You Can Get an STD from Oral Sex, Here’s How It Happens
Quick Answer: STD symptoms in the mouth, like red patches, ulcers, white spots, or persistent sore throats, are often noticed first by dentists during routine exams, especially if you’ve had recent oral sex or kissing exposures.
This Isn’t Just a Canker Sore, And Here’s Why
If you’ve ever had a sore in your mouth, you’ve probably been told it’s “just a canker.” And most of the time, that’s true. But when a sore doesn’t heal within 10 days, looks unusually deep, or comes with throat pain and swollen glands, it’s worth looking closer, especially if you’ve recently engaged in oral sex.
Dr. Nabila Iqbal, a dentist in Austin, recalls a patient she referred out for testing after noticing irregular ulcers under the tongue. “It looked like a trauma lesion at first,” she says. “But the shape, color, and how long it had been there, it didn’t add up. I advised him to get tested, and it turned out to be herpes simplex.”
The tricky part is that oral STD symptoms can mimic everyday dental issues. That sore might not be from spicy food. That white film on your tonsils might not be allergies. Dentists are trained to look for patterns that don’t match the usual suspects, and many are becoming unofficial frontline screeners for oral STDs without even meaning to be.
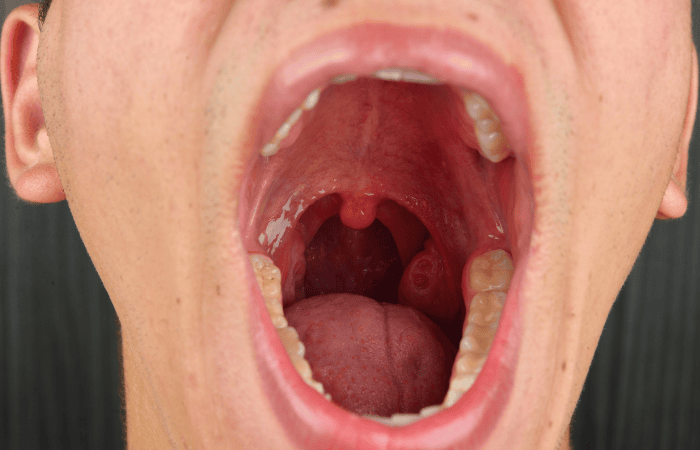
Red Flags in Your Mouth: What STDs Look Like Up Close
While STDs often go unnoticed in their early stages, the mouth can tell a very different story, if someone knows what to look for. Oral sex and deep kissing can transmit infections like gonorrhea, herpes, syphilis, chlamydia, and even HPV. And some of them show up in visible ways that a dentist might catch during a routine checkup.
Here's a breakdown of some of the most common oral manifestations that raise red flags during dental exams:
Table 1. How different STDs may appear inside the mouth, and how they can be spotted during a dental exam. Dentists aren't diagnosing STDs, but they may see signs others miss.
People are also reading: What Does HPV Look Like in Men? (Sometimes, Nothing at All)
What Your Dentist Sees (and What They Can, and Can’t, Say)
Here’s the thing: your dentist isn’t legally diagnosing you with an STD. In most places, they aren’t allowed to. But they can tell when something looks suspicious, and they’ll often recommend a visit to your primary care provider or a sexual health clinic to get it checked out.
Dental professionals are trained to screen for oral cancers, chronic infections, and systemic disease indicators, which includes many signs that overlap with sexually transmitted infections. If they see an ulcer that doesn’t behave like a trauma wound or a spot on your tonsil that shouldn’t be there, they’ll document it and usually suggest further testing. Some may even hand you a referral note with something vague like “rule out infectious cause” written on it.
Anna, 23, got a wake-up call when her dentist asked if she’d been feeling sick lately. “I had no idea oral gonorrhea was a thing,” she said. “I thought my throat was just irritated from vaping.” But the exam turned up telltale swelling and redness, just enough to push her to get tested. She was positive for both gonorrhea and chlamydia in her throat, despite having zero genital symptoms.
It's not uncommon. In fact, oral STDs are often completely asymptomatic, and only found during unrelated exams like dental visits. That makes them easy to spread unknowingly, and harder to track unless someone knows where to look.
The Problem With Silent Infections in the Mouth
One of the scariest things about oral STDs? Many of them don’t hurt, don’t itch, and don’t look like anything special. You can walk around with an active infection in your throat and not even know it, until someone else starts showing symptoms after kissing or oral sex.
