What a High-Risk HPV Diagnosis Means (And How to Protect Yourself)
Quick Answer: Pap smears detect cell changes caused by HPV, while self-tests detect the virus itself. Both are accurate when used correctly, but self-tests are best for people over 30 who are asymptomatic and overdue for screening. If you have symptoms or a history of abnormal results, opt for a Pap smear or co-testing at a clinic.
Who This Is For (And Why the Stakes Are Real)
This article is for anyone who’s due for cervical cancer screening but feels stuck. Maybe you’re uninsured. Maybe you live hours from the nearest clinic. Maybe trauma, dysphoria, or disability makes pelvic exams unbearable. Or maybe you just want to know if a simple, private, at-home test can give you real answers about your risk.
Let’s be clear: testing isn’t about morality. It’s about protection. HPV is the most common STI in the world, and while most strains clear on their own, some, especially HPV 16 and 18, can lead to cancer if left undetected. That’s why screening matters, even when you feel fine. And yes, it’s possible to have high-risk HPV and zero symptoms.
In this guide, we’ll cover the core differences between at-home HPV tests and Pap smears, when each one makes sense, and how to avoid common mistakes that lead to false reassurance or panic. We’ll also link you to helpful resources, like the STD Risk Checker Quiz, so you can figure out your next step in under 60 seconds.

People are also reading: Think You’re Safe Because You Haven’t Had Sex? Not So Fast
What’s the Real Difference Between an HPV Test and a Pap Smear?
The confusion is real, and it’s not your fault. Many people think a Pap smear and an HPV test are the same thing. They’re not. A Pap smear checks for abnormal or precancerous cells on your cervix. An HPV test checks for the presence of the virus that causes those changes. They serve different but related purposes.
In a clinical setting, these are often done together (called “co-testing”). But at-home HPV tests usually only check for high-risk HPV DNA, not for actual cell changes. If your at-home HPV test is positive, you’ll still need a Pap smear or colposcopy to assess whether any damage has occurred. That’s a key limitation of self-testing: it’s a first step, not a final answer.
In terms of guidelines, the CDC and USPSTF recommend HPV-first testing (with or without a Pap) for people over 30. If you’re in that age group and asymptomatic, a self-test may be a reasonable option, especially if it’s FDA-cleared and processed by a certified lab.
How These Tests Actually Work: What You’re Swabbing For
Both Pap smears and HPV tests rely on collecting cells from your cervix. The difference lies in what the lab is looking for. During a Pap smear, a clinician uses a speculum to access the cervix and collects cells from the transformation zone, the area most likely to show changes from HPV.
With an at-home HPV test, you collect your own vaginal sample using a swab or brush. The sample is mailed to a lab that looks for high-risk HPV DNA. Some tests cover 14 strains; others, only a few. The best tests are FDA-cleared, use stabilizing transport fluid, and include prepaid shipping to CLIA-certified labs.
Research shows that self-collected samples, when done correctly, can offer accuracy similar to clinician-collected ones. A meta-analysis in BMJ found self-sampling for high-risk HPV had a sensitivity of ~88% and specificity of ~97%, very close to clinic standards.
