began.
So when someone asks, “How did I get HPV if neither of us cheated?” the answer is often: one of you had it already, but the virus just never made itself known until now.
That’s not betrayal. That’s biology.
HPV Reactivation: What the Research Shows
Let’s get into the science. HPV reactivation isn’t just a theory, it’s been documented in peer-reviewed research. A study published in the Journal of Infectious Diseases followed women who had previously tested negative and then years later tested positive for the same strain of HPV, even though they reported no new partners during that time. Researchers concluded that HPV reactivation is a real and likely common phenomenon.
That means even if you’ve had the same partner for years, a positive HPV result doesn’t automatically equal recent transmission. Instead, it may be an old infection surfacing again, something your immune system had previously kept suppressed.
HPV doesn’t always “stay gone” after your body fights it off. It can hide in your cells and come back later, which makes tracing it like chasing shadows: confusing, frustrating, and ultimately a dead end if you’re trying to prove or disprove loyalty.
When HPV Shows Up in Long-Term Relationships
HPV is often first detected during a Pap smear or an HPV DNA test, sometimes years into a relationship. And that first positive test can feel like a betrayal, even when no one did anything wrong. The emotional whiplash is real, and the doubt it creates can be just as damaging as the virus itself.
But this exact scenario is so common that many OB-GYNs now have standard scripts to explain it. Here’s what Dr. Ana R., a gynecologist in California, tells her patients:
“The number one thing I say is: HPV doesn’t mean anyone cheated. It means you’re sexually active and human. This virus can hide for years and show up out of nowhere. Don’t assume the worst.”
For couples in monogamous relationships, this knowledge can be both comforting and disorienting. On one hand, there’s relief, it doesn’t necessarily mean someone broke trust. On the other hand, it leaves people with questions they may never fully answer. That’s the emotional complexity of HPV: it’s both common and unclear, both medically harmless in most cases and emotionally heavy in the moment.
If you're feeling overwhelmed after a positive result, you're not weak, you're reacting to a deeply misunderstood virus that’s wrapped up in outdated ideas about loyalty and purity. The truth is far messier, and more human.