This is especially true with gonorrhea, which can sit in the throat for weeks or months without a single cough or sore. In the meantime, the bacteria is still active and transmittable. The same goes for chlamydia and herpes, they can take up residence in the oral tissues and live there quietly unless triggered.
That’s why catching these infections early, whether through symptoms or routine testing, is so important. A dentist isn’t a substitute for sexual health screening, but they might be the reason you decide to finally get one.
And if you’re thinking, “But I feel fine,” consider this: According to the CDC, over 50% of throat gonorrhea infections occur without symptoms, and still spread to partners.
Can You Really Get an STD from Kissing or Oral Sex?
The short answer is yes, and it’s more common than most people realize. Oral sex can transmit a range of infections, even if it feels “lower risk” than vaginal or anal sex. That includes gonorrhea, chlamydia, herpes simplex virus, syphilis, and even HPV or HIV in rare cases. And deep kissing, especially when there are cuts or sores in the mouth, can also spread herpes or syphilis.
Picture this: Sam hooked up with someone new, and it never went “all the way.” Just some making out, mutual oral, and a late-night goodbye. Two weeks later, he noticed red patches on his tonsils and a strange taste in his mouth. He thought it was strep, but the strep test came back negative. A few days later, his doctor called back: oral gonorrhea. He never knew kissing and oral could pass it on.
There’s no judgment here, just facts. Even without ejaculation, even with condoms used for penetration, oral sex can expose your throat, tongue, tonsils, and gums to STDs. And if you’re the one performing oral, you’re often at greater risk because the mucous membranes in the mouth absorb bacteria and viruses quickly.
Why Oral STD Testing Often Gets Skipped (And Why That’s a Problem)
Here’s something most people don’t know: unless you specifically ask for it, most STD panels don’t include throat or mouth testing. Clinics and labs usually default to urine tests and genital swabs, especially if you don’t mention oral sex in your history. That means if you’ve been exposed through the mouth, a standard test might completely miss it.
Even when someone does request testing, providers often skip oral samples unless symptoms are visible. It's part of why oral STDs fly under the radar. And if you’ve already been to a clinic and got a “negative” result without a throat swab? You might not be as clear as you thought.
That gap in testing has real consequences. If you’re unknowingly carrying gonorrhea in your throat, you can give it to others, through oral, kissing, or even shared objects like vape pens or sex toys. Silent infections = silent transmission.
Luckily, some at-home test kits now include oral swabs, especially for those who report recent oral exposure. If you're unsure whether yours does, check the product page or FAQ section. STD Rapid Test Kits offers discreet combo kits that can test for oral exposure alongside genital samples. If you're not sure what you need, this combo test kit covers the most common infections and includes easy-to-follow instructions.
Testing the Throat: What Happens and How Accurate Is It?
If your provider, or your test kit, includes an oral swab, here’s what happens: a soft brush or swab is rubbed along your tonsils and the back of your throat. It might tickle or gag slightly, but it’s quick. The sample is then analyzed for DNA of common STDs using nucleic acid amplification testing (NAAT), which is the gold standard.
Here’s what you should know about accuracy:
Table 2. Common oral STD testing methods, with expected accuracy and ideal timing. Testing too early can lead to false negatives, retesting may be needed if symptoms develop later.
If you’ve had recent oral exposure and your test came back negative but something still feels off, don’t ignore it. Many providers recommend retesting after 2–4 weeks if symptoms show up later or if the test was taken too soon after exposure.
Case File: When the First Test Missed It
Jasmine, 30, had a negative STD test at an urgent care clinic after an unprotected oral encounter. Her test panel was clean, no chlamydia, no gonorrhea, no syphilis. But two weeks later, she noticed swollen glands in her neck, a white patch on her left tonsil, and a burning feeling that wouldn’t go away. She went back and specifically requested an oral swab. That test came back positive for gonorrhea.
“I was floored,” she said. “I didn’t even think I needed to test for that. The first clinic never mentioned the mouth.”
This happens more than people realize. If the timing is off, or if the right areas aren't tested, early infections can sneak past the radar. Dentists are sometimes the first to raise the red flag. But follow-up testing is still key.
Trust your instincts. If something feels off, it probably is. And if your mouth or throat starts showing weird symptoms, persistent soreness, ulcers, or white patches, after a new partner or hookup, don’t wait. You don’t need to feel sick for an STD to be active.
Testing at Home: How to Get Oral Swabs Without the Awkwardness
If the idea of going into a clinic makes you anxious, or if you're just not ready to answer awkward questions, at-home testing is a legitimate option. Many providers now offer test kits that include oral swabs, allowing you to collect a sample from your throat and send it in for analysis.
