HIV Rapid Test Errors and Faint Lines: How to Know What’s Real
Quick Answer: STD stigma in LGBTQ+ communities often delays testing, fuels misinformation, and worsens health outcomes, but at-home testing and open dialogue can break the cycle.
What Stigma Actually Feels Like, And Why It Hits Queer Folks Differently
Stigma isn’t just being called “dirty” or shamed outright. Sometimes it looks like a queer woman avoiding the clinic because staff always assume she’s straight. Sometimes it’s a trans man who won’t get tested for chlamydia because the swab they require is dysphoria-triggering. Sometimes it’s just a gay man swiping left on anyone who says “positive” in their bio, not out of malice, but out of fear. That’s the kind of internalized judgment that keeps us quiet.
In a world already obsessed with policing queer bodies, STDs become the perfect excuse to further marginalize. Even within the community. You’re expected to be sex-positive, but not too risky. Knowledgeable, but never infected. Honest, but never vulnerable. The result? A cultural double bind. Either you get tested and face shame, or you stay silent and hope it goes away.
Research substantiates this assertion. A 2023 survey published in the Journal of Adolescent Health indicated that LGBTQ+ individuals were 60% more likely to postpone STD testing due to fear of judgment in comparison to their heterosexual counterparts. Bisexual and transgender participants explicitly indicated avoidance stemming from provider stigma and community silence.
When Sex-Positivity Isn’t Enough: The Limits of Progress
We like to believe that because queer culture champions openness, we’ve somehow transcended STD shame. The truth is more complicated. Sex-positivity gives us the language, but not always the safety. Talking about kinks is celebrated. Talking about your herpes diagnosis? Not so much. Even in activist spaces, infection is often seen as personal failure, not public health.
Take Mateo, a 26-year-old Latinx nonbinary person who shared their experience in a 2024 VICE Health feature. After being diagnosed with gonorrhea, they tried to tell a former partner, someone they’d met through a queer mutual aid network. The response? “Wow, I thought you were responsible.” Mateo didn’t reply. They blocked the number and never disclosed again. “It felt like the price of honesty was social exile,” they said.
This emotional cost, of honesty, of disclosure, is one reason many LGBTQ+ people choose silence. Not because they’re careless. But because they know what happens when you speak. And often, it’s not support. It’s shame. It’s ghosting. It’s gossip.

People are also reading: Everything You’re Afraid to Ask About At-Home STD Tests
Table Talk: The Most Common Stigma Triggers in Queer Spaces
Below is a table capturing some of the most frequently reported reasons LGBTQ+ individuals avoid testing or discussing STDs, drawn from community health reports, Reddit threads, and public health surveys.
Figure 1. Triggers and outcomes of STD stigma in queer spaces.
Why At-Home Testing Changes Everything, But Isn’t the Whole Solution
When you’re afraid of judgment, privacy becomes a lifeline. That’s where at-home STD testing becomes a game-changer. No waiting rooms. No misgendering. No need to out yourself just to pee in a cup. You test on your terms. You stay in control.
For trans and nonbinary folks especially, the ability to collect samples in a familiar, safe environment matters. One trans woman shared anonymously on a Reddit AMA that clinic testing meant enduring two levels of trauma: invasive questions about her genitalia and staff using the wrong pronouns. “I’d rather just not go,” she wrote. At-home kits became her bridge back to care.
You can order a discreet combo test that checks for common STDs like chlamydia, gonorrhea, syphilis, and HIV, all from home. Results come fast. Packaging is non-identifiable. And most importantly, you don’t have to explain your life to anyone just to get protected.
Case Study: “I Didn’t Think Lesbians Could Get STDs”
Amina, 34, had been with women exclusively since college. When she started feeling pelvic pressure and a low fever, she assumed it was stress or maybe a UTI. Her doctor disagreed. Tests came back positive for trichomoniasis.
“I felt so stupid,” she said. “Like, I preach all this feminist health stuff online, but I didn’t even know I was at risk. And no one around me talked about it either.”
Her story isn’t rare. The CDC notes that many queer women are misinformed about STD risk because so much sexual health education is heteronormative. In fact, research from the American Journal of Public Health found that providers often skip full screening panels when patients identify as lesbian, falsely assuming low risk.
The consequences? Silent infections. Missed treatments. And a deepening of the belief that some people just don’t count, or that seeking care makes you less queer, less in control, or less welcome.
