Took the Antibiotics but Still Feel Off? You’re Not Imagining It
Quick Answer: The best probiotics for vaginal health contain strains like Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14, which have been clinically shown to reduce BV, yeast infections, and restore vaginal flora, especially after antibiotic or STD treatment.
Why Vaginal Probiotics Are Different (And Why That Matters)
You might already be taking a probiotic, for digestion, bloating, or gut health. But vaginal health requires a very different bacterial environment. While gut probiotics focus on bifidobacteria and a mix of lactobacillus strains, the vagina depends almost entirely on specific types of Lactobacillus to maintain a healthy acidic pH (around 3.8–4.5), which helps keep yeast, BV, and even certain STDs in check.
Picture this: after a week on antibiotics for gonorrhea, Kayla, 26, noticed a sudden surge of watery discharge with a fishy smell. Her STD symptoms were gone, but now something else had shifted. Her doctor explained that while the meds cleared the infection, they also wiped out the “good bacteria” in her vaginal microbiome, leaving room for BV to bloom. This is where targeted probiotics come in, not just to replace bacteria, but to rebalance the entire vaginal ecosystem.
Here’s the core problem: most shelf probiotics don’t include the strains proven to colonize the vagina. And even among vaginal-specific options, few offer the right delivery system (oral vs. vaginal) or enough CFUs (colony-forming units) to make a difference.
Which Symptoms Point to a Vaginal Flora Imbalance?
Maybe you’re not dealing with a full-blown infection, but things just feel...off. Mild itchiness. A small smell. Discharge that is not the same as what you usually have. STI tests and Pap smears often miss these less obvious symptoms, but they still affect comfort, confidence, and overall sexual health. Sometimes they emerge after sex. Sometimes after your period. Sometimes for no obvious reason at all.
Consider Bri, 33, who began experiencing thick white discharge after using a spermicide with her partner. It wasn’t her typical yeast infection, but it also wasn’t nothing. She wasn’t sure if it warranted a doctor’s visit, or if she could rebalance things herself. She tried a store-brand probiotic labeled “women’s blend,” but it didn’t help. Only later did she learn that the strain she needed, Lactobacillus reuteri, wasn’t even included.
To make sense of what strain helps with what, we’ll break it down by symptom and condition below. But first, here’s why timing and delivery route also matter.

People are aslo reading: That UTI Might Be Chlamydia, Here’s How to Know for Sure
Oral vs. Vaginal Probiotics: What the Research Shows
It’s tempting to think that putting probiotics “where the problem is” makes the most sense. And in some cases, like severe recurrent BV, vaginal capsules may offer faster results. But most of the best-researched strains for vaginal health have actually been studied in oral form. Why? Because when taken orally, certain strains survive the gut and colonize the vagina via the rectal-vaginal pathway. It sounds weird, but the gut and vagina are surprisingly interconnected.
In fact, a seminal 2006 study on Lactobacillus rhamnosus GR-1 and reuteri RC-14 found that oral doses could significantly reduce recurrence of BV and yeast infections within weeks. These strains have since become the gold standard for vaginal probiotics, and are notably absent from most generic supplements.
Still, there are cases where vaginal delivery might be better. If you’ve just finished antibiotics, are prone to persistent infections, or have trouble with absorption, a vaginal probiotic suppository may offer direct relief. Just make sure the product uses strains proven to colonize the vaginal epithelium, not random gut blends.
Figure 1. Choosing between oral and vaginal probiotics depends on your current symptoms, recurrence history, and sensitivity to treatment methods.
Which Probiotic Strains Actually Work for Vaginal Health?
Start with this: not all Lactobacillus are created equal. Some are good for your gut, some are good for your skin, but only a few have been proven in clinical trials to restore and protect the vaginal microbiome. Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 are the two strains that are most studied. These aren’t just buzzwords, they’re strain-level specifics backed by randomized, controlled studies. And yes, that matters. Without strain-level ID, you’re basically buying mystery microbes and hoping they help.
Take Jenna, 29. After taking antibiotics for a persistent urinary tract infection, she started experiencing milky discharge with a metallic odor. Tests for BV and STDs came back negative. Still, something felt off. She tried a “gut + vaginal” probiotic blend from a big wellness brand, but her symptoms persisted. After reading clinical studies online at 2AM (because that’s when anxiety peaks), she ordered a supplement containing GR-1 and RC-14. Two weeks later, the odor faded. It didn’t happen overnight, but it worked. The difference? A few strains can literally talk to your immune system and settle into the vagina the way they’re supposed to, instead of just passing through your gut.