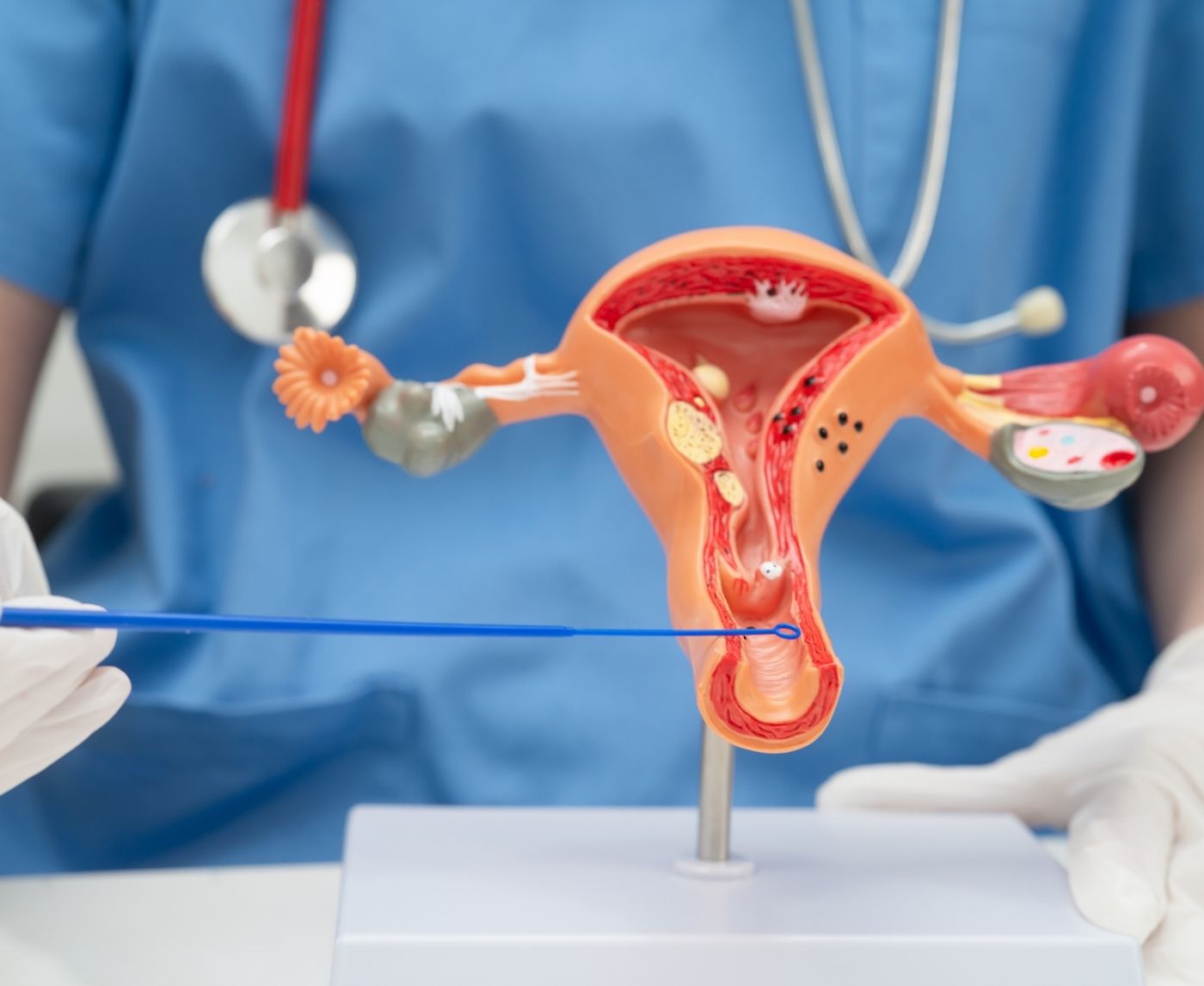
Figure 1. Comparison of HPV screening methods based on what they detect and how samples are collected.
How Accurate Is At-Home HPV Testing, Really?
This is the question that keeps people awake at night. What is the answer? It mostly depends on the brand of the test, the quality of the lab, and how you get your sample. When all three are in sync, the accuracy is very good. The reliability goes down if any of them slip up.
A 2021 study in JAMA found that samples taken by the person themselves were just as good at finding high-risk HPV strains as samples taken by a doctor. But accuracy went down when people tested too soon after being exposed, didn't follow the directions, or used a test from a provider that wasn't certified.
That's why it's important to get your information from a trustworthy source, like the lab-processed kits that STD Test Kits sells. There is real data, clear instructions, and dependable turnaround times for these tests. If you want to feel better, the quality of the test is just as important as taking it.
Why Timing Makes or Breaks Your Results
HPV doesn't show up immediately after exposure, and that’s where many people get tripped up. Just like other STDs, HPV has a window period, which is the time between exposure and when the virus becomes detectable by a test. If you test too early, your results may come back negative even if you're already infected.
Most experts recommend waiting at least 3 weeks after a new sexual partner or potential exposure before taking an HPV test. But for the most accurate results, especially for home tests, waiting 6 to 8 weeks is better. That’s when viral load is more likely to be high enough for detection.