What to Do Next: Testing, Vaccines, and Talking With Your Partner
If you’ve tested positive for HPV, or your partner has, it’s time to pause, breathe, and make a plan. Here’s what to consider:
Table 2. Action steps after a new HPV diagnosis, whether you're symptomatic or not.
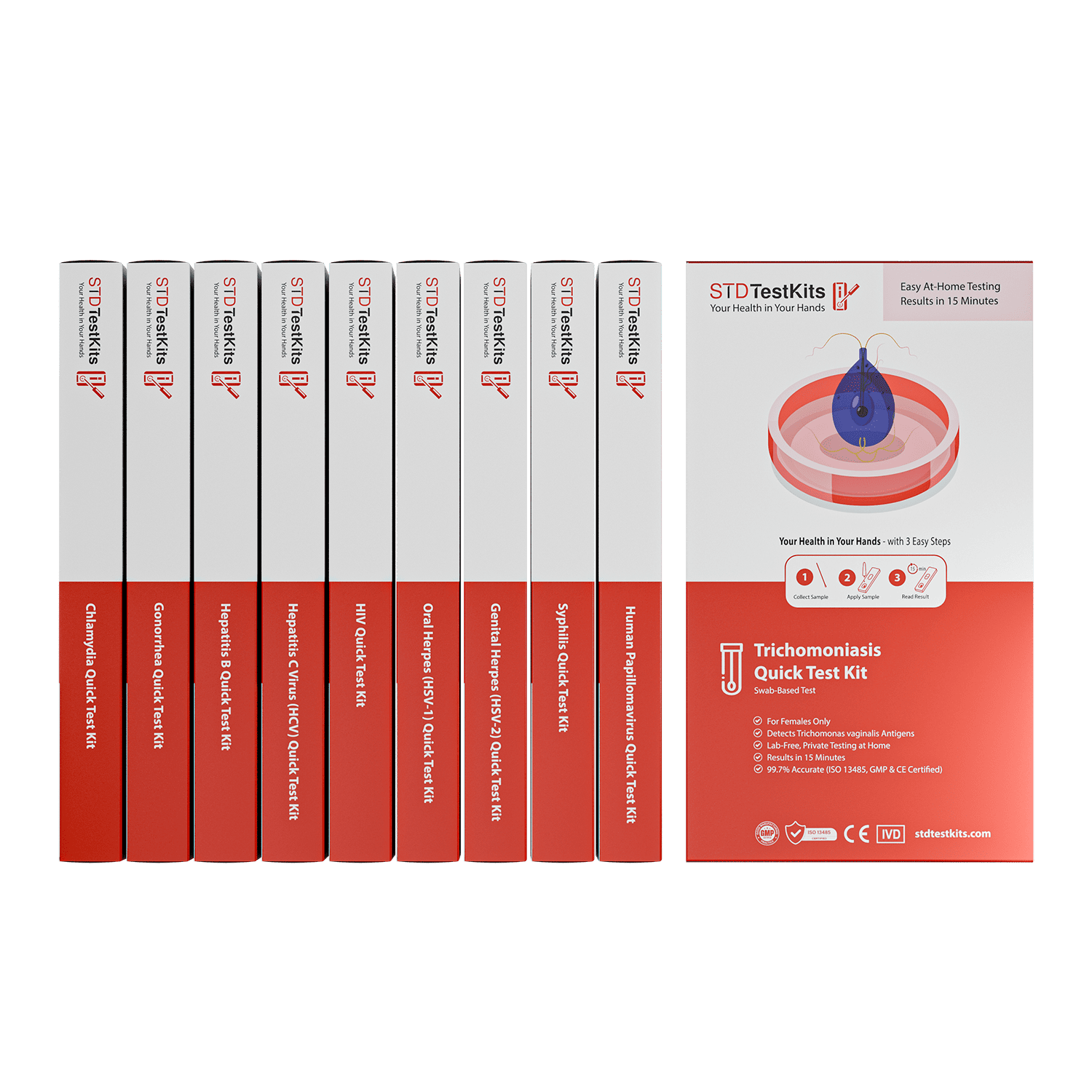
Peace of mind starts with clarity. If you're spinning in questions or fears, a private test can offer relief and direction. You can order a discreet kit right now from STD Test Kits or explore combo kits that screen for multiple infections.
This Isn’t About Blame, It’s About Biology
The idea that STDs are “proof” of cheating is outdated and damaging, but it’s deeply ingrained. For many people, an HPV diagnosis doesn’t just trigger medical questions; it cracks open emotional landmines: fear, betrayal, shame, and confusion. Even if you trust your partner, even if they trust you, the mere appearance of an STI can make you question everything.
But here’s the truth: HPV isn’t a moral infection. It’s a biological one. And biology doesn’t care about relationship labels. It doesn’t track fidelity or remember when the virus arrived. It just does what viruses do, hide, wait, and sometimes reappear.
We’ve been taught to equate sexual health with moral purity. That’s not only scientifically inaccurate, it’s cruel. You can be the most loyal partner in the world and still test positive for HPV. You can have HPV for years and never know. You can pass it unknowingly, and be passed it unknowingly, without anyone lying or cheating.
In that light, an HPV diagnosis isn’t a betrayal. It’s a reminder that our bodies carry history, even when our minds have moved on.
Rebuilding Trust After an Unexpected Diagnosis
For couples, especially those in long-term monogamous relationships, an unexpected HPV result can feel like an earthquake. It’s not just about health, it’s about trust. But rebuilding after that initial shock is possible, and often transformative.
Here’s one story that captures this process:
Daniel, who was 38 years old, had been with his partner for six years when she got a positive test for high-risk HPV. He thought she had cheated on him, and their relationship almost ended. But after reading medical articles and talking to a doctor together, they found out that she probably got the virus from a previous partner and that it had just now shown up.
