At-Home HPV Test or Pap Smear? Here's How to Choose
Quick Answer: Vaginal itching that doesn’t go away after yeast infection treatment could be a sign of trichomoniasis or bacterial vaginosis. These infections can mimic yeast but require different treatment and testing.
When It’s Not Yeast: Real People, Real Symptoms
Sophia, 29, had been treating what she assumed was her fourth yeast infection of the year. “I knew the drill, itching, some discharge, no odor,” she said. “But this time, the cream didn’t help. I went back to urgent care, and they told me it might be bacterial vaginosis or trichomoniasis. I had never even heard of trich before.”
This isn’t rare. Up to 70% of people with trichomoniasis have mild or no symptoms, and when symptoms do show up, they often resemble common vaginal conditions like yeast or BV. According to the CDC, trichomoniasis is the most common curable STD in the U.S., yet it remains widely underdiagnosed because it’s often mistaken for something else.
What makes this more confusing is that people can have more than one infection at the same time. BV and trich can overlap. Yeast and trich can co-exist. That’s why treating based on assumption, especially if you’re not testing, can prolong symptoms or delay real care.

People are also reading: Can You Get HPV From a One-Night Stand? The Answer’s Complicated
Symptom Breakdown: How Trich, BV, and Yeast Overlap (and Don’t)
Let’s be blunt: vaginal symptoms aren’t always distinct. Burning, itching, weird discharge, odor, these signs get mixed up all the time, even by healthcare providers. Here’s a breakdown to help you compare what you’re feeling with the clinical patterns of each condition:
Figure 1. Visual comparison of symptoms between yeast infections, BV, and trichomoniasis. These symptoms are not definitive diagnoses and overlap is common.
Why Trichomoniasis Gets Missed, Even by Doctors
Trich is sneaky. It doesn’t always cause frothy discharge or burning. In fact, the most common symptom might just be an itch that won’t quit. That’s why it’s so often confused with yeast, especially in people who self-treat with over-the-counter antifungals. According to a recent NIH study, trichomoniasis is frequently underdiagnosed in routine care settings, especially when vaginal pH isn’t tested or when point-of-care tests aren’t used.
Here’s another issue: stigma. Many people don’t want to believe an STD could be the cause of their symptoms, so they delay testing, try home remedies, or wait it out. But trichomoniasis isn’t a moral failure, it’s a common, curable infection that just needs the right test and treatment.
If you’ve treated a yeast infection and symptoms keep coming back, or never went away, you deserve to rule out trich. And that’s where at-home STD testing can give fast, stigma-free answers.
Stay tuned, next, we’ll cover how testing for trichomoniasis actually works, when to test, and how it compares to BV and yeast in terms of timing and accuracy.
How to Actually Test for Trichomoniasis (and Not Guess)
Let’s say you’ve tried the cream. Maybe even did an online consult and were told it’s “probably yeast.” But something’s still not right. This is the moment when testing matters, and the good news is, you don’t need to sit in a clinic waiting room or explain your sex life to three different people just to get an answer.
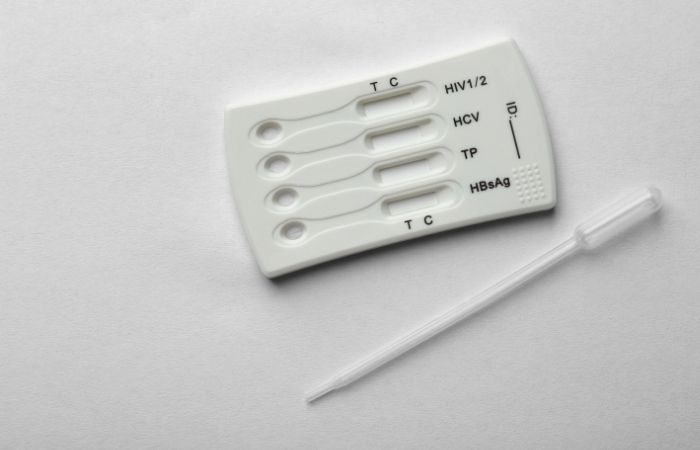
Testing for trichomoniasis is straightforward when you know what to ask for. The most accurate tests are NAATs (nucleic acid amplification tests), which can detect the parasite’s genetic material. There are also rapid antigen tests that can provide results in about 10–15 minutes, which are often used in clinics and are now available in some at-home test kits too.
