When the STD Test Says “Negative” But Your Body Says “Something’s Wrong”
Quick Answer: Chlamydia can cause irreversible reproductive damage before any symptoms show up. Regular testing is essential, even if you feel completely fine.
Why This Story Is More Common Than You Think
Natalie’s case isn’t rare. According to the Centers for Disease Control and Prevention (CDC), chlamydia is the most frequently reported bacterial STD in the U.S. And yet, more than 70% of women and about half of men who contract it never experience noticeable symptoms. That’s why it’s often called a “silent” infection, and why it slips through the cracks of normal life.
Imagine you just started dating someone new. You used a condom the first few times but stopped once things felt serious. There’s trust. Maybe even exclusivity. So you don’t think about testing. And if you’re not itching, leaking, or burning, why would you?
This is exactly how it hides. Not in plain sight, but in our assumptions. And the longer chlamydia goes undetected, the higher the risk of pelvic inflammatory disease (PID), chronic pelvic pain, and infertility. For people with uteruses, the consequences can be permanent. For people without, they often remain asymptomatic carriers, passing it unknowingly from one partner to the next.
What Chlamydia Feels Like, When You Feel Anything At All
While many cases are silent, the symptoms that do appear can be subtle or easy to misread. Take Ana, 23, who thought her unusual spotting was due to switching birth control pills. She also noticed it hurt a little to pee, but it wasn’t a full-on UTI burn, more like a vague irritation that came and went. “I thought I was being paranoid,” she said. “It wasn’t until my boyfriend had discharge that I even considered testing.” Both tested positive.
What’s maddening is how often chlamydia mimics other things: hormonal changes, yeast infections, minor bladder irritation. It rarely announces itself clearly. That’s why testing, not symptoms, is the only reliable way to know.
Table 1. How chlamydia symptoms often get misread, especially early on.

People are also reading: The Numbers Don’t Lie Why Non-Sex Workers Often Have Higher Undiagnosed STD Rates
The Clock Starts Before You Even Know It
One of the most dangerous things about chlamydia is how early the damage can begin, even when you feel normal. Infections can travel from the cervix to the uterus and fallopian tubes over time, leading to scarring that blocks fertilization. This can happen quietly, especially if someone isn’t testing regularly.
By the time pain appears, it’s often a sign that inflammation has already progressed. A study published in the journal Sexually Transmitted Diseases found that nearly 25% of women who experienced tubal infertility had previously undiagnosed chlamydia infections.
And it’s not just about future kids. PID caused by chlamydia can lead to chronic pelvic pain, ectopic pregnancy (which can be life-threatening), and emotional fallout that lingers long after the physical symptoms subside. As one Reddit user put it: “The scariest part wasn’t the diagnosis, it was realizing how long it had been there without me knowing.”
Can You Really Get Chlamydia Without Cheating?
This question comes up more than most people expect, especially in long-term relationships. And the answer is yes, with a heavy asterisk. Chlamydia doesn’t appear spontaneously, but it can go undetected for months or even years, resurfacing long after the initial infection. That means someone may have contracted it before a relationship began, never showed symptoms, and only passed it on later.
Case in point: Malik, 31, tested positive for chlamydia after experiencing pain during ejaculation. He immediately suspected his girlfriend of cheating. But she’d never had symptoms, and she tested positive too. “We almost broke up over it,” he said. “But her OB explained that it could’ve been dormant in either of us.” Retroactive blame only made the emotional toll worse.
This is why retesting, even in trusted relationships, is a form of self-care, not suspicion. STDs aren’t a moral verdict. They’re bacteria and viruses, not betrayals. But because chlamydia can stay asymptomatic for so long, it has the power to break trust if people assume symptoms always appear when something’s wrong.
That’s why organizations like Planned Parenthood recommend yearly chlamydia testing for all sexually active people under 25 and for older adults with new or multiple partners. If you’re in a monogamous relationship, testing can still be worth it, especially before you stop using condoms or start trying to conceive.
Why “I Got Tested” Doesn’t Always Mean “I’m Clear”
Here’s the confusing truth: not all STD tests screen for everything, and not all timing is accurate. Chlamydia has a window period of roughly 7 to 14 days after exposure, meaning a test taken too early may come back negative even if you’re infected.
Consider the experience of Jordan, 26, who tested negative two days after a condom broke with a casual partner. “I thought I was being responsible,” he said. “But then my ex texted me two weeks later saying I gave her something.” Turns out, his test was too early. A repeat swab later confirmed a chlamydia infection.
Understanding how chlamydia tests work, and when they work best, can prevent false reassurance. Most home or clinic-based chlamydia tests use a highly sensitive method called NAAT (nucleic acid amplification test), which detects the bacteria’s genetic material. But even the best test can’t outsmart timing.
Table 2. Chlamydia test windows and accuracy by method.
It's no wonder so many people test, feel “clear,” and still end up spreading the infection. That’s why follow-up testing is sometimes necessary, especially after new exposures, condom failures, or early testing. It’s not about paranoia. It’s about precision.