These kits come with clear instructions, are packaged in a way that doesn't draw attention to them, and don't require any face-to-face contact. Some, like the Combo STD Home Test Kit, include swabs for oral, genital, and sometimes rectal testing, all depending on your exposure and preferences. Results usually arrive within 2–5 business days, and you can decide how to follow up from there.
It's not just about convenience, it's about control. Testing from home lets you take your health into your own hands, especially if you’ve had an oral exposure or if something felt off after kissing or giving oral. You don’t need to wait for symptoms to start (or worse, wait for a partner to mention theirs).
If your head’s spinning, remember: peace of mind is just one test away.
When to Retest, and Why One Negative Isn’t Always Enough
Let’s say you tested negative after oral sex. No symptoms, clean panel, and a sigh of relief. But then, a few days or weeks later, your throat feels weird. Or you notice a new sore in your mouth. Or your partner says they just tested positive. Now what?
This is where retesting matters. No test is perfect, especially when it comes to timing. Testing too early after exposure can lead to false negatives, simply because the infection hasn’t built up enough to be detected yet. It’s not about failure; it’s about biology. Your body needs time to develop detectable levels of bacteria, viral DNA, or antibodies.
Here’s a general rule of thumb: if you test within 5 days of exposure and it's negative, that’s not a final result. Many oral infections, especially gonorrhea and chlamydia, take at least 7 to 14 days to reach detectable levels in the throat. And even then, some providers recommend a follow-up at 30 days just to confirm.
Case in point: Carlos, 27, tested negative 4 days after a high-risk hookup. But his sore throat wouldn’t go away. He re-tested at day 15 with a self-swab kit. This time? Positive for chlamydia in the throat. “I didn’t even think to retest. I just assumed I was fine,” he said.
If you’ve started treatment (say for syphilis or herpes), retesting can also be helpful to confirm that the infection is under control or fully cleared. But timing matters here, too, testing too soon after antibiotics or antivirals may show leftover traces, even if you’re no longer infectious.
How to Talk About It Without Freaking Out
Let’s get real: bringing up an STD, especially one that started in your mouth, is not an easy conversation. But it doesn’t have to be a scary one. Most people who test positive for oral gonorrhea, chlamydia, or herpes have no idea they were even exposed. And many have passed it to others without knowing.
The truth is, saying something simple like, “Hey, I got tested and found something I didn’t expect, I just want you to know” is enough. You don’t need to script a perfect speech. You just need to keep it honest and grounded in care.
Remember, STDs aren’t punishments. They’re incredibly common infections that thrive on silence and shame. Breaking that cycle starts with being brave enough to say something.
If you’d rather notify someone anonymously, many public health departments and telehealth platforms offer tools to send a confidential message. You can also use partner notification services, which let you alert past partners without attaching your name.
The same goes for letting someone know your dentist noticed something odd, no need to spiral. Just explain what was seen and that you're taking the steps to rule things out. It's about responsibility, not embarrassment.

People are also reading: When Pink Eye Is Actually an STD: What to Look For
Prevention Is a Conversation, Not Just a Condom
We tend to think of condoms as the gold standard for STD prevention. And they are. But when it comes to oral sex, the equation changes. Many people don’t use barriers for oral, and even fewer use dental dams during oral-vaginal contact. That means your mouth is wide open, literally, for exposure.
Preventing oral STDs isn’t about shame, it’s about choice. You can use flavored condoms or dental dams. You can ask your partner about recent testing. You can rinse your mouth after oral sex (but avoid brushing immediately, since it can create tiny cuts). You can even get vaccinated, HPV vaccines like Gardasil can prevent strains that cause oral cancers and genital warts.
More than anything, prevention means staying in the loop about your own body. If you notice something weird in your mouth, an ulcer, a red spot, swollen tonsils, or a new burning sensation, don't write it off. Take a picture. Track how long it lasts. And if it sticks around or gets worse, test.
It’s not about living in fear. It’s about staying curious and informed. Your dentist might spot something first, but you get to choose what happens next.
What Happens If You Don’t Catch It?
Let’s talk consequences, not to scare, but to ground things in reality. Oral gonorrhea left untreated can lead to painful throat infections, spread to the bloodstream (rare but serious), and even contribute to antibiotic resistance. Untreated syphilis can progress to more dangerous stages, and herpes can cause recurring painful outbreaks.
But perhaps most importantly, when you don’t know you’re infected, you keep passing it on. Kissing, oral sex, sharing vape pens or straws, all of it becomes a risk for others. And while you may not feel symptoms, someone else might.