Here’s how trich, BV, and yeast testing generally work:
Figure 2. Testing methods for yeast infections, BV, and trichomoniasis, including where and how long it takes to get results. Trich is the only one of the three considered an STD.
Timing Matters: When Should You Test for Trich?
If you’ve had symptoms for a few days and they haven’t improved, or if they briefly improved and then came back, it’s not too early to test. Trichomoniasis can usually be detected within 5 to 7 days of exposure, and accuracy peaks around 10–14 days. If you're not sure when exposure may have happened (or if you even had one), you can still test based on symptoms.
Here’s how testing timing plays out depending on your situation:
- Still itchy after treating yeast? If it's been more than 5 days, you can test for trich or BV now.
- Recurring discharge? Even without itching, test for trich if BV and yeast treatment failed.
- New partner in the last month? Consider a combo STD test kit that includes trich, chlamydia, gonorrhea, and more.
False negatives are possible if you test too early, so if symptoms persist after a negative result, retest in 10–14 days. This two-step testing is standard for anyone dealing with ongoing vaginal irritation with no clear diagnosis.
What Happens If You Do Have Trichomoniasis?
Here’s the thing no one tells you: trich is actually curable. One round of antibiotics, typically metronidazole or tinidazole, can clear it up. But because symptoms overlap with other vaginal infections, trich often goes untreated until someone tests or pushes for a diagnosis. That’s why your persistence matters.
If your test comes back positive, you’ll need a prescription. If you used a home test, some kits include telehealth pathways to treatment. Otherwise, bring your results to a clinic or doctor. And yes, you should tell your recent partners. Trich can be passed back and forth during vaginal sex, and reinfection is common if only one person gets treated.
But don’t panic. Trich doesn’t make you dirty. It doesn’t mean someone cheated. It just means you’re human, and now you know what’s going on.
Whether it’s for clarity, peace of mind, or to end the itching for good, testing is the next best step. Order your discreet trich test here and find out what's really going on.
People are also reading: You’re on PrEP. Do You Still Need to Worry About STDs?
Why Yeast Keeps Coming Back (When It’s Not Yeast at All)
Here’s a common pattern: you treat for a yeast infection, the itching fades briefly, then flares up again. You switch creams. You try a different probiotic. You cut out sugar. And still, your vulva feels like it’s on fire. If this cycle sounds familiar, you might be dealing with a condition that isn’t actually yeast.
Many people experience what they believe are recurrent yeast infections, but in reality, they’re dealing with undiagnosed trichomoniasis or bacterial vaginosis. A 2023 review in the journal Sexually Transmitted Diseases found that nearly 20% of self-reported “yeast infection” cases were actually trich or mixed infections.
Here’s the bottom line: if your symptoms keep coming back despite antifungal treatment, it’s time to test, not guess. Getting the wrong treatment over and over can delay healing and increase the risk of passing the infection to others.
What About pH? It’s Not Just About “Balance”
“My doctor said it was just a pH imbalance.” That might sound comforting, but it’s not a diagnosis. Both BV and trichomoniasis can raise vaginal pH above the normal range of 3.8 to 4.5. Yeast infections, by contrast, usually happen without disrupting pH.
If you've used a pH strip and the result was above 4.5, that strongly suggests it’s not yeast. But pH alone can't confirm what’s going on, it just tells you the environment has changed. That’s why you need a test that looks for the actual cause, not just the symptom.
Testing for trich, BV, and yeast together is the most accurate way to find out what’s behind your symptoms. Some at-home test kits now offer combination swabs that check for multiple vaginal infections at once, which is ideal for people dealing with repeat irritation or “mystery” discharge.
How to Care for Symptoms at Home (Without Making It Worse)
When your vulva is irritated, every product feels like a gamble. Scented soaps? Nope. Tight leggings? Painful. Here’s how to care for yourself while waiting for test results, or while deciding if it’s time to test:
Figure 3. Comfort care options while managing vaginal irritation. These do not replace diagnosis and are not curative for STDs, BV, or yeast infections.
If you're feeling unsure, it's okay to pause, take care of yourself, and test when you're ready. The most important thing is knowing that persistent symptoms aren’t your fault, and they’re not something you just have to “live with.”
When to Go to a Clinic (Or Reach Out for Help)
Home testing is convenient, but some symptoms need a closer look, especially if they involve fever, severe pelvic pain, or symptoms that worsen rapidly. If any of these apply, don’t wait:
- You’re experiencing intense abdominal pain with discharge
- You’ve tested but symptoms are getting worse, not better
- You’re pregnant and unsure what’s causing the symptoms
- You’ve had a sexual assault or need support navigating care
In those cases, a clinic or urgent care center is the right move. Bring any results from at-home tests with you, they can help providers pinpoint what to do next. If you’re in a rural area or prefer privacy, Planned Parenthood and many telehealth services offer confidential consultations by phone or video.
