Think You Have HIV? Why Testing Too Early Can Backfire
Quick Answer: Syphilis spreads in 2026 because symptoms are easy to miss, testing is often delayed, and reinfection is common, even after treatment. PAHO’s new elimination agreement aims to close these gaps across the Americas.
“I Thought It Was Razor Burn”, How Syphilis Gets Missed
“I didn’t even think about syphilis. I just thought I’d nicked myself shaving,” said Carlos, 27, a bisexual man in rural Florida. By the time he got tested, the painless ulcer near his groin had disappeared, and so had his opportunity to stop the spread early.
Primary syphilis often presents as a single, painless sore or ulcer on or near the genitals, mouth, or anus. For many people, especially those without regular access to sexual health care, this sign goes unnoticed or gets misdiagnosed as something minor like an ingrown hair, heat rash, or a pimple. By the time secondary symptoms emerge, rashes, mucous patches, or flu-like symptoms, the infection has already progressed.
According to the CDC, syphilis infections rose dramatically in the last decade, with congenital syphilis (passed during pregnancy) increasing nearly 10-fold in some areas. But the bigger problem isn’t just rising numbers, it’s that the symptoms are sneaky, and the silence is dangerous.

People are also reading: Can You Get HPV From a One-Night Stand? The Answer’s Complicated
The Reinfection Loop: Yes, You Can Get Syphilis Again
One of the biggest myths about syphilis is that once you’ve had it, and taken antibiotics, you’re immune. You’re not. You can get syphilis again and again, even within the same year. In fact, the PAHO report on the new elimination agreement specifically addresses reinfection as a core challenge to stopping transmission in the Americas.
Reinfection is especially common in groups where testing isn't routine or partner notification is difficult. This includes LGBTQ+ communities, people without stable housing, sex workers, and those in countries where healthcare access is limited or stigmatized. When testing isn’t easy, and conversations about exposure are taboo, the same infections keep bouncing around unchecked.
“I got treated once, then again six months later. Different guy, different weekend, same result,” said Jasmine, 32, a Black queer woman in Atlanta. “Now I test every three months. It’s just part of my routine.”
Why a Cure Isn’t Enough: The PAHO Elimination Agreement
In November 2023, the Pan American Health Organization (PAHO) announced a new regional agreement that 35 countries signed to get rid of syphilis in the Americas. The plan stresses that everyone should be able to get tested, that pregnant women should be screened, and that more people should be able to get treatment.
It looks like a huge win on paper. But campaigns to get rid of syphilis often focus on pregnant women and babies, where the disease can cause miscarriage, stillbirth, or lifelong disability. They don't do a good job of explaining how reinfection, stigma, and gaps in testing keep the disease going in adults.
While congenital syphilis prevention is a crucial step, experts warn that focusing only on maternal cases can miss the broader community spread. “You can’t treat a baby without treating their parents and partners,” said Dr. Leanne Gutiérrez, a sexual health physician based in Bogotá.
In that sense, the PAHO agreement is a start. But elimination will only succeed if everyday people can access rapid, confidential testing, especially those who don’t feel safe walking into a clinic.
Why Syphilis Still Spreads Despite Being Curable
Figure 1. Key reasons syphilis continues to spread even with effective cures available. Solutions must address both clinical and emotional barriers to testing.
When Timing Betrays You: The Window Period Problem
Many people rush to test right after a risky encounter. Sometimes, it is the very next day. But this can backfire: Most syphilis tests won't detect infection until at least 2-3 weeks after exposure. This window period is the time between infection and when a test can reliably pick it up. Testing too early can lead to false negatives, making someone think they are in the clear when they are not.
“I tested three days after the hookup. It came back negative, so I thought I was fine,” said Dominic, 29, a musician in Mexico City. “Then the rash showed up a week later, and I tested again, positive.”
According to research published in the Journal of Infectious Diseases, treponemal antibody tests used to detect syphilis usually become reactive around 14 to 21 days post-exposure. Retesting is often required when early results are negative but suspicion remains high. That’s especially important for people in ongoing high-risk networks or relationships with multiple partners.