Intersectional Pain: When Stigma Meets Race, Gender, and Trauma
STD stigma in queer spaces doesn’t hit everyone the same. If you're Black, trans, disabled, or undocumented, that shame gets compounded by systemic mistrust, past medical trauma, and survival logic. It's not just “go get tested”, it’s “can I afford the risk of being seen here?”
Jamal, a 22-year-old Black gay man in Atlanta, described his experience this way: “In my community, you don’t talk about being sick. You pray, you push through. Telling someone you got an STD? That’s not just embarrassing. It’s risky. It changes how people treat you.”
And if you’re undocumented or don’t have insurance, traditional clinics may feel more like threats than safe spaces. Even when free testing is offered, the forms, the IDs, the waiting rooms, all of it sends a message: this system isn’t built for you. The silence becomes a shield.
For trans people, stigma often fuses with body dysphoria and gender trauma. A vaginal swab or rectal exam test might feel like more than just a procedure; it might feel like a violation. As one trans masc activist put it in a 2025 HuffPost essay: “STD testing saved my life. But I had to survive a panic attack in a clinic bathroom to get there.”
Table: Breaking the Barrier, Stigma vs Solutions
Understanding the common obstacles queer individuals face around STD testing helps us design better tools and support systems. Here’s how the most frequent stigma-based barriers stack up against what’s actually working.
Figure 2. Common LGBTQ+ testing barriers and what’s being done to overcome them.
Creating a Culture of Consent and Clarity, Not Judgment
So how do we undo decades of conditioning that told us to shut up, stay pretty, and never admit risk? We start by changing the story. Instead of treating STDs as proof of recklessness, we treat them as part of life. Like a cold, a cavity, or a sprained ankle, normal, treatable, common.
We normalize status talks, not just when something goes wrong, but before intimacy ever starts. We stop treating “I got tested” like a confession. We make it part of care. Of foreplay, even. We say: “Hey, I test every few months, and I use this kit. Want to test together?”
We also challenge hookup culture’s hypocrisy. It's not radical to demand “clean” partners and then ghost people who disclose. That’s not safety. That’s punishment. Real safety is rooted in information, honesty, and access. Apps and dating spaces need to evolve with us, offering fields for status, retesting dates, or even direct links to resources like the Combo STD Test Kit.
Case Study: “I’m HIV Positive, and Still Worth Loving”
Ravi, 38, was diagnosed with HIV in 2020. He’s virally suppressed, undetectable, and in his words, “healthier than I was before I knew.” But dating? That’s still brutal.
“When I tell people upfront, some block me. When I wait, they say I was dishonest. There’s no winning.”
U=U, Undetectable = Untransmittable, is backed by science. But stigma often lags behind truth. Even in queer spaces that celebrate sex-positivity, people still whisper, ghost, or judge. Ravi’s turned to disclosure scripts and educational resources, including a tattoo that says “U=U.” But even with clarity, the rejection stings.
“It’s not the virus that hurts me,” he says. “It’s the way people treat me because of it.”
His story reminds us that STD stigma isn’t just about infection, it’s about love. Who we believe is worthy. Who we protect. Who we throw away. And how we can change that, one conversation at a time.
Queering Care: What Real Support Looks Like
We often say queer liberation includes sexual liberation, but that only works when care is part of the equation. Real support isn’t just rainbow logos or Pride flags in clinics. It’s culturally competent providers. It’s rapid tests without gendered assumptions. It’s knowing that a positive result doesn’t make you less desirable, less queer, or less loved.
Organizations like Planned Parenthood have expanded LGBTQ+-affirming services across the country. Queer-led health centers in places like San Francisco, Chicago, and New York offer walk-in testing with trauma-informed staff. But access is uneven. In rural areas or southern states, finding a nonjudgmental provider can feel impossible.
That’s where at-home testing becomes not just a tool, but a survival strategy. For those in controlling families, religious environments, or closeted relationships, being able to test discreetly can literally change lives. A kit left in your sock drawer. A sample dropped off at a quiet postbox. Peace of mind doesn’t have to be public.
And that’s the point: care should never require shame.
Queer Mythologies: What We Still Get Wrong About STD Risk
For all our memes, mutual aid, and queer literacy, we’re still battling dangerous misconceptions, often passed down from clinics that erased us or health classes that never included us. These myths don’t just confuse, they delay care, silence symptoms, and perpetuate stigma.