But for most people with mild or moderate symptoms? A discreet at-home test is often the best first step, especially if you’ve been down the “yeast infection again” rabbit hole too many times.
FAQs
1. I treated a yeast infection but I’m still itchy. Could it really be something else?
Yes, and you’re far from the only one in this boat. Itching that sticks around after antifungal treatment is a big red flag that something else might be going on, especially if your discharge looks different or there’s a weird odor. Trichomoniasis often flies under the radar because its symptoms overlap with yeast. If you’ve done “the usual” and it’s not working, it’s time to test, not guess.
2. What does trichomoniasis feel like?
Honestly? Sometimes like nothing. Other times, it’s sneaky, mild itching, a weird discharge, a funky smell after sex, or spotting when you wipe. You might chalk it up to irritation or your period being weird, but if things feel off and yeast cream isn’t cutting it, trich deserves a spot on your radar.
3. How is trich different from BV or a yeast infection?
Think of it like this: yeast is usually thick and clumpy (like cottage cheese), BV is thin and fishy-smelling, and trich can be yellowish-green, frothy, and irritating. But here’s the twist, these aren’t hard rules. You could have two at once. Or none of the “classic” symptoms and still test positive. That’s why testing is the only real way to know.
4. Can I get trich even if I’ve only had one partner?
Yes. Trich doesn’t care if it’s your first time or your hundredth. It’s often passed through vaginal sex, and many people carry it without symptoms. So even if your partner "seems fine" or you’ve been monogamous, that doesn’t rule it out. STDs don’t follow emotional logic, they follow biology.
5. Is trichomoniasis a big deal?
It can be if you leave it untreated. Trich can increase your risk of getting or passing HIV, and it’s linked to complications in pregnancy. The good news? It’s one of the few STDs that’s 100% curable with antibiotics. But you’ve got to catch it first, and that starts with testing.
6. Why do doctors misdiagnose it so often?
Because trich is a master of disguise. And because, let’s be honest, a lot of vaginal health concerns get brushed off as “yeast” without proper testing. If your provider didn’t do a swab or a specific STD test, they may have missed it. Trust your gut, if you still feel off, advocate for yourself or test at home.
7. Can I test for trich without going to a clinic?
Absolutely. There are FDA-cleared at-home trich tests that use a swab or urine sample. No stirrups, no awkward small talk, just answers. Results can be ready in minutes, or within a few days for lab-based kits.
8. If I test positive, what do I do?
Take a deep breath, you’re not dirty, broken, or alone. You’ll need a prescription antibiotic (usually metronidazole or tinidazole). Many at-home tests include treatment options through telehealth. You should also let recent partners know, so they can get treated too. It’s not about blame, it’s about stopping the ping-pong of reinfection.
9. Will trich go away on its own if I wait it out?
Nope. Unlike some mild BV cases, trich doesn’t just “clear up” with time or probiotics. It needs meds. Delaying treatment risks more irritation, partner transmission, and long-term inflammation. Testing now = peace of mind later.
10. I’m embarrassed to talk about this. Is it normal to feel that way?
Totally normal, and also unfair. Vaginal symptoms get dismissed, joked about, or shamed way too often. But your body deserves care, not criticism. There’s nothing gross about wanting answers. Whether you test at home or talk to a provider, know this: you’re doing the brave, smart thing.
When It’s More Than Just Itching: Take the Next Step
We get it, you’re tired of the back and forth. You’ve tried treating a yeast infection. You’ve Googled every possible reason you still feel off. But if your symptoms are lingering, changing, or just not adding up, it’s time to test for the things yeast cream can’t fix.
You don’t have to wait for things to get worse before doing something about it. This at-home trichomoniasis test offers privacy, speed, and clarity, so you can stop guessing and start healing.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Planned Parenthood – What is Trichomoniasis?
2. Human Papillomavirus (HPV) and Cancer – WHO
3. Human Papillomavirus (HPV) – MedlinePlus
4. HPV Infection – Symptoms & Causes (Mayo Clinic)
5. STI Risk and Oral Sex – CDC
6. Viruses That Can Lead to Cancer – American Cancer Society
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Lena Ortez, RN, MPH | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.