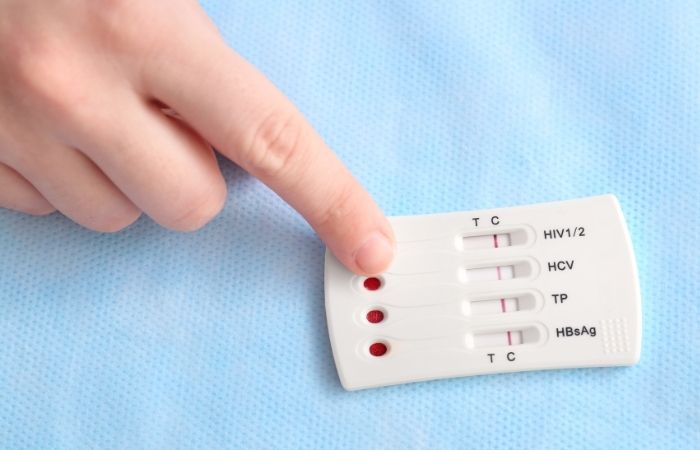
The Rise of At-Home Syphilis Tests (And Why They Matter)
In places where STI clinics are scarce, or where walking into one feels unsafe, at-home testing is changing the game. Rapid syphilis tests, using a small blood sample from a fingerstick, can provide results in minutes. These tests aren’t perfect, but they close an important gap for people who might otherwise go undiagnosed for months.
You can now order a Syphilis Rapid Test Kit here, test yourself discreetly, and follow up with a doctor if needed. The privacy, speed, and autonomy are part of what makes these tools so essential to breaking the transmission chain. They don’t require insurance. They don’t require awkward conversations at the pharmacy counter.
“If I had to wait for an appointment at the free clinic, I probably wouldn’t have gone,” said Angela, 35, who lives in a remote area of Brazil. “But I could test at home, and I caught it before I gave it to anyone else.”
While at-home tests have slightly lower sensitivity than lab-based options, they are more accessible and often better than no test at all, especially when paired with repeat testing strategies and symptom awareness.
People are also reading: Everything You’re Afraid to Ask About At-Home STD Tests
False Negatives and Emotional Fallout: What the Data Won’t Show
Testing negative doesn’t always mean you’re negative. Especially when the test is taken too early, the emotional relief it provides can be temporary, and dangerously misleading. Many people interpret a negative test as a green light to resume unprotected sex, unaware that the infection might not be detectable yet.
This is why public health experts recommend testing again 30 to 45 days after a risky encounter, particularly if new symptoms appear or if you’re in a high-transmission network. CDC guidelines support follow-up testing in cases of ongoing exposure or persistent symptoms, even after an initial negative result.
“That first test was a false sense of security,” said Michael, 41, who tested negative on day six, only to test positive weeks later. “I wish someone had told me that timing mattered that much.”
When “Cured” Didn’t Mean Done
Ravi, 38, thought he was out of the woods. After testing positive for syphilis last year, he received a penicillin shot and followed his doctor’s advice to abstain from sex for two weeks. But what no one told him was how common reinfection is, and how few people in his local network were testing regularly.
“Three months later, it came back. I didn’t even feel symptoms. I only tested again because my ex said he had it too,” Ravi said. “That’s when I realized: curing it once isn’t enough. You have to stay on top of it.”
This cycle, test, treat, re-expose, is one of the biggest drivers of ongoing syphilis spread. And it’s not about irresponsibility. It’s about systemic gaps, partner silence, and a lack of clear public messaging. People don’t retest because they think the story ends with a single cure. But it doesn’t.
The Stigma Spiral: Why People Still Don’t Talk About Syphilis
Syphilis carries a stigma so old it predates antibiotics. It’s still associated with moral failure, risky sex, and outdated ideas about who “deserves” to get sick. That shame keeps people quiet, and that silence keeps the disease spreading. Even in 2026, a full generation after HIV activism reshaped public health, many people still avoid saying the word out loud.
“I’ve had chlamydia twice and never felt this judged,” said Mateo, 25, a trans man living in Bogotá. “When I told a partner about syphilis, he ghosted me. I ended up deleting all my apps for months.”
This emotional cost, rejection, blame, internalized shame, leads many people to delay testing, hide symptoms, or avoid telling partners. It also creates blind spots for clinicians, who may skip routine STI screens unless prompted. The result? Entire networks of transmission where no one is talking, and no one is testing.
Eliminating syphilis requires more than medicine. It means dismantling the cultural shame that keeps people sick.
Who Gets Left Behind: Pregnant People, Yes, But Also Everyone Else
The PAHO regional agreement deserves praise for spotlighting congenital syphilis, which can be devastating during pregnancy. But in many regions, the only time someone gets tested for syphilis is during prenatal visits. Everyone else, including single adults, queer folks, and older men, often slips through the cracks.
And while PAHO’s plan calls for routine screening during antenatal care, it relies on national programs to actually implement and fund those tests. In low-resource settings, those tests are often skipped, misread, or understocked.