Myth one? “Lesbians don’t get STDs.” False. Herpes, HPV, trichomoniasis, and even gonorrhea can be passed through vulva-to-vulva contact, shared sex toys, or oral sex. But because providers and educational systems ignored queer sex, many women who love women simply weren’t told the risks, or the need for screening.
Myth two? “If there are no symptoms, you’re fine.” Also false. The CDC estimates that up to 80% of chlamydia cases in women and 50% in men are asymptomatic. The same goes for other STDs. No burning doesn’t mean no bacteria. And for those who do notice changes, like an unusual discharge, sore throat, or rash after sex, it’s easy to second guess. Was it the lube? The razor? A heat rash? Denial becomes a coping mechanism.
Myth three? “If you’re careful, you won’t get anything.” But STDs aren’t a punishment for being careless. They’re a biological possibility of being human, of sharing bodies. We need to move away from this idea that infection equals irresponsibility. You can wear condoms. You can test regularly. And still get something. That doesn’t make you bad. It makes you alive.
“I Should’ve Tested Sooner”: What Regret Sounds Like at 2AM
There’s a specific kind of silence that hits after a hookup, when something feels...off. Maybe it’s an itch. Maybe a bump. Maybe it’s nothing. But your brain won’t shut up. You tell yourself not to panic. You scroll forums. You compare photos you shouldn’t be comparing. And still, the worry doesn’t fade.
This is the moment many of us realize we’ve been avoiding the test. Not because we’re unaware. But because we’re afraid of what it might mean. Will it change how we see ourselves? Will it confirm some deep fear that we’re flawed, unworthy, broken?
These fears are powerful. But they’re also solvable. The truth is, most STDs are treatable. Some clear up on their own. Others require a quick round of antibiotics. Even HIV, once a death sentence, is now a manageable condition, with medication, someone living with HIV can live a long, healthy, and fully sexual life.
So what do we do in that 2AM spiral? We give ourselves permission to know. To test. To find out, not to punish, but to plan. Because even the worst-case scenario is easier than the endless loop of “what if.”

People are aslo reading: You’re on PrEP. Do You Still Need to Worry About STDs?
Testing as a Love Language: From Panic to Partnership
Testing doesn’t have to be scary. It doesn’t even have to be solo. For queer couples, polycules, or casual partners, testing together can become a ritual of trust. It says: I care about your health. I want us to feel safe. Let’s be real together.
That’s why many people now use at-home kits not just after a scare, but before new connections. A swab shared before sex. A test swapped during a movie night. It becomes part of the language of intimacy, like condoms, like lube, like check-ins about boundaries and pain and pleasure.
And for those who prefer privacy, kits like the Combo STD Test Kit offer an accessible, judgment-free way to reclaim your autonomy. You don’t need to perform for a nurse. You don’t need to answer invasive questions. You just follow the instructions, send the sample (if mail-in), or read the results in minutes (if rapid), and decide your next step, with support, not shame.
Whether you're worried about a new sore or just ready for peace of mind, testing is care. It’s community. It’s an act of radical self-trust.
Finding Safety When You’ve Been Hurt by the System
For many LGBTQ+ folks, especially those with histories of assault, clinic trauma, or family rejection, even thinking about STD testing can be triggering. It’s not “just a swab.” It’s a reminder of past violations. Of being told your body is wrong. Of being silenced.
That’s why trauma-informed care matters. It's why providers need training. Intake forms need options. Rooms need privacy. And it’s why queer-led spaces, both physical and digital, are lifelines. Communities that say: “We believe you. You deserve care. You don’t have to prove anything to be worth protecting.”
If a clinic harmed you, you’re not alone. If a provider dismissed your symptoms or misgendered you during an exam, that wasn’t your fault. And you still deserve to feel safe. Sometimes that safety starts at home, with a test kit and a moment of control. Sometimes it starts by telling a friend, “I think I need to test, but I’m scared.” That’s care too.
Care doesn’t have to be clinical. Sometimes, it just needs to be honest.
Before You Panic, Here’s What to Do Next
STDs are not a moral failure. They’re not proof of being reckless, dirty, or broken. They’re part of being human, and they’re manageable. What matters is knowing, not guessing. Acting, not spiraling.
