How Long After Exposure Can Chlamydia Be Detected?
Quick Answer: Retest for chlamydia about 3 months after treatment, even if you have no symptoms. If you still have symptoms after treatment, wait at least 3 weeks before testing again to avoid false positives.
Why This Article Matters (and Who It’s For)
This isn’t just a clinical protocol breakdown, it’s a lifeline for the confused, the panicked, and the people who followed all the rules but still found themselves staring down a second positive result. Maybe you’re in a monogamous relationship and can’t understand how it came back. Maybe your partner never took their meds. Or maybe you did everything right… and still ended up retesting too soon.
Whether you tested at a clinic, used an at-home STD kit, or got antibiotics from urgent care, you’re not alone. This article is for anyone navigating the awkward gray zone after treatment, unsure when to test again, how to tell a partner, or what a second result even means. And yes, we’ll cover how to prevent the endless reinfection loop no one talks about.

People are also reading: When Travel Turns Risky: How Soon You Should Test After Sex Abroad
Can Chlamydia Come Back After Treatment?
Medically? No, once treated correctly with a full course of antibiotics, the original chlamydia infection is gone. But practically? Yes, because most cases of “it came back” are actually cases of reinfection, not resistance. This happens when a sexual partner hasn’t been treated, or when someone is re-exposed before the body has fully cleared the infection.
Even more confusing: if you test too soon after antibiotics, you might still have chlamydia DNA in your body, even though you’re no longer contagious. That leftover genetic material can trigger a false positive on a highly sensitive test like NAAT (nucleic acid amplification test).
Here’s the real talk: Yes, chlamydia can “come back”, but usually because someone gave it back to you. That’s why retesting isn’t optional. It’s protection.
Why Retesting After Chlamydia Matters
Retesting after a chlamydia infection isn’t just a checkbox, it's the only way to know if you’re truly clear or if you’ve been reinfected. The CDC recommends everyone who’s tested positive for chlamydia retest approximately three months after treatment, even if they feel fine.
Here’s why that matters:
Table 1. Why retesting isn’t optional, it’s essential.
Retesting also helps break the ping-pong effect: when partners pass the infection back and forth unknowingly. You could both be taking turns treating and reinfecting each other without realizing it. And yes, it happens in committed, monogamous couples too.
How Long After Treatment Should You Retest?
Timing is everything. Test too early, and you could get a false positive. Wait too long, and you could miss a silent reinfection. Here’s how to think about retesting windows:
If you're asymptomatic and completed treatment:
- Retest at 3 months, even if you feel fine.
- If you're at high risk (new partners, untreated partner, previous infection), consider retesting every 3–6 months.
If you still have symptoms after treatment:
- Wait at least 3 weeks before retesting to avoid false positives.
- If symptoms persist after that, consult a provider, it could be another infection or something else entirely.
If your partner didn’t get treated, or you’re unsure, they should be tested and treated immediately. Otherwise, you’re both trapped in a feedback loop.
If you're ready to retest discreetly, order a chlamydia test kit here. Results in minutes, no clinic visit needed.
What If It’s Still Positive? Real Stories, Real Scenarios
Sabrina, 23, thought she was in the clear. She took her antibiotics, waited a week, and got back to life as usual. But something still didn’t feel right, sex was uncomfortable, and there was a new discharge. Her follow-up test came back positive. Her first reaction: “Did the meds not work?” But what actually happened? Her boyfriend hadn’t finished his prescription.
Reinfection isn’t always about cheating. Sometimes it’s about miscommunication, delayed treatment, or partners not realizing they need meds too. Other times, it’s about testing too soon. NAAT tests are so sensitive they can pick up leftover DNA fragments from a dead infection for up to 3 weeks. This isn’t a failed treatment, it’s a biological echo.
Now imagine Jordan, 31, who took antibiotics after a casual partner tested positive. He never had symptoms but wanted to be safe. A month later, he retested, still positive. In his case? It wasn’t reinfection or resistance. It was a mail-in test taken too early and misinterpreted. His doctor explained: “If you’re symptom-free, wait at least 21 days. Earlier than that, we can’t be sure what the test is picking up.”
How to Avoid a False Positive After Chlamydia Treatment
If your chlamydia test is still positive weeks after treatment, it doesn’t always mean you’re still infected. Here's what might be going on:
Table 2. Why your test might be positive even after treatment.
To avoid confusion, plan your retest with these tips:
- Wait at least 21 days post-treatment before retesting, unless advised otherwise by a provider.
- Make sure all partners are treated simultaneously.
- Use a reliable home test with clear instructions, or visit a clinic if symptoms worsen.
Partner Didn't Get Treated? Here's What Happens
If your partner didn’t take medication, or wasn’t told they needed to, your infection cycle hasn’t actually ended. You can pass chlamydia back and forth without symptoms, without realizing it, and without “doing anything wrong.” This isn’t about blame. It’s about biology.