"I realized I had linked a STI to betrayal. But that was not right. We never talked about the things I had in my past either. This started conversations that we should have had a long time ago."
Daniel's story is powerful because it shows how wrong ideas about HPV can hurt people emotionally. But if you are patient, honest, and learn, relationships don't just last, they get stronger.
If you're having a similar conversation, be careful. Begin with what you already know: HPV is common, can stay dormant for years, and usually has nothing to do with what you've done recently. If you and your partner are both feeling upset, take a break, learn the facts together, and think about going to a therapist or provider to help you talk things over.
Remember: communication builds intimacy. Silence builds suspicion. When it comes to sexual health, honesty, paired with knowledge, is your best ally.

People are also reading: Too Late for the HPV Vaccine? Not Necessarily
Why This Happens So Often (And We Don’t Talk About It)
One reason HPV can feel so devastating is that no one talks about it. Despite being the most common STI in the world, it carries a strange silence. There’s no celebrity campaign, no hashtags, no open dialogues on dating shows or doctor dramas. Instead, HPV lurks in whispers, wrapped in shame and confusion.
Part of that silence is structural: men aren’t routinely tested, so they never know they have it. Part of it is gendered: people with cervixes are told they’re “infected” without any mention of where the virus came from. And part of it is moral: society still treats STDs as proof of poor judgment, even when they’re the inevitable result of being human and sexual.
Here’s what that means in practice: someone gets HPV, feels ashamed, blames themselves, or worse, blames their partner. That leads to broken relationships, anxiety, and avoidance of future care. All because no one explained how normal this virus actually is.
Breaking that silence starts with better conversations, and better access to testing.
At-Home Testing: Taking Back Control (Without the Drama)
If you’re navigating an unexpected HPV diagnosis, or supporting someone who is, one of the most empowering steps you can take is to check your full sexual health status. You don’t need to go to a clinic, sit in a waiting room, or explain your entire sexual history to a stranger. You can test privately, from your home.
STD Test Kits offers discreet, accurate kits for chlamydia, gonorrhea, HIV, syphilis, and more. While there’s no at-home test for HPV itself, you can rule out other STDs that may be present, especially if you’re sexually active or haven’t tested in a while. And that clarity can quiet the mental noise.
If your head keeps spinning, peace of mind is one test away. You can order a combo STD test kit here and take control of your health on your own terms. Fast, discreet, and accurate, without the judgment.
Talking to New Partners About HPV
If you're single or dating, HPV can feel like a difficult subject to bring up. What if they think you're "unclean"? What if they walk away? What if they ask how you got it, and you don’t know the answer?
Here’s the truth: HPV doesn’t define your worth or your desirability. The vast majority of sexually active people will contract it at some point. Talking about it isn’t a red flag, it’s a sign of maturity and respect.
When you do decide to share, keep it factual and confident. You might say:
“Just so you know, I tested positive for HPV in the past. It’s super common and most people have it without knowing. I just want to be transparent because I care about your health too.”
Short. Clear. Compassionate. If they shame you, that’s on them, not on you.
The right person will appreciate your honesty. The wrong one wasn’t worth your energy.
Why HPV Education Should Be Part of Sex Ed
One final truth: we wouldn’t be having this conversation if schools taught HPV the way they should. Most people don't learn about latency, strain types, or how common the virus is until it shows up in their medical records. And by then, it's too late to prevent the fear spiral.
Imagine if students were taught:
- HPV is normal: Almost everyone gets it.
- HPV isn’t proof of cheating: It can stay hidden for years.
- Vaccines help, but aren’t perfect: You can still get non-covered strains.
- Testing is care, not confession: It’s how we stay safe together.
Until then, articles like this one have to fill the gap. If you're here, reading this, you’re already part of a new kind of sex education, one based on science, compassion, and reality.