You don’t need to do it alone. You don’t need to announce it to the world. But you do deserve clarity. And you can get it, on your terms, in your time, from the safety of your space.
If something feels off, or even if it doesn’t but you haven’t tested in a while, take that step. This at-home combo test kit checks for the most common STDs discreetly, quickly, and without judgment. Because your health shouldn’t have to wait for your courage to catch up.
FAQs
1. Can I really get an STD even if I used protection?
Yep. Protection helps , a lot , but it’s not a magic force field. Condoms and dental dams reduce risk, but infections like herpes and HPV can spread through skin contact outside those barriers. Think of them as great tools, not guarantees. That’s why testing still matters, even when you do everything “right.”
2. Do lesbians and queer women really need to worry about STDs?
100%. We’ve been left out of sex ed for too long, but the risk is real. Infections like trichomoniasis, HPV, and herpes can pass through oral sex, shared toys, or even fingering , especially if there are cuts or sores involved. Bottom line: queer sex deserves real protection and real care, too.
3. How do I get tested without being outed or judged?
Start at home. Literally. At-home STD test kits let you screen in your own space, on your own schedule. No awkward waiting rooms, no nosy nurses. Just you, a test, and the truth , safely yours.
4. What if I test positive?
First, take a deep breath. Seriously. A positive result doesn’t mean you did something wrong. It means you now have information , and options. Most STDs are treatable. Many are temporary. And if it’s something chronic like herpes or HIV, there are amazing meds that make life just as full and sexy as before.
5. Will people still want to date me if I’ve had an STD?
The right ones will. Plenty of people have had STDs , most just don’t talk about it. Disclosure can feel terrifying, but it also weeds out people who aren’t safe or mature enough to deserve your trust. And hey, there are whole dating communities for people living with herpes, HIV, or other diagnoses. You’re not alone , you’re experienced.
6. Do I need to test if I feel fine?
Yes. Many STDs , especially chlamydia, gonorrhea, and even syphilis , can hang out with zero symptoms. You could feel totally normal and still pass something on. Testing isn’t about reacting to a scare. It’s about keeping tabs on your body like you would your teeth or your blood pressure.
7. How often should I test?
If you’re having sex with new or multiple partners, every 3 to 6 months is a solid rhythm. If you’re monogamous or not active right now, once a year is still a good health habit. Think of it like changing your oil , don’t wait until something breaks.