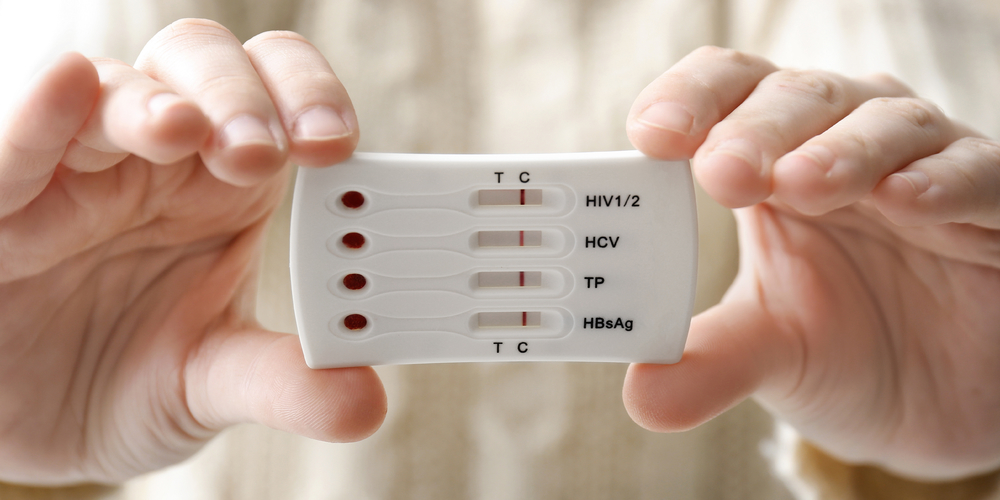
If you’re unsure when you were exposed or if your symptoms keep shifting, a combo test kit can help identify multiple infections at once, and retesting after 2–3 weeks can confirm early results.
What Happens If You Don’t Catch It in Time?
The danger of untreated chlamydia lies in its slow creep. What starts as a simple bacterial infection can turn into pelvic inflammatory disease (PID), which causes inflammation, scarring, and permanent damage in reproductive organs. The fallopian tubes, in particular, are vulnerable, once scarred, they can block eggs from reaching the uterus or increase the risk of ectopic pregnancy.
One study published in BMJ Open found that up to 30% of women with untreated chlamydia may go on to develop PID. And here’s the worst part: many don’t realize it until years later, when they’re trying to conceive and face unexplained infertility.
Long-term complications aren’t limited to those with uteruses. Men can develop epididymitis, painful inflammation near the testicles, that, in rare cases, can affect fertility. Chlamydia can also increase the risk of acquiring or transmitting HIV.
“I thought it was no big deal,” said one user in a support forum, describing their untreated chlamydia that led to PID. “I kept waiting for symptoms. They never came, just years of invisible damage.”
This is why testing isn't just about the present. It's about protecting your future body, your future self.
Can Chlamydia Come Back After Treatment?
Short answer? Yes, but it’s not that the antibiotics failed. Chlamydia reinfection is common, especially if your partner wasn’t treated at the same time. The CDC reports that up to 20% of people treated for chlamydia will get it again within a few months, not because the meds didn’t work, but because someone in their network didn’t follow through.
Let’s rewind to Megan, 24, who took her antibiotics exactly as prescribed. She felt fine afterward and assumed everything was handled. Her boyfriend, on the other hand, delayed treatment and never got retested. They resumed sex a week later. Within two months, she was positive again, this time with more intense symptoms.
Retesting after three months is now a standard recommendation for anyone who’s been treated for chlamydia. It’s not about blaming your partner, it’s about making sure the infection hasn’t circled back. It can happen even in monogamous couples, especially if one person delayed treatment or got exposed again elsewhere.
Not sure if you need to test again? If you were treated recently, changed partners, or have symptoms reappear, STD Rapid Test Kits offers discreet, at-home testing to keep things on your own timeline. You’re not being “extra”, you’re protecting your body.
How to Talk to Partners Without Shame or Panic
This part trips up nearly everyone. Whether you tested positive, suspect exposure, or just want to get tested together, the conversation can feel heavy. But it doesn’t have to be. Think of it like a seatbelt, it’s about prevention, not prediction.
Brent, 30, said he was terrified to tell his girlfriend he’d tested positive for chlamydia, fearing she’d assume he cheated. But when he told her calmly, explained he’d had no symptoms, and offered to get tested together again, she softened. “She actually thanked me for being upfront. We both tested, both treated. It turned into trust instead of a fight.”
Scripts help. So do facts. Saying, “I just found out I had a silent STD that often shows no symptoms” is a very different conversation than “I gave you something.” Framing matters. Testing together can be a gesture of care, not confession.
There are also anonymous notification tools and telehealth support lines that help reduce the emotional burden. You don’t have to go through it alone, and you don’t have to sound like a textbook. You just have to start.

People are also reading: What No One Tells You About Cleaning Sex Toys (and Why It Matters)
How Privacy and Timing Work With At-Home Kits
Waiting in a clinic lobby when you’re panicked about STD symptoms is a specific kind of stress. So is trying to explain your last sexual encounter to a stranger in scrubs. That’s why at-home testing exists, not as a shortcut, but as an option for people who value privacy and convenience.