Think of testing as community care. You’re not just protecting yourself, you’re looking out for the people you’re intimate with, even casually. One quiet throat infection can become five new cases if it’s left unchecked. But one quick test can stop it in its tracks.
Most oral STDs are easily treatable with antibiotics or antivirals. The hard part isn’t the cure, it’s catching them early enough to stop the cycle. And that starts with paying attention to your mouth, listening to your dentist, and trusting your gut.
FAQs
1. Can a dentist really tell if I have an STD?
They won’t say “You have gonorrhea,” but they might raise an eyebrow and ask how long you’ve had that sore. Dentists see thousands of mouths a year, they know what doesn’t look right. If something’s off (like a deep ulcer, inflamed tonsils, or weird white patches), they’ll usually suggest seeing a doctor or getting tested. It’s less about diagnosis and more about red flags.
2. Which STDs actually show up in your mouth?
More than you think. Herpes (yep, even HSV-2), gonorrhea, chlamydia, syphilis, and HPV can all affect the mouth or throat, especially after oral sex. Sometimes it’s blisters, sometimes ulcers, sometimes just a sore throat that won't quit. And sometimes? Nothing at all. Totally silent. That’s the scary part.
3. Can I get an STD from kissing?
You can. It’s not the most common route, but if there are cuts, cold sores, or oral lesions involved, infections like herpes or syphilis can spread through deep kissing. It’s rare, but not impossible. Most of the time though, oral sex is the bigger risk.
4. What does oral gonorrhea actually feel like?
Here’s the kicker, it often doesn’t feel like anything. But when it does, it can mimic strep: sore throat, redness, maybe a little pus or swollen tonsils. Sometimes it’s just a funky taste in your mouth. If you've had oral sex recently and your throat feels off, it’s worth checking out, even if it just feels like allergies or a vape hangover.
5. How soon after oral sex should I test?
Best bet is 7 to 14 days after exposure. Sooner than that, and you might test too early to catch anything. If symptoms pop up earlier, you can test right away, but be ready to retest later if it's negative. Some folks test at day 5, feel relief, then test again at day 15 and get a surprise.
6. Do at-home STD kits test your mouth, too?
Not all of them. That’s why you have to check the fine print. Many kits only cover urine or genital swabs unless you choose a combo kit with an oral swab included. This one does. If your exposure was oral, testing the mouth matters, otherwise you’re flying blind.
7. I tested negative but still have symptoms. Should I retest?
If you tested too soon, yep, retest. If your kit didn’t include a throat swab, double yep. STD symptoms can lag, and many tests have windows where they miss early infections. Trust your body. If something still feels off, don’t gaslight yourself. Retesting is normal. Smart, even.
8. Could I have an STD in my mouth and not down there?
Absolutely. If your only exposure was giving oral sex, the infection might stay localized to your mouth or throat. It’s why site-specific testing is so important, and why just peeing in a cup doesn’t always tell the full story.
9. What if I have cold sores but haven’t had sex?
You’re not alone. Most cold sores are caused by HSV-1, which many people get in childhood from non-sexual contact. It’s still technically an STD, but don’t let that label scare you. It’s incredibly common and not always linked to sex. If you're unsure whether it’s herpes or something else, testing can help clear the air.
10. Should I tell my partner if I have oral herpes?
Yes. It’s the kind of honesty that builds trust, not breaks it. You don’t have to make it dramatic, just be clear about what you know and how you manage it. “I get cold sores sometimes; it’s oral HSV-1. Just wanted you to know in case it matters to you.” That’s it. Most people appreciate the heads-up.
You Deserve Answers, Not Assumptions
Your mouth is more than a place for words, food, or kisses. It's also where early signs of infection can quietly begin, and where professionals like your dentist might spot something worth checking.
If you've had a new partner, oral sex, or even a makeout session that left you wondering, trust that instinct. Whether you feel symptoms or not, you don’t need permission to get tested. You deserve clarity, control, and care.
Don’t wait and wonder, this at-home combo test kit checks for the most common STDs discreetly and quickly. Oral swabs included, no judgment required.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. CDC – Gonorrhea Detailed Fact Sheet
2. Planned Parenthood – Herpes Education
3. About STI Risk and Oral Sex – CDC
7. About Genital HPV Infection – CDC
8. Getting Tested for STIs – CDC
9. Sexually Transmitted Diseases (STDs) – Mayo Clinic
10. Sexually Transmitted Infections – StatPearls (NCBI)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Amanda T. Reyes, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.