8. Are at-home test kits really legit?
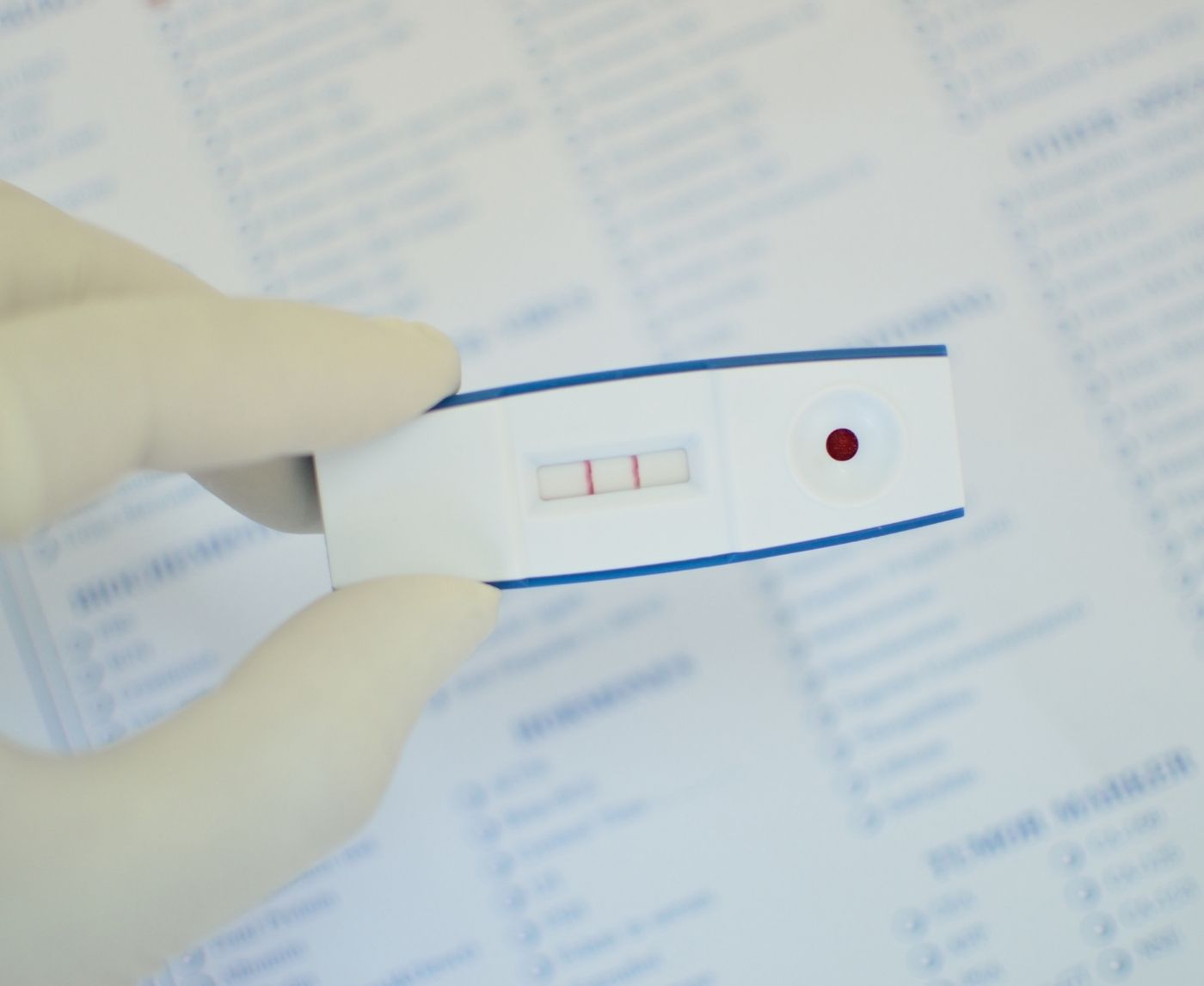
They are if you buy from a reputable source. Brands like STD Rapid Test Kits use the same science labs and test types as clinics. You’ll get reliable results without leaving your bedroom , which, let’s be honest, is where most of the questions start anyway.
9. What if I’m scared to even look at the results?
Totally normal. Waiting can feel worse than knowing. But remember: knowing gives you power. Whether it’s a clear negative or a “hey, let’s deal with this,” it’s yours to own , and you don’t have to do it alone. Text a friend. Journal your panic. Then check. Courage isn’t the absence of fear; it’s checking anyway.
10. I’m trans. Do I really need to go through dysphoric testing?
You shouldn’t have to. If traditional clinics feel unsafe or invalidating, at-home kits let you take samples on your terms, in your body, with your language. You’re allowed to protect both your physical health and your mental well-being. Testing can feel gender-affirming when you do it your way.
You Deserve Answers, Not Assumptions
You’ve been told a lot of things about STDs , that they’re shameful, that they only happen to “those kinds of people,” that silence is safer than truth. But here’s what you haven’t been told enough: you deserve clarity. You deserve tools. You deserve care that meets you where you are , not where someone thinks you should be.
Infections don’t make you less queer, less clean, or less worthy of love. They just make you someone with a body , a body that’s living, touching, craving, healing. And knowing what’s going on with that body? That’s not gross. That’s powerful.
If you’ve been putting off testing because of fear, judgment, or trauma, you’re not alone. And you’re not out of options. This at-home combo test kit can be your first step , quiet, simple, and entirely yours. No assumptions. Just answers.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. HIV.gov – U=U and Living with HIV
2. STIs & How to Prevent Them | CDC
3. Attitudes and Perceived Barriers to Sexually Transmitted Infection Testing Among U.S. Adults
4. Relationships Between Perceived STD‑Related Stigma and STD Testing Among Young Adults
5. Barriers to HIV Testing: Patient and Provider Perspectives in Primary Health Clinics
6. Exploring Facilitators and Barriers to STI/HIV Self‑Testing Among College Students
7. Differences in Healthcare Access, Use, and Experiences Among LGBTQ and Non‑LGBTQ Adults
8. Cisnormativity as a Structural Barrier to STI Testing for Trans and Gender‑Diverse People
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: M. Kelsey, MPH | Last medically reviewed: November 2025
This article is for information only and should not be used as medical advice.