FAQs
1. I’ve only been with one person. How could I possibly have HPV?
Totally fair question, and you're not alone in asking it. The reality? You can contract HPV from just one partner, even years ago. The virus doesn’t need multiple exposures or a “wild phase” to show up. You could have been exposed the first time you ever had sex, and it just stayed quiet until now.
2. Does testing positive mean my partner cheated?
Not at all. It’s a common panic thought, but medically, it doesn’t hold up. HPV can live in your body for years without a single symptom. That means someone could’ve had it before your relationship began, never knew, and it finally got picked up on a test. It’s not a loyalty test, it’s a virus.
3. How long can HPV stay hidden before showing up?
Honestly? Years. Like, decade-level years. We've seen cases where it popped up 15+ years after someone’s last new partner. It’s a sleeper virus. That’s why trying to “trace it” usually leads to dead ends and unnecessary stress.
4. Can guys get tested for HPV?
Frustratingly, no, at least not in any routine, reliable way. There’s no approved test for men unless they have symptoms like genital warts (and most don’t). So men can carry and pass HPV without ever knowing it. It’s a huge gap in sexual health testing, and one reason so many people are blindsided.
5. Wait, I had HPV years ago. Can it come back?
Yep. It’s called reactivation. Your immune system might’ve pushed the virus into hiding, but that doesn’t always mean it’s completely gone. Illness, stress, hormonal changes, any of these can bring it back to the surface. Doesn’t mean you “caught it again.” Just means it stopped playing possum.
6. Does this mean I’m at risk for cancer now?
Not necessarily. Most HPV infections go away on their own. But high-risk strains can cause cervical or other cancers if left unchecked, which is exactly why Pap smears and HPV testing are so important. Early detection = total game changer. So if your test flagged something, follow up. It’s not panic time, it’s prevention time.
7. Should I tell my partner I tested positive?
Yes, and no, it doesn’t have to be a scary conversation. Try something like: “Hey, my doctor said I tested positive for HPV. It’s super common, and lots of people have it without knowing. I just wanted you to know so we can both stay informed.” Calm, honest, no blame. That’s the vibe.
8. If we use condoms, doesn’t that mean we’re protected?
Condoms reduce the risk of HPV infection, but do not fully prevent it. HPV is transmitted skin to skin, so areas not covered by a condom-for example, the base of the penis or surrounding genital skin-can still allow for viral transmission. It is safer to use condoms, but not foolproof.
9. I got the vaccine, why did I still test positive?
The vaccine paradox, oh. The HPV vaccine protects against the most dangerous strains, such as the ones that cause warts and cancer the most. There are more than 100 types of HPV, and the vaccine doesn't protect against all of them. So yes, you can still get a strain that isn't covered. That being said, people who have been vaccinated usually have fewer problems, so it's still a win.
10. What kind of test should I take now?
If you've tested positive for HPV, your provider will likely follow up with cervical monitoring (like a Pap or colposcopy). But if you want to make sure you’re clear on everything else, an at-home STD test can help. It’s discreet, fast, and doesn’t require an awkward clinic visit. Check out this combo test kit, it’s a good way to quiet the mental spiral.
You Deserve Answers, Not Assumptions
Getting diagnosed with HPV while in a monogamous relationship can feel like your entire foundation just cracked, but science tells a different story. HPV is silent, slippery, and staggeringly common. It doesn’t mean someone lied. It means the human body holds onto things, sometimes longer than we expect.
Whether you're grappling with the emotional fallout, looking for a way to talk to your partner, or simply trying to understand how this happened, you're not alone. Knowledge is your best protection. Compassion is your best tool.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Journal of Infectious Diseases – Evidence for HPV Reactivation
2. Genital HPV Infection — CDC
3. CDC: HPV (Human Papillomavirus) — STI Treatment Guidelines
4. HPV Infection — Symptoms & Causes (Mayo Clinic)
5. The Estimated Lifetime Probability of Acquiring Human Papillomavirus — PMC / NCBI
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: T. Lawson, NP, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.