Ashamed to Ask Your Doctor About STDs? There’s Another Way
Quick Answer: STD testing doesn't have to be awkward or confusing. Understanding timing, test types, and your rights to privacy can make a huge difference in how your first (or next) test feels.
1. Timing Matters More Than I Realized
The first time I got tested, it was four days after a hookup that scared me. I felt like I was doing the responsible thing. But no one told me that many STDs don’t show up right away, and that testing too early can give you a false negative. According to the CDC, infections like chlamydia and gonorrhea can take up to 7–14 days to show up in tests. For HIV, it can take even longer depending on the type of test.
Knowing the right window periods would have saved me a lot of confusion. Now I wait at least two weeks after a possible exposure, unless I have symptoms earlier. Even then, I retest later to be sure.
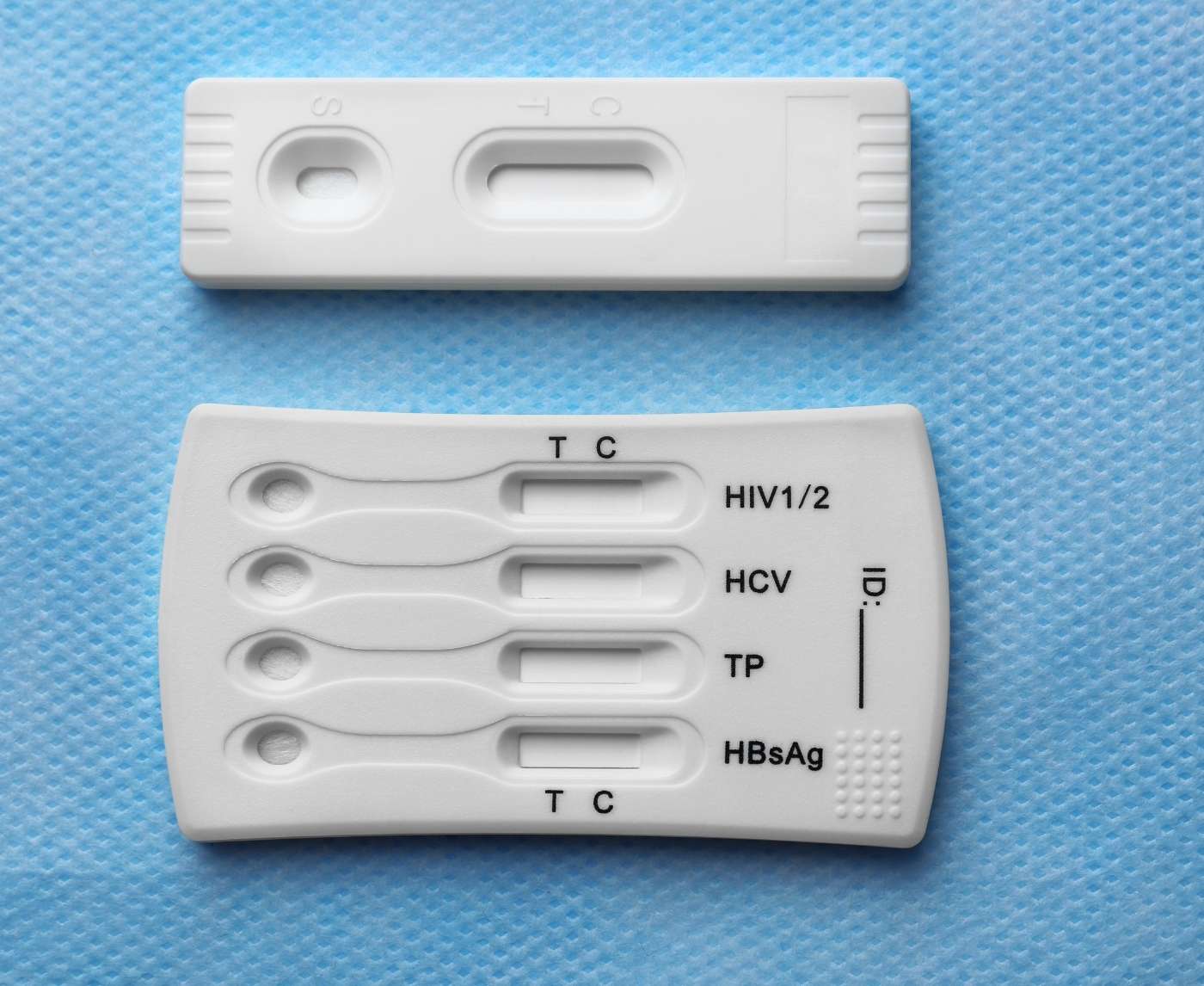
Figure 1. Window periods for common STDs. Testing too soon may not detect the infection yet, even if you're already exposed.