“When I was pregnant in Honduras, I had to pay for my own syphilis test because the clinic was out,” said Sofia, 33. “If I hadn’t insisted, they would’ve just skipped it.”
Testing during pregnancy is critical, but it must be part of a broader web of access, not the only safety net in place.
Regional Gaps in Syphilis Testing Access (2026)
Figure 2. Testing access for syphilis varies widely across the Americas. Elimination efforts must account for these gaps to succeed.
Public Health Isn’t Just Policy, It’s Personal
You can’t eliminate syphilis by spreadsheet alone. It’s not enough to pass resolutions or publish ambitious goals. Real elimination requires getting tests into real hands, especially those who are afraid to ask or unable to reach a clinic. That means removing gatekeeping, shame, and structural barriers.
It also means empowering people to take control of their own health. Whether it’s a first-time test after years of silence or a retest after a surprise exposure, access matters. Timing matters. Language matters.
That’s why STD Test Kits exists, not just to sell products, but to reduce the silence. Because when you know what’s going on in your body, you don’t just protect yourself, you stop the cycle.
FAQs
1. Can syphilis actually be cured?
Yes, and pretty easily. A single shot of penicillin can clear it, especially if caught early. The catch? That cure doesn’t come with immunity. You can treat syphilis, but your body doesn’t “learn” from it like it does with some viruses. You’re still vulnerable if you get exposed again.
2. So... can I get syphilis more than once?
Absolutely. And people do. Often. We hear from folks who’ve had it twice in the same year, sometimes from different partners, sometimes from the same one who didn’t get treated. Reinfection is real, and it’s part of why the cycle keeps going.
3. What does a syphilis sore actually look like?
Most people expect something gnarly, but the truth is... it’s sneaky. The first sore (a chancre) is usually painless and can look like a cut, a pimple, or even a razor burn. It shows up where the bacteria entered, genitals, mouth, or anus, and then disappears on its own. No drama, just easy to miss. That’s the problem.
4. I got tested three days after a hookup. Am I in the clear?
Probably not. Most tests can’t catch syphilis until 2–3 weeks after exposure. If you tested early and it came back negative, you’ll need to test again after the window closes. No shame, just timing.
5. What happens if I don’t treat it?
It sticks around. Syphilis doesn’t go away on its own. Left untreated, it can damage your brain, nerves, eyes, and other organs, even years later. It’s called “the great imitator” for a reason. But again: easy to treat, if you catch it.
6. Are at-home syphilis tests accurate?
They’re pretty solid, especially if you use them after the right amount of time has passed. At-home rapid tests detect antibodies, so they won’t work too early, but once you’re in the testing window, they’re a powerful tool. Plus, testing at home means no waiting room, no weird looks, and no paperwork trail. Just you and the result.
7. Does syphilis always cause symptoms?
Nope. Some people sail through the early stages without noticing a thing. Others get symptoms and chalk them up to something else, yeast, stress, allergies, razor burn. That’s why regular testing matters, even if you feel totally fine.
8. How do I tell a partner I tested positive?
Deep breath. It’s uncomfortable, but you’re doing the right thing. Be direct, be calm, and be kind. Try: “I recently tested positive for syphilis. I’m getting treated, and I wanted to let you know so you can check in on your health too.” If you can’t say it directly, there are anonymous notification tools to help. What matters most is that you tell them. It’s about care, not blame.
9. Can I just take a test without going to a clinic?
Yes, and you should if that feels safer or easier. You can order a Syphilis Test Kit online, use a tiny blood sample from your fingertip, and get results in minutes, no doctor visit required.
10. If I tested negative, do I still need to retest?
If you tested early, like within the first 10 days, or you’ve had new partners since, then yes, a retest is smart. Think of it like checking the mail: sometimes the info just hasn’t arrived yet. Retesting gives you peace of mind you can actually trust.
Knowing Isn’t Shameful, It’s Powerful
Syphilis didn’t survive into 2026 because people are reckless. It surv
ived because testing still isn’t easy, talking about STDs still isn’t safe for everyone, and many of us don’t realize how easy it is to miss the signs. But knowledge cuts through that fog. You don’t need perfect timing or the perfect words, you just need to know what’s happening in your body.
Don’t wait until symptoms become something scarier. This at-home combo STD test kit makes it easy to screen for syphilis and other common infections. No judgment. No waiting room. Just answers.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. CDC STI Treatment Guidelines: Syphilis
3. Syphilis – STI Treatment Guidelines (CDC)
5. Syphilis – Symptoms and Causes (Mayo Clinic)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Jenna R. Lee, MPH | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.