The CDC recommends treating all recent sexual partners from the past 60 days, regardless of symptoms. And yes, even oral sex counts, chlamydia can live in the throat. If you’re not sure how to tell a partner or are worried about awkward conversations, there are anonymous partner notification tools available online. Some clinics even offer free scripts and anonymous text options.
If you’re unsure whether your partner completed treatment or you’re afraid to ask, the safest move is to avoid sex until both of you have tested negative, after treatment and the recommended wait period.
Want to avoid the retesting rollercoaster? This combo STD test kit lets you and your partner test at the same time, from home.
People are also reading: Too Soon to Test? The Hepatitis B Window Period Explained
How to Prevent Reinfection, Even in Long-Term Relationships
It’s a painful truth: even committed couples can get trapped in a reinfection loop. That doesn’t mean someone cheated. It could mean:
- One person never took their antibiotics
- Sex resumed too soon after treatment
- Chlamydia was present in the throat, but only the genitals were treated/tested
Prevention isn’t about paranoia. It’s about setting each other up for success. Here’s what helps:
- Wait 7 days after both partners complete treatment before having sex again
- Use condoms until both test negative after the 3-week window
- Consider full STD panels if you’ve never tested together before
Reinfection isn’t a relationship failure, it’s a fixable communication gap. The best prevention is shared action: both of you testing, treating, and retesting. That’s not awkward. That’s love.
If you're unsure what kit to use or how long to wait, check out the STD Test Kits homepage for discreet tools and personalized test options.
The Emotional Toll of Retesting (And Why You’re Not Overreacting)
Let’s be honest, retesting for chlamydia isn’t just about labs and timelines. It’s about anxiety, doubt, and that sick feeling in your stomach when you realize: “I might not be done with this.” You did the right thing. You got treated. But here you are, again, wondering if your body betrayed you… or if someone else did.
This emotional spiral is common, and completely valid. Many people feel ashamed when they have to retest, as if needing a second check means they failed. It doesn’t. It means you’re protecting yourself and others. In fact, people who don’t retest are more likely to spread infection without knowing it.
One Reddit user wrote, “I tested positive again after being with one person for six months. We both cried. But it turned out he didn’t take all the meds, he thought one dose was enough.” Stories like this aren’t rare. They’re reality. And they show why retesting is an act of care, not an admission of guilt.
What If You Test Positive Again?
Step one: breathe. Then reframe. A second positive doesn’t mean antibiotics failed. It means something didn’t finish the cycle, whether that was a partner’s treatment, your body’s clearance timeline, or a missed exposure. Reinfection is frustrating, but it’s also fixable.
Here’s what to do:
- Wait at least 3 weeks post-treatment before retesting to avoid false positives.
- If positive after 3 weeks and you’re sure treatment was followed, consult a provider to assess reinfection risk.
- Test all recent partners. This step is often skipped and leads to repeat exposure.
- Ask for a second antibiotic course only under medical guidance, don’t self-treat repeatedly.
And emotionally? Give yourself some grace. Plenty of people test positive again. It doesn’t make you careless or dirty. It makes you human, and human bodies are messy.
What to Expect With At-Home Retesting Kits
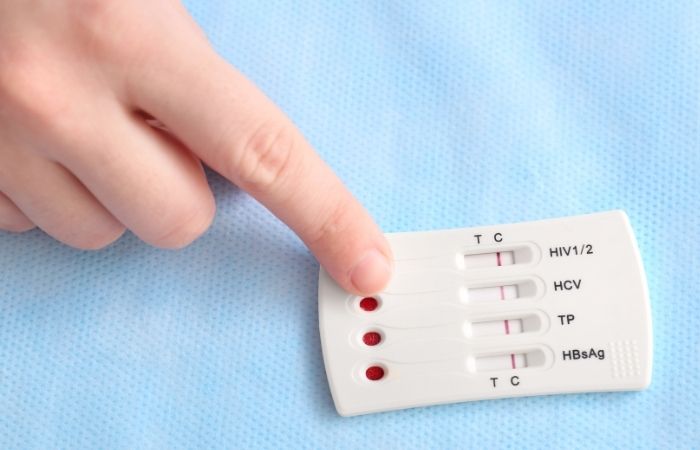
If the idea of returning to a clinic makes your skin crawl, or if you're managing this privately, at-home testing might be the best route. Modern chlamydia home tests use either urine samples or genital swabs and deliver results in as little as 10 minutes (rapid lateral flow) or 2–5 days (mail-in lab kits).
Here’s what people love about at-home retesting:
- Discreet packaging, nothing says “STD test” on the label
- No scheduling, no waiting rooms
- Results delivered directly to your inbox or seen on the test strip
Shipping usually takes 1–3 days, and many kits are eligible for FSA/HSA coverage. You’ll want to read instructions closely to avoid sample issues, especially for mail-in kits that require refrigeration or timing buffers.
If you’re feeling stuck, this chlamydia test kit offers step-by-step guidance and support, even if it’s not your first round.