Lactobacillus crispatus is another strain to keep in mind because it is naturally dominant in the healthiest vaginal microbiomes. Lactobacillus acidophilus may help keep the pH balance, but it hasn't been studied as much for direct vaginal effects.
Figure 2. Each probiotic strain plays a unique role in vaginal health. Matching the strain to the symptom increases your chance of success.
Can Probiotics Help After an STD?
Let’s be real: treating an STD like chlamydia or gonorrhea doesn’t always end with the last antibiotic pill. For a lot of people, treatment is followed by a second wave of symptoms, not from the STD itself, but from the microbial chaos left behind. This is especially common with BV flare-ups, yeast infections, or general irritation that feels like something’s still wrong.
Here’s where vaginal probiotics become more than just wellness fluff. They help repopulate the vagina with protective Lactobacillus species that were likely wiped out during treatment. Some studies suggest that early probiotic use post-antibiotics can reduce recurrence of BV by up to 50%, and can help restore the acidic environment that discourages STD re-infection. It’s not a cure-all, but it is a tool in the toolkit.
Consider Malina, 24. After being treated for trichomoniasis, she started a course of probiotics containing GR-1 and RC-14, on her nurse practitioner’s recommendation. She was skeptical at first. But six weeks later, her vaginal symptoms had completely resolved. More importantly, she hadn’t had a recurrence, which was a first. Malina later said the probiotic gave her a sense of control after a scary diagnosis, something that mattered just as much as the symptom relief.
Can the Wrong Probiotic Make Things Worse?
Yes. In some cases, taking the wrong probiotic, or the wrong dose, can do more harm than good. Formulas designed for gut health may disrupt your vaginal flora if they contain strains that compete with Lactobacillus. Also, supplements that haven't been tested in a lab might not have viable CFUs, especially if they weren't stored correctly or were exposed to heat while being shipped.
Another risk? Overdosing. While rare, some people experience bloating, nausea, or even increased discharge when starting a new probiotic. This can happen when you’re already dealing with an infection or your body reacts to the influx of new microbes. Always start with one capsule per day, unless directed otherwise. And if symptoms worsen, pause and consult a provider familiar with microbiome health, not just a pharmacist reading a label.
And then there’s the issue of expectation. If you’re using probiotics to treat an active STD or yeast infection without first treating the underlying cause, you’re setting yourself up for disappointment. Probiotics support, not replace, treatment. They’re best used after antibiotics, as a preventive tool, or to gently address low-grade symptoms of imbalance. If you have burning, lesions, or intense odor, get tested first. Then think about what probiotics can help with next.
Are Refrigerated Probiotics Better?
This is one of the most common questions people have. Short answer: not necessarily. While it’s true that probiotics are live cultures and can degrade at high temperatures, many modern formulas use freeze-drying technology that keeps strains stable at room temp. That said, if a product requires refrigeration, make sure it’s shipped cold, and stored properly. If it’s been sitting on a hot warehouse shelf for weeks, those bacteria may already be dead by the time you take them.
Focus more on the strain, CFU count (look for 1 billion or higher for vaginal support), and whether the brand offers transparent third-party testing. Don’t get caught up in branding terms like “women’s blend” or vague health claims. The right strain matters more than the color of the bottle.
When Should You Take Probiotics for Vaginal Health?
The timing of probiotic use is something most people overlook, yet it often makes the difference between “this helped a little” and “wow, that actually fixed it.” Vaginal flora shifts throughout your menstrual cycle, after sex, and even during periods of stress. Think of your vaginal microbiome as a neighborhood that needs stability; the best time to take probiotics is when that neighborhood is either rebuilding or already calm enough to welcome new residents.
Imagine Sara, 31, who always felt irritation right after her period. It wasn’t a full-blown yeast infection, but a raw sensation she described as “like my vagina forgot how to be itself.” She tried switching soaps, underwear, even detergents. Nothing changed. When she started taking her probiotic consistently right after her period ended, things finally stabilized. Why? Because estrogen begins to rise again in that phase, boosting natural Lactobacillus growth, meaning the probiotic strains had a friendlier environment to settle into.
Sex also influences timing. Semen is alkaline, and even protected sex can shift vaginal pH due to friction, lube ingredients, or microtears. For people prone to BV or yeast overgrowth after intercourse, taking probiotics within a few hours of sex, or daily during sexually active periods, can help the vaginal flora bounce back faster. It’s not about treating anything; it’s about reinforcing the groundwork so issues don’t take hold in the first place.