For a full breakdown of STI window periods (including HPV), bookmark this useful guide: STD Testing Window Periods. It’s especially helpful if you’re considering multiple tests or retesting timelines.
Figure 2. Window period recommendations for HPV testing following possible exposure. Variations depending on the level of risk and the presence of any symptoms.
When Should You Choose an At-Home HPV Test?
In some situations, at-home HPV tests are the best choice. You could be a good fit if:
You are over 30, don't have any symptoms, and are due for a routine screening. You can't see a gynecologist or don't feel safe or comfortable with pelvic exams. You want a private test that you can send in by mail and that gives you control without having to wait at the clinic.
These tests offer real power, especially for people navigating medical trauma, gender dysphoria, busy schedules, or just plain burnout with the healthcare system. They can also be helpful between annual visits, or when your insurance doesn't cover regular testing.
But they’re not ideal for every situation. If you have symptoms like bleeding between periods, postcoital bleeding, pelvic pain, or discharge changes, skip the at-home test and go straight to a provider. You may need more than a viral screen, you may need a physical exam or even a biopsy.
When a Pap Smear (or Co-Test) Is the Better Choice
If you’ve had abnormal Pap results in the past, have a family history of cervical cancer, or are immunocompromised (including living with HIV), you need a clinician’s eyes on your cervix. Even if you feel fine, these risk factors warrant more thorough evaluation, including both HPV testing and visual assessment of the cervix.
Here’s another reason to choose a Pap: you’re under 30. In this age group, HPV infections are common and often transient, meaning they resolve without intervention. Routine Pap smears catch concerning cell changes without overtesting for the virus itself, which can lead to unnecessary anxiety or procedures.
And if you’ve received the HPV vaccine? That’s great news, but not a reason to skip screening. The vaccine doesn’t protect against all high-risk strains, so routine testing is still recommended.
What Happens If Your HPV Self-Test Comes Back Positive?
First, take a breath. A positive test doesn’t mean you have cancer, it means you’ve tested positive for one or more strains of high-risk HPV. Most people with HPV will never develop cancer. In fact, most HPV infections clear on their own within one to two years.
The next step depends on your age and medical history. If you’re under 30, your provider may recommend waiting and repeating the test in a year. If you’re over 30, they may schedule a Pap smear or a colposcopy to look for changes in cervical cells.
Real story: After testing positive for HPV-16 on an at-home test, Lorena, 37, scheduled a Pap. It came back normal. Her provider advised a follow-up HPV test in 12 months. A year later, she tested negative, her body had cleared the virus.
The point is: HPV doesn’t always mean treatment. Sometimes, it just means monitoring, and knowledge is power. Knowing your status lets you make informed choices about sex, screening, and your long-term health.
What If Your At-Home Test Is Negative, Can You Relax?
Yes, but with some caveats. A negative result means no high-risk HPV strains were detected in your sample. That’s a good sign, but it doesn’t mean you’re immune or protected for life. HPV can still be acquired in the future, and false negatives are possible, especially if the test was taken too soon after exposure or collected improperly.
If you’re in a monogamous relationship with no new partners, a negative test may give you peace of mind. But if you’ve had recent exposure, or are planning to change partners, consider retesting in 6–12 months for full confidence.
And remember: the accuracy of at-home tests hinges on technique. Always follow instructions carefully and choose a trusted provider. For discreet, lab-reviewed testing you can rely on, consider this HPV rapid test kit, no stirrups, no waiting room, just answers.
What If Your Self-Test Result Is Inconclusive?
It happens more often than people expect, especially with home tests. You collect your sample, send it off, and a few days later you get an “inconclusive” or “invalid” result. This can be frustrating, but it’s not necessarily a red flag about your health. More often, it’s a technical issue with the sample itself.
Common causes include insufficient sample collection, contamination (e.g., testing during menstruation), or improper storage during shipping. Most reputable testing services will offer a free retest if this happens, and some include access to clinician support to walk you through the next steps.
If you receive an inconclusive result and you’re experiencing symptoms, or just want definitive peace of mind, it’s best to follow up with a clinician-collected HPV test or co-testing. Especially if this is your first time testing or you have a complex medical history, don’t wait. Get the confirmation you deserve.