2. Not All STD Tests Are the Same
I assumed they were testing me for everything. They weren’t. Most clinics only run tests based on what you request, or what you admit to doing. I didn’t know that. I was too embarrassed to mention oral sex, so they didn’t test my throat. I didn’t know herpes isn’t part of a standard panel unless you ask.
Now I use the 6‑in‑1 At‑Home STD Test Kit to check for the big five: chlamydia, gonorrhea, syphilis, HIV, and trichomoniasis. It covers the most common infections and gives results from home, no awkward conversations, no judgment.

People are also reading: When Pink Eye Is Actually an STD: What to Look For
3. Clinics Can Be Overwhelming (and That's Not Your Fault)
I thought I was overreacting, but I wasn’t. The clinic waiting room had a sliding glass window that slammed shut after I signed in. The form asked if I’d ever traded sex for drugs or money. The nurse was polite but clearly rushing. It felt more like a transaction than care. I left feeling small.
That experience almost made me never test again. And that’s a huge problem. A single negative experience can delay care, increase risk, and compound shame. If your first test feels like a failure, that’s not your fault. You’re still doing the right thing by getting tested, just maybe in a different way next time.
If you want a more private and supportive option, STD Test Kits offers tests you can do at home, at your own pace.
4. At-Home Testing Changed Everything for Me
The second time I got tested, I didn’t go to a clinic. I used a discreet at-home kit. No one asking invasive questions. No cold exam table. No paperwork about whether I was "high risk."
Just me, a test cassette, and a simple set of instructions. I took the sample myself, followed the timing guide, and had results in minutes. It wasn’t just easier. It felt like healing. It felt like taking control.
Figure 2. Comparing STD test methods. Home kits offer privacy and simplicity, especially for repeat testers or trauma-informed care needs.
5. It's Okay to Cry, Panic, or Go Numb
No one prepared me for the emotional whiplash. I went in for my initial STD test thinking that I would leave with my head held high. But I felt exposed. It wasn't the test, it was everything that went with it. The fear, the shame, the silence.
If this is your first time, and you’re feeling overwhelmed? That’s not weakness. That’s humanity. These are high-stakes tests. They involve your body, your relationships, your identity. It’s normal to feel big emotions. Just don’t let those emotions stop you from getting the answers you deserve.
6. You Have a Right to Privacy, Even in a Clinic
I used to think I had to answer every question during a clinic STD test. I didn’t realize I could say, “I’m not comfortable sharing that,” or ask what a test was for before agreeing to it. No one told me I could decline an internal exam. No one told me I didn’t have to give my full name at some clinics.
There are laws, like HIPAA in the U.S., that protect your health privacy. And in many cities, you can access free or low-cost testing without using your insurance or real name. But when you don’t know your rights, it’s easy to feel powerless. That’s why I now choose testing options where I feel in control from the beginning, especially at home.
7. Symptoms or No Symptoms, You Still Might Be Positive
I waited until I noticed itching and discharge to get tested. What I didn’t realize is that many STDs don’t show symptoms at all, especially in the early stages. According to the Planned Parenthood guide on STI testing, infections like chlamydia and gonorrhea can be completely silent and still cause long-term damage if untreated.
I also learned that sometimes symptoms have nothing to do with STDs, yeast infections, UTIs, allergic reactions, even anxiety can mimic similar signs. That’s why testing isn’t about waiting until something is “obvious.” It’s about getting peace of mind before things get complicated.
8. You Don’t Have to Tell Anyone (But You Can)
The first time, I told no one I was getting tested. I felt like it was this shameful thing I had to do alone. But the second time, I told a friend. And suddenly, the weight lifted. She had stories of her own. She even recommended the at-home kit I ended up using.
You don’t owe anyone your story, but you also don’t have to carry it alone. If you’ve had a hard first test, consider sharing it with someone safe. It might make your next test feel a little lighter. It did for me.
And if you want to make sure your partner is on the same page, you can even test together. Ordering two kits can make the experience feel shared, not secretive. 8‑in‑1 Complete At-Home STD Test Kit is easy to use for both partners, no awkward conversations at the clinic required.

People are also reading: What Does HPV Look Like in Men? (Sometimes, Nothing at All)
9. Knowing What Happens Next Makes It Easier
No one explained how results would be delivered during my first test. I didn’t know how long it would take, what “positive” even meant, or whether I’d need treatment. The unknown was scarier than any infection.
Now I ask every time: When will I get my results? What happens if I test positive? Is treatment available here, or do I need to go somewhere else? With at-home tests, I have the instructions in my hand, the timing is clear, and if I need treatment, I already have a plan in place. That peace of mind makes a huge difference.
One of the biggest things I wish I’d known? That testing is just the first step. If the result is positive, it doesn’t mean panic, it means a plan. Most STDs are treatable. And all of them are manageable once you know.
10. You Deserve to Feel Safe While Testing
I didn’t feel safe my first time. I didn’t feel seen. But I want you to know something I learned the hard way: testing should feel like care, not punishment.