Figure 3. Timing probiotic use with natural vaginal shifts helps strengthen colonization and symptom control.
Do Probiotics Help With Vaginal Discharge and Odor?
Let’s talk about discharge, the topic people whisper about but Google in a panic at 1AM. Discharge changes are one of the most common reasons people try vaginal probiotics, yet many don’t know which type of discharge points to which imbalance. A thin grayish fluid with a fishy smell hints at BV, while thick cottage-cheese-like clumps lean toward yeast. A watery, musty odor often appears after antibiotics or hormonal shifts. Probiotics don’t “fix” discharge directly; they alter the microbial environment that creates it.
Mia, 22, once described her symptoms like this: “It’s not bad enough to call my doctor, but bad enough that I’m thinking about it every day in class.” Her discharge wasn’t intense, just different, slightly mustier and more frequent. After three weeks of a targeted probiotic with GR-1 and RC-14, her symptoms leveled out. What improved wasn’t the discharge itself but the ratio of helpful bacteria keeping the vaginal pH acidic and stable. Her vagina began communicating less distress.
Persistent or worsening odor always deserves medical testing, because untreated infections, especially trichomoniasis, can mimic BV. But once an infection is ruled out or treated, probiotics can help restore the microbial landscape that prevents that smell from returning. Think of it as re-seeding a garden after pulling out weeds; the shape of the garden changes slowly, not overnight.

People are aslo reading: Doctors Said It Was Nothing, Turns Out It Was Herpes
How Long Do Probiotics Take to Work?
Most people expect change within a few days, but vaginal probiotics don’t operate on the same timeline as antifungals or antibiotics. They aren’t killing things; they’re rebuilding. That process takes time. Most clinical studies show improvements around the 2–4 week mark, with the most significant changes felt after consistent daily use for at least a month. Faster relief can happen when probiotics are paired with lifestyle shifts like breathable underwear, reduced sugar intake, or switching lubricants, but the microbes themselves still need time to colonize responsibly.
Take Naya, 34, who battled recurring BV for years. She once said, “I’ve tried every probiotic on Amazon.” She’d take a supplement for three days, see no difference, then throw it out. When her nurse practitioner explained that probiotics build stability gradually, not instantly, Naya committed to six weeks of consistent use. For the first time in years, she made it through two cycles without a flare-up. Her vagina didn’t change overnight; it changed slowly, like a city rebuilding after too many storms.
If symptoms worsen in the first week, don’t panic. Mild temporary increases in discharge or digestive shifts can happen as your body adjusts. But severe odor, pain, or burning isn’t a “detox”, it’s a sign you need STI testing or yeast/BV evaluation before continuing self-treatment.
When Probiotics Aren’t Enough: The Red Flags