Shipping is usually discreet, arriving in nondescript packaging. Some kits come with prepaid return mailers; others give you results within 15–30 minutes, depending on the format. Most use a urine sample or vaginal swab, with instructions you can follow at home. And yes, they’re real tests. Many are FDA-cleared and use the same tech as lab-based options.
The key is reading instructions carefully, timing your test based on last exposure, and following up if anything’s unclear. If you're testing because of symptoms or a known exposure, testing 7 to 14 days post-exposure gives the most reliable results.
Need a place to start? The Combo STD Home Test Kit checks for multiple infections, so you’re not just treating what you suspect, you’re ruling out what you can’t see.
What Happens After a Positive Result?
First, take a breath. Seriously. A positive chlamydia result can feel like a punch to the gut, but it’s one of the most treatable STDs. A single round of antibiotics (usually azithromycin or doxycycline) clears the infection in most cases. The hardest part is often emotional, not medical.
If you tested using a rapid kit, follow up with a confirmatory NAAT test at a clinic or through a mail-in lab. If you tested through a lab, your results are already high-accuracy. From there, notify partners, abstain from sex for seven days after treatment (or until symptoms resolve), and plan for a follow-up test in about three months.
“I sat in my car staring at the result,” said one reader. “I felt gross. But then I told myself, this is just information. Now I know. Now I can act.”
You’re not alone. Millions go through this, and many never even tell anyone. But you deserve support, and a clear next step.
FAQs
1. Can chlamydia really cause damage even if I feel totally fine?
Yes, and that’s the scary part, it’s like a leak behind your walls. You might not see it, but the damage can build. Chlamydia can quietly lead to pelvic scarring, fertility issues, and chronic pain without making a scene first. That’s why “no symptoms” doesn’t mean “no problem.”
2. How did I get chlamydia if I didn’t cheat, and neither did my partner?
One word: timing. Either of you could’ve had it before the relationship started and not known it. It can sit in the body quietly, sometimes for months, and get passed on later. It’s not always a sign of betrayal, it’s often just bad luck and missed timing.
3. Is it true you can get chlamydia from oral sex?
Totally true. It’s less common than other routes, but oral-to-genital transmission happens. You could even have it in your throat and never know. No joke, this is one reason condoms and dental dams during oral aren’t just for show.
4. Does a negative test mean I’m in the clear?
Only if the timing is right. Testing the day after a hookup? Too early. Chlamydia needs a window, usually 7 to 14 days after exposure, to show up on tests. A negative before then might give false confidence. If in doubt, test again later.
5. Will I definitely have symptoms if I get it?
Nope. Most people don’t. And the symptoms that do show up can be confusing, spotting, slight burning, or maybe just feeling “off.” It’s like trying to guess if you’ve got a cold or allergies, symptoms aren’t a guarantee, and many go unnoticed.
6. Can I treat chlamydia at home without seeing a doctor?
You can start at home with a test, yes, but treatment still requires a prescription. The go-to is antibiotics like doxycycline. The good news? Many telehealth services will prescribe meds once your test result is confirmed. No in-person awkwardness required.
7. What if I got treated, can I still get it again?
Definitely. Chlamydia doesn’t create immunity. If your partner wasn’t treated, or if you hook up with someone new who has it, you can get reinfected. That’s why retesting after a few months is part of the standard game plan.
8. Should I tell my exes I tested positive?
It’s not easy, but yeah, it’s the right thing to do. You don’t have to give a TED Talk. Just a heads-up so they can test too. Some clinics offer anonymous partner notification if that makes it easier.
9. Do home chlamydia tests actually work?
When used correctly and timed right, yes. Many use the same NAAT technology as labs. The key is following the instructions, collecting your sample carefully, and not testing too early. If you can handle a rapid COVID test, you’ve got this.
10. Can untreated chlamydia really make it harder to get pregnant?
Unfortunately, yes. That’s the part no one talks about enough. Silent infections can scar the fallopian tubes or cause PID, making conception harder down the line. It’s not meant to scare you, but it is meant to get your attention. Testing early changes everything.
You Deserve Answers, Not Assumptions
It's easy to ignore a mild symptom, believe that one early test, or think that you're "not the type" to get an STD. Chlamydia, on the other hand, doesn't care who you are or what you wanted to do. It spreads slowly, waits patiently, and doesn't always show up the way you think it will.
Testing is more than just a way to stop something; it's also a way to give people power. Getting tested gives you control over your health and peace of mind, whether you have symptoms or not.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. Planned Parenthood – Chlamydia Overview
2. American Sexual Health Association – Chlamydia
3. Mayo Clinic – Chlamydia Overview
4. NHS – Chlamydia Symptoms and Treatment
5. WHO – Sexually Transmitted Infections Fact Sheet
7. Chlamydia‑associated reproductive complications in women — Australian Journal of General Practice
8. Chlamydia trachomatis: From Urogenital Infections to the Development of Infertility — MDPI Genes
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Kara Stinson, NP | Last medically reviewed: November 2025
This article is for informational purposes and does not replace medical advice.