You deserve a space that respects your body, your story, and your boundaries. That might be a great clinic. That might be your bedroom with a rapid test and a cup of tea. Either way, it’s your choice. Your health, your rules.
Whether you're testing after a risky encounter, starting a new relationship, or just checking in on your body, you're doing something brave. And you deserve every bit of safety and clarity that comes with it.
“I Almost Never Got Tested Again”
Andre, 27, went for his first STD test at a busy walk-in clinic after a condom broke during a hookup. He says the staff barely looked at him, rushed through the intake, and never told him what they were testing for. He left feeling more judged than helped, and never received his results.
“I just figured if I didn’t hear anything, I was fine. But the anxiety didn’t go away. I kept Googling things, second-guessing myself, having dreams about getting sick.”
Two months later, Andre ordered an at-home test after his partner encouraged him. This time, he followed every step, saw the result himself, and felt the difference.
“It felt like something I was doing for me, not something being done to me.”
His test was negative. But more importantly, it gave him back a sense of control. And now, he says he tests regularly, with less fear and more clarity.
FAQs
1. Do I really need to get tested if I don’t have symptoms?
Yes, 100 times yes. Most STDs don’t throw up obvious red flags. You could be carrying chlamydia or gonorrhea without a single itch, drip, or bump. Testing isn’t about panic, it’s about peace of mind, even when everything seems quiet.
2. How soon is too soon to test after sex?
Depends on what you're testing for. A quick hookup last night? Probably too early. Most infections need at least a week to show up on tests. Two weeks is better. Some (like HIV) take even longer depending on the test type. The golden rule: test once at the 2-week mark, then again later if symptoms show or for full peace of mind.
3. Does it hurt?
Let’s be real: no one’s thrilled about swabs or finger pricks. But “hurt” might be a strong word. Most STD tests are more annoying than painful. Pee in a cup? Easy. Fingerstick? A moment of pinch. Swabs? Slightly uncomfortable, but over fast. Bonus: many at-home tests skip the invasive stuff altogether.
4. Will I get tested for everything automatically?
Not unless you ask. Here's the tricky part, many clinics only test for what you request. Herpes? Not usually included. Oral or rectal swabs? Only if you say you need them. That’s why knowing your exposure, and speaking up, is half the battle.
5. What if I’m too embarrassed to talk to someone about testing?
You’re not the only one. That’s exactly why at-home kits exist. You don’t need to justify your sex life to anyone. Order a test online, do it in your own space, and skip the awkward eye contact altogether. Testing should feel like self-care, not an interrogation.
6. Can I just wait and see if symptoms show up?
You could, but it's risky. Some STDs can hang out quietly and do damage behind the scenes. Others mimic common stuff like yeast infections or UTIs. If you're relying on symptoms alone, you're basically gambling. And not the fun Vegas kind.
7. What if my result is positive?
Deep breath. Positive doesn’t mean doomed, it means you have information. Most STDs are treatable. All of them are manageable. You'll get through it. Call a clinic, follow the care steps, tell your partner(s) if needed, and move forward. You’re still you, just more informed.
8. Can I take the test and keep it private?
Absolutely. Whether you’re 19 and still on your parents' insurance or 42 and just don't want your business out there, privacy is your right. Most at-home kits don’t report to insurance. The package is discreet. The results are yours, period.
9. How often should I be getting tested?
Depends on your sex life, not your relationship status. New partner? Casual hookups? Open relationship? Every 3–6 months is smart. In a long-term monogamous situation? Once a year is a good baseline. If something feels off, test sooner. No shame either way.
10. What happens if I mess up the test at home?
Don’t panic. Most kits are pretty foolproof, but if you miss a step (we’ve all skimmed instructions), just retest. If you're unsure about the result, or it looks weird, faint, or broken, go with your gut and do another test. Better to double-check than sit in uncertainty.
Before You Panic, Here’s What to Do Next
Your initial STD test doesn't have to dictate your health experience. Whatever it was -- awkward, hurtful, confusing, or just plain awful -- it doesn't have be that way next time. You do have control over making it better.
Begin with a practice that honors your anonymity, puts your comfort first, and gives you immediate and clear responses. You have the right to feel cared for and comfortable in the process.
Don't hesitate and ponder, have the clarity that's yours due.
How We Sourced This Article: We combined lived-experience reports, peer-reviewed studies, and medical guidelines from trusted organizations like the CDC and Planned Parenthood to make this guide honest and practical. Around fifteen sources informed our writing; below, we’ve highlighted six of the most useful and reader-focused ones.
Sources
1. CDC – 2021 Sexually Transmitted Infections Treatment Guidelines
2. STD Testing: What’s Right for You? | Mayo Clinic
3. How Do I Talk With My Partner About STD Testing? | Planned Parenthood
4. How STD Testing Works | Planned Parenthood
5. Getting Tested for STIs | CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Jenna L. Ortiz, NP | Last medically reviewed: September 2025
This article is for informational purposes and does not replace medical advice.