Probiotics are powerful, but they aren’t cure-alls. They can’t clear chlamydia, gonorrhea, trichomoniasis, or herpes. They won’t treat a full-blown yeast infection or reverse pelvic inflammatory disease. And they can’t override severe pH disturbances caused by douching, harsh products, or repeated unprotected sex with a partner whose semen chemistry consistently disrupts your flora.
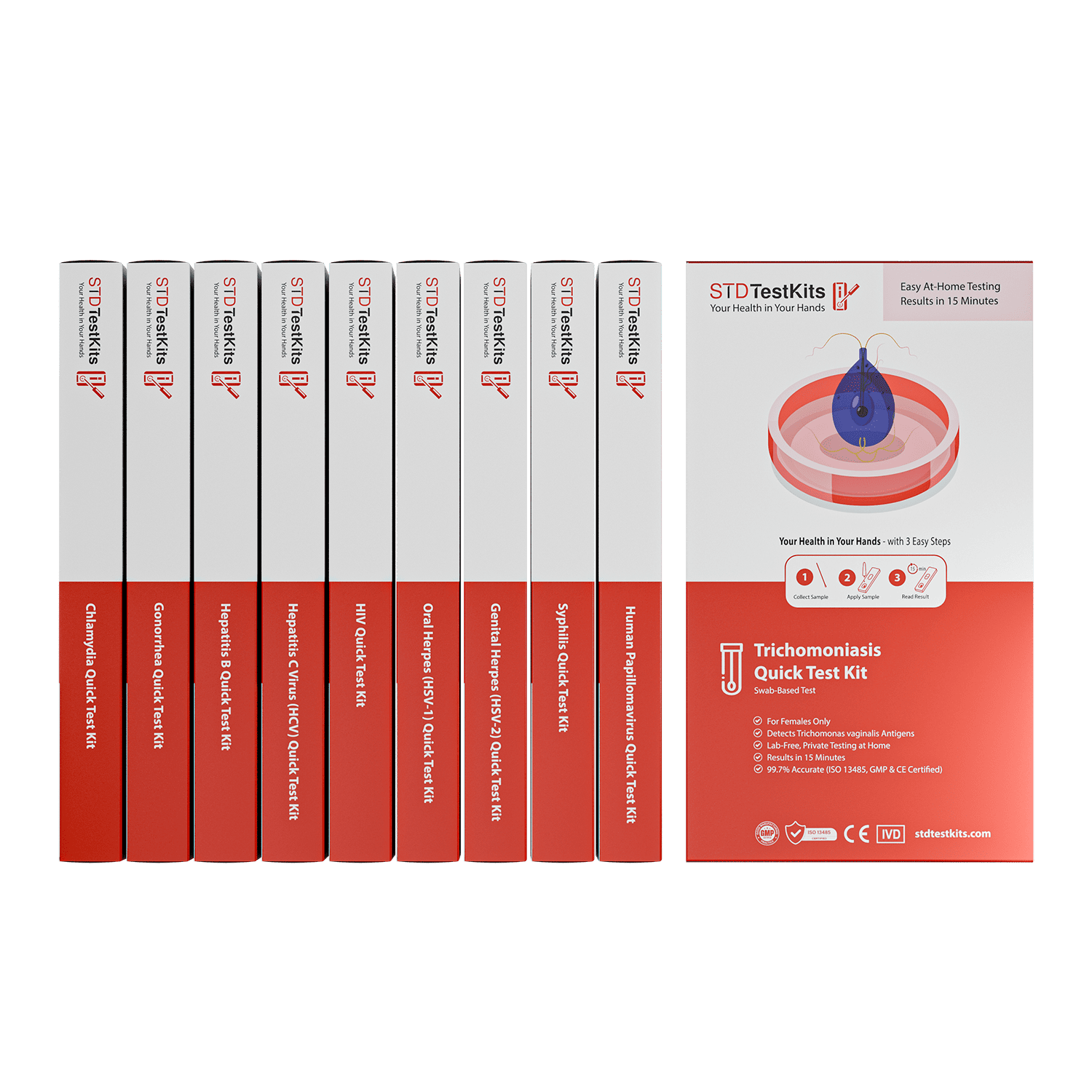
Red flags include sharp pelvic pain, green or frothy discharge, lesions, bleeding after sex, or symptoms that worsen quickly. At that point, testing isn’t optional, it’s necessary. You can use an at‑home kit like the ones offered on STD Rapid Test Kits if you want privacy and fast results, especially when uncertainty feels emotionally heavy. Probiotics can support you after treatment, but they aren't a substitute for diagnosis.
Even if you're dealing with stubborn symptoms that don’t rise to emergency levels, getting clarity helps. Once you know what you’re dealing with, probiotics can play their role more clearly, whether that’s restoration after antibiotics, maintenance between cycles, or ongoing support to prevent recurrent flare-ups.
How to Choose a Probiotic That Actually Works
Forget the branding. Forget the pastel packaging and buzzwords like “feminine wellness” or “pH harmony.” What matters most is the strain, the dose, and whether the bacteria can survive the journey to your vagina. Look for clinical-grade strains like GR-1, RC-14, and in some cases L. crispatus. Aim for at least 1 billion CFUs, though higher amounts aren’t always better; consistency matters more than potency. And always check whether a product is third-party tested, because supplements aren’t regulated with the same rigor as medications.
The delivery system also matters. If you’re choosing oral probiotics, opt for delayed‑release capsules that protect bacteria from stomach acid. If you’re choosing vaginal suppositories, make sure they’re designed for that use; inserting a gut probiotic capsule vaginally is unsafe, ineffective, and potentially irritating.Don't trust products that hide behind pretty labels and vague promises. Instead, trust ones that are clear about what they do, what strains they use, and how they test them.
If you want to feel more at ease during this process, think about combining the use of probiotics with a testing plan. The Combo STD Home Test Kit is one option that lets you test yourself at home without anyone knowing. This is especially helpful if your symptoms are similar to those of common STDs. Your probiotics can do their job better once you get rid of the things that aren't working.
FAQs
1. Can probiotics really fix BV?
They can help, especially after antibiotics, but they're not magic pills. If you're dealing with that classic fishy smell and thin discharge, you'll probably need a prescription first. Once that's handled, though, a probiotic with GR-1 and RC-14 can absolutely help your vagina bounce back and stay balanced. Think of it as cleanup crew after the firefight.