Shipping, Privacy, and Testing While Off-Grid
Yes, you can still retest even if you live rural, travel frequently, or share space with roommates or family. At-home STD tests like those from STD Rapid Test Kits come in plain mailers, no branding, no awkward logos, and no one knows what’s inside unless you tell them.
For people living off-grid or with limited internet, it’s smart to order a backup test kit ahead of time. You don’t need a pharmacy, a doctor’s appointment, or insurance. And because many reinfections happen quietly, having a test on hand makes proactive care easier and less stressful.
Some kits come with 24/7 support chat or telehealth referrals if your result is positive again. That way, you’re not alone, and you can make a plan fast without waiting for an in-person appointment.
If this all sounds like what you need, the 7-in-1 Complete At-Home STD Test Kit includes chlamydia, gonorrhea, syphilis, and HIV, and it ships discreetly, fast.
FAQs
1. Can chlamydia come back even if I took the antibiotics?
Unfortunately, yes, but it’s not because the meds didn’t work. The most common reason people test positive again is reinfection from a partner who wasn’t treated or didn’t finish their meds. Chlamydia doesn’t magically “reactivate,” but it can show up again if the loop isn’t fully closed. That’s why treating your partner and waiting the full 7 days before sex really matters.
2. How long should I wait before retesting for chlamydia?
Best practice? Wait at least 3 weeks after finishing antibiotics if you still have symptoms. That gives your body time to clear out the dead bacteria and prevents a false positive. If you’re symptom-free, the CDC recommends a follow-up test at around 3 months. Think of it as a double-check, not a punishment.
3. I still feel weird “down there.” Does that mean I wasn’t cured?
Not necessarily. Some people feel irritation, discharge, or just “off” for a week or two after treatment. It could be inflammation, another infection like BV or a yeast imbalance, or just your body healing. But if things don’t feel right after 2–3 weeks, don’t guess, retest.
4. What if I tested positive, but my partner didn’t?
Tricky, but it happens. Maybe they tested too early, used the wrong sample type, or the infection is living somewhere it wasn’t tested (yes, chlamydia can hide in the throat or rectum). Or maybe, someone caught it between partners. This is where honest conversations and full-panel testing come in handy.
5. Can I really test for chlamydia at home and trust the result?
You can, and many people do. Today’s FDA-cleared home kits are incredibly reliable when used correctly. You pee in a cup or swab your genitals, mail it in or get instant results, and skip the awkward clinic chat. Just follow the instructions like a recipe and you’re good to go.
6. Is it weird to ask my partner to test again too?
Nope, it’s actually hot. Caring about each other’s health is a green flag. You can say something like, “I’m planning to retest just to be safe. Want to do it together?” You’d be surprised how many people feel relieved someone brought it up first.
7. Can I get chlamydia from oral sex?
Yes, though it’s less common. Chlamydia can infect the throat, and people often don’t realize they’re carrying it there because it usually has zero symptoms. That’s why some tests miss it, if your partner only tested genitally, they could still be passing it along orally without knowing.
8. Do I need to retest if I don’t have any symptoms?
Yes. Most chlamydia cases, especially in people with vaginas, come with zero symptoms. You might feel totally fine and still be contagious. That’s why the 3-month retest is so important. It’s not about being paranoid, it’s about being safe and staying clear for good.
9. Will insurance cover at-home retesting?
Sometimes! Some FSA and HSA plans cover it, and a few testing services offer reimbursement forms. But even if it’s out-of-pocket, many kits are cheaper than urgent care, and you get to keep your dignity in sweatpants.
10. I’m scared to tell a past hookup I had chlamydia. Do I have to?
It’s hard, we get it. But yes, if you were sexually active in the last 60 days, those partners should be told. The good news? You don’t have to do it face to face. There are anonymous texting services and partner notification tools online that make it way easier. It’s not about shame, it’s about care.
Get The Results You Need
Retaking a chlamydia test does not mean you did something wrong; it means you’re doing something right. You’re being informed, taking control, and putting an end to the silent cycle of reinfection. It might be your first time, your second, your third, but however you look at it, healing isn’t linear; it’s layered.
Don’t let confusion or shame stop you from getting clarity. This discreet combo test kit checks for the most common STDs and helps you move forward, with or without symptoms, and with total privacy.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Planned Parenthood – Chlamydia Overview
2. Retesting After Treatment to Detect Repeat Infections – CDC
3. Sexually Transmitted Diseases: Diagnosis & Retesting – Mayo Clinic
4. Chlamydia Test & Reinfection Retesting – MedlinePlus
5. Chlamydial Infections Screening and Retesting Guidance – CDC
About the Author
Dr. F. David, MD, is a board-certified infectious disease specialist who specializes in the prevention, diagnosis, and treatment of STIs. He is an expert at balancing accuracy and no-nonsense advice with a sex-positive attitude and is dedicated to making his information accessible to readers in urban and off-grid environments alike.
Reviewed by: L. Monroe, RN, MPH | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.