People are also reading: Mouth Sores, White Patches, or Nothing? What Oral HPV Really Looks Like
Can Men or Nonbinary People Use At-Home HPV Tests?
Most commercially available HPV self-tests are designed for people with a cervix. That means the swabs and lab protocols are validated for vaginal or cervical samples, not for penis, anal, or oral testing. However, HPV absolutely affects people of all genders.
For nonbinary people or trans men who still have a cervix, at-home testing may offer a more affirming alternative to invasive exams. That said, test kits aren’t always inclusive in their language or instructions, something many providers are working to fix. If a pelvic exam is dysphoria-inducing or simply inaccessible, self-sampling can be a critical bridge to care.
People without a cervix, such as cis men, trans women, or nonbinary folks without uterus/cervix anatomy, cannot currently use these tests. HPV testing for the penis, anus, or throat requires clinic-based swabbing or specialized kits still in development. If you're in this group and concerned about exposure, talk to a sexual health provider about risk-based testing and monitoring.
Let’s Talk About Privacy, Packaging, and What Shows Up at Your Door
One of the biggest appeals of self-testing is discretion. No waiting rooms, no awkward check-ins, no one else needs to know. But not all test providers are created equal when it comes to privacy.
Here’s what you should look for when ordering an at-home HPV test:
- Discreet shipping: The package should be plain, with no sexual health or STI labeling.
- Clear return packaging: Most kits include a pre-paid return label and tamper-evident bag.
- Digital results: Choose a service that delivers results online via a secure portal, not email or text alone.
The best services also offer guidance after results, whether that’s a direct telehealth referral or instructions on what kind of provider to contact. If you test positive and feel overwhelmed, you should never be left on your own to Google next steps.
Want to see what discreet, lab-backed self-testing looks like? Browse the kits at STD Rapid Test Kits. It’s health empowerment in a plain box.
“I Waited Too Long, Then Got a Scare”
Jenna, 41, hadn’t had a Pap smear in nearly a decade. Between raising kids, working full-time, and the awkwardness she felt during exams, screening kept falling to the bottom of her list. One night, after seeing a friend share her cervical cancer diagnosis online, Jenna panicked and ordered an at-home HPV test.
The result came back positive for HPV-18. She immediately booked a Pap, which showed moderate dysplasia, precancerous cell changes. Her doctor said the timing was lucky. With a few more years of delay, things might have looked different.
“The self-test saved me,” Jenna says. “It gave me the nudge I needed to act.”
Her story isn’t rare. Many people use at-home tests as a gateway to re-engaging with care. If that’s your situation, if fear or shame or trauma has kept you from the stirrups, there’s no judgment here. Start with the test that feels doable. Then take it from there.
Cost Comparison: What You’ll Pay (And What Insurance Covers)
Pap smears and HPV co-testing are usually covered under preventive care mandates for insured patients. But if you’re uninsured, out of network, or dealing with high deductibles, the out-of-pocket cost can climb to $150–$400 depending on location and whether follow-up procedures are needed.
At-home HPV tests range from $49 to $149. The price depends on whether the kit includes lab processing, digital results, and clinician access. Cheaper kits may not include certified lab work or use transport media that degrades the sample during shipping, so be cautious with ultra-low prices.
If you're low-income, some public clinics or Planned Parenthood locations offer free or sliding-scale HPV screening, including mail-in self-tests for eligible patients. Check local options before assuming self-testing is your only route.
Get Clarity Without Compromise
You shouldn’t have to choose between accuracy and autonomy. Whether you’re screening for the first time in years or simply want a less invasive option, there’s a test that meets you where you are. HPV testing isn’t one-size-fits-all, but the goal is always the same: protect your body, your future, and your peace of mind.
Order your discreet HPV rapid test kit today. It’s fast, private, and processed by trusted labs, because you deserve real answers, not more worry.
FAQs
1. Can I really trust an at-home HPV test?
Yes, if you are working with a legit one. Also, be looking for those that are FDA-approved and analyzed in credible labs (not those instant analyses with nothing to follow through on). Given proper use, they do almost the same thing in testing for the high-risk strains of the human pap virus as a sample collected by a doc.