2. Is it okay to use probiotics during STD treatment?
Yes, and in fact, it's a smart move. Antibiotics kill the bad stuff, but also your good bacteria. A vaginal probiotic during or right after treatment can help stop the spiral of BV or yeast that sometimes follows. Just don’t expect it to treat the STD itself. That’s not what probiotics do. They’re support, not soldiers.
3. How long before I feel anything?
Be patient. This isn’t Plan B, it’s more like therapy. Most people notice changes after 2–4 weeks of daily use. Sometimes it’s subtle, like discharge normalizing or irritation fading. If you're expecting overnight results, you’ll be disappointed. But give your vagina time to rebuild, and you might be surprised by how steady things feel after a month.
4. Can probiotics help with yeast infections?
Not as a solo act. If you're already mid-infection, hello, cottage cheese discharge and fire-level itching, you'll likely need antifungal treatment first. But probiotics can help prevent recurrences or that weird in-between state where you’re not sure if it’s yeast or just a cranky microbiome.
5. What if probiotics make things worse?
It happens. Some people get more discharge or bloating in the first week, it’s usually just your body adjusting. But if the discharge smells foul, turns green, or comes with pain or burning, stop and get tested. That’s not detox. That’s your vagina waving a red flag.
6. Should I refrigerate my probiotics?
Only if the label says so. Most modern vaginal probiotics are shelf-stable thanks to freeze-drying. The real issue isn’t your fridge, it’s how the supplement was shipped and stored. If it sat in a delivery truck all day in August heat, those cultures might be toast before you ever open the bottle.
7. Do probiotics make your vagina smell better?
Short answer: yes, sometimes. A healthy microbiome helps maintain that low, clean pH that naturally suppresses odor. But smell is complex, it can be hormonal, bacterial, or totally normal for you. Probiotics won’t make you smell like roses, but they can help reduce that “something’s off” scent you might get after sex or your period.
8. Can I take probiotics with birth control?
Absolutely. Probiotics don’t mess with hormones, and they’re not absorbed into the bloodstream in a way that would interfere with your pill, patch, or IUD. If anything, they might actually help offset some of the flora shifts that come with hormonal contraception.
9. What if I’m using a probiotic and still feel off?
Trust your instincts. If your symptoms linger or get worse, especially if you’ve got pain, strong odor, or unusual discharge, it’s time to test. Don’t fall into the trap of throwing supplements at an untreated infection. Rule out STDs, yeast, and BV first. Then let probiotics do their thing without playing defense.
10. Are probiotics safe to use long term?
Yes, especially the ones made for vaginal use. If you’re someone who gets BV after every round of antibiotics or yeast infections after every weekend trip with a partner, long-term probiotics might be your new BFF. Think of them as maintenance for your vaginal ecosystem, not a one-time rescue mission.
You Deserve Answers, Not Assumptions
It's not just about not getting infections; it's also about being comfortable in your own body. And when something doesn't feel right, the last thing you want is vague advice or someone who doesn't understand how unsettling it is to wonder all day if your discharge is normal, if your partner's chemistry messed things up, or if that last round of antibiotics did more harm than good.
That’s where probiotics come in, not as a cure-all, but as part of a bigger picture. When chosen right, they help reset the balance, rebuild what's been disrupted, and support a body that’s been through enough already. Whether you’re healing after an STD, navigating recurring BV, or just want to feel a little more in sync, you deserve more than assumptions. You deserve clarity.
And if you’re not sure what’s going on yet? You don’t have to guess. This discreet combo STD test kit checks for the most common infections, all from home. Knowing what you’re working with is the first step toward healing that lasts.
How We Sourced This Article: We pulled together real science, from clinical studies to trusted health orgs, to make sure everything here is clear, useful, and actually applies to your body, not just a lab chart.
Sources
1. CDC: Sexually Transmitted Infections Overview
2. Office on Women’s Health: Vaginal Yeast Infections
3. WHO: STI Guidance and Resources
4. The role of probiotics in vaginal health
5. Vulvovaginal Candidiasis – STI Treatment Guidelines
6. Which Works Better for BV: Oral or Vaginal Probiotics?
7. Yeast infection (vaginal) – Diagnosis and Treatment (Mayo Clinic)
8. The Role of Probiotics in the Treatment of Vulvovaginal Candidiasis
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who blends clinical precision with sex-positive, trauma-informed education. His work focuses on making sexual health accessible, clear, and stigma-free for readers everywhere.
Reviewed by: Dr. L. Rhodes, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.