2. Is a Pap smear better than an HPV self-test?
It depends what you mean by "better." A Pap smear checks for abnormal cells on your cervix. An HPV test checks for the virus that causes those changes. For people over 30, an HPV test may actually catch risk earlier. But if you’ve got symptoms, past abnormal Paps, or want a full picture, Pap smears (or co-testing) are the gold standard.
3. I'm under 30, can I still take a home HPV test?
Technically, yes. But it’s not usually recommended unless a provider specifically tells you to. HPV is super common under 30, and your body often clears it on its own. That’s why Pap smears are the go-to for that age group. If you're feeling anxious though, talk to your doctor, peace of mind matters, too.
4. What happens if I test positive for HPV?
First of all, don’t panic. Having a positive test result means you’re infected with a high-risk type of the human pap virus, but it doesn’t mean you’re infected with cancer. Most people clear the virus on their own and especially if you’re under the age of 35. For those over the age of thirty, a Pap test and a colposcopy will be the next step.
5. I tested negative, am I in the clear?
Probably, but don’t get too comfortable. Getting a negative test result is fantastic news, but it doesn’t mean you’re safe forever. You can still be infected with the virus through a new sexual partner, and there’s a chance of a false negative test result, especially if the test was conducted too early. If, however, you switch sexual partners and want to know for certain, retest in 6 to 12 months.
6. What if my self-test result is “inconclusive” or “invalid”?
Ugh, we know, it’s the worst. But it doesn’t mean anything's wrong with you. Usually, it means the sample wasn’t collected quite right, or it didn’t survive the shipping process. Most good test providers will send a replacement kit. If you’re nervous or have symptoms, skip the retest and head to a clinic.
7. Can men or nonbinary folks use these tests?
If you have a cervix, then yes, no matter the gender identity. Lots of transfags and nonbinary people find an at-home test much more validating than a spec exam. Just make sure the test instructions make you feel included and that you are comfortable doing the test yourself. For people who don't have a cervix, i.e., cis guys and people who have had a hysterectomy, the test for HPV will need to be done differently.
8. I’ve had the HPV vaccine, do I still need to test?
"Yeah. The vaccine will protect against the most dangerous strains, but not against all of them. You can still get infected with a type that the vaccine doesn’t protect against." Even if you’re vaccinated, you still need to be checked out periodically if you’re over thirty or if you’ve had new partners.
9. How often should I test for HPV?
If you're over 30 and healthy, you might only need to test every 5 years, especially if you do co-testing (Pap + HPV). But if you’ve had a past abnormal result or are immune-compromised, your provider might recommend a tighter timeline. And hey, if you're ever in doubt? Test. It's your body, you call the shots.
10. Will anyone know I ordered a self-test?
Not unless you tell them. Kits from places like STD Test Kits ship in plain packaging with no health labels. Results are delivered through secure online portals, not texts your roommate might see. Your body, your results, your business.
You Deserve Answers, Not Assumptions
HPV is common. Cancer isn’t, but the risk goes up when you don’t know your status. Whether you test at home or in a clinic, the most important thing is that you do it. Testing isn’t about guilt or shame, it’s about owning your health, protecting your partners, and catching issues early while they’re still easy to treat.
Don’t wait for a scare. Don’t wait for symptoms. And definitely don’t wait for someone else to give you permission. Order a discreet HPV test today, or call your provider to get screened. Either way, you're making a decision rooted in care.
Sources
1. USPSTF – Cervical Cancer Screening Guidelines
2. Planned Parenthood – Cervical Cancer
3. CDC: Screening for Cervical Cancer — Pap Test and HPV Test
4. American Cancer Society: HPV Testing — What to Know
5. Mayo Clinic: HPV Test — Overview
About the Author
Dr. F. David, MD is a board-certified infectious disease doctor who specializes in preventing, diagnosing, and treating STIs. He is dedicated to making his work available to more people, whether they live in cities or off the grid. He combines clinical accuracy with a straightforward, sex-positive approach.
Reviewed by: R. Chen, MSN, WHNP-BC | Last medically reviewed: December 2025