How Soon After Sex Can I Test for Gonorrhea?
Quick Answer: The best time to test for syphilis is 6 to 12 weeks after potential exposure. Testing before 3 weeks often leads to false negatives. If you test early, retesting is strongly recommended.
This Is for You If You’re Waiting, Wondering, or Worried
Maybe the condom broke. Maybe there was no condom at all. Maybe you found out your partner wasn’t exclusive after all. Or maybe you were tested last week and still can’t shake the feeling something’s wrong. If any of that sounds familiar, this guide is for you.
Testing for syphilis isn’t just a clinical step, it’s emotional. People who search for “when to test for syphilis after exposure” are often in a waiting game with their own thoughts. You might not feel sick. You might feel fine. But you also might feel scared, ashamed, angry, or just exhausted from thinking about it. And here’s what matters: all of that is normal.
We wrote this for the people in limbo. For the ones refreshing clinic hours, the ones hiding symptoms from partners, the ones who don’t have symptoms at all but can’t sleep until they know. We’ll break down exactly when syphilis shows up, why early tests fail, and how to time your testing for the most accurate, useful results. Because testing is care, not confession.

People are also reading: You’re on PrEP. Do You Still Need to Worry About STDs?
What Kind of Test Are We Even Talking About?
When we talk about testing for syphilis, we’re usually talking about blood tests. These come in two flavors: treponemal and non-treponemal. Some tests look for antibodies your body creates in response to the infection, while others look for direct signs of the bacteria itself. Most at-home or rapid syphilis tests detect antibodies, which takes time. Your body doesn’t produce them instantly.
Let’s say you had a possible exposure yesterday and want peace of mind today. A rapid fingerstick test might sound like a good idea, but here’s the truth: even if you’re infected, your body probably hasn’t produced enough antibodies yet to show up on that test. That means you could test negative and still have syphilis. That’s not fearmongering, it’s just biology.
Mail-in lab kits use more sensitive assays, but they still depend on your immune response. Clinic tests, including RPR and VDRL, also rely on this timeline. That’s why no matter how you test, at home, by mail, or at a clinic, the question isn’t just which test you use, but when you use it.
The Window Period: Where False Negatives Lurk
This is where everyone tends to slip up. The "window period" is the time from the time that you were exposed to syphilis until the time that a test will be able to identify it. While in this window, the infection can continue to quietly spread even as your test remains negative.
The syphilis bacterium, Treponema pallidum, also starts reproducing quickly after it infects your body, either through mucous membranes or skin. But it also takes time for the immune system to respond. The vast majority of antibody-based tests will not reliably detect syphilis until at least 3 weeks after exposure. And the slightly-more-reliable time period? About 6 weeks. The highest detection rate usually occurs between 6 and 12 weeks.
Figure 1. Syphilis testing accuracy across the window period.
Here’s the bottom line: if you test during week 1 or 2, even the best rapid test could miss the infection. That doesn’t mean you’re in the clear. It just means your body hasn’t caught up yet.
Real Talk: What Happens When You Test Too Soon
Let’s say you had unprotected sex five days ago. You’re anxious. You want answers. You take a rapid syphilis test on day six, it’s negative. So you breathe a little. You go back to your routine.
But then, around day 15, you notice something. A small sore, maybe a little crusty. No pain, so you ignore it. Then a rash starts to appear, on your hands, maybe your chest. It doesn’t itch. You Google. And now you’re spiraling, because everything you read says syphilis.
This is a common arc. Early testing gives false reassurance, and people stop paying attention until symptoms become undeniable. One Reddit user shared, “I tested at a clinic a week after a risky hookup. Came back negative. Three weeks later, I got this weird rash and thought it was detergent. Surprise, it was syphilis.”
Even clinicians see this play out. According to the CDC’s syphilis treatment guidelines, early-stage syphilis is often missed when testing is done before antibody levels rise. That’s why retesting is built into most protocols. A negative result too early isn’t a diagnosis, it’s a placeholder.
This isn’t your fault. It’s the way the infection works. The solution? Understand the timing, and retest when it matters. You deserve accuracy, not just fast results.
What Exposure Scenarios Really Look Like (And Why Timing Changes Everything)
Let’s stop pretending every sexual encounter happens under perfect, controllable circumstances. People get drunk. Condoms get forgotten. Feelings get complicated. Exposure isn’t always as clear-cut as a checklist, and the confusion that follows is exactly what makes timing so difficult to navigate.
Take Joel, 26. He hooked up with someone he met at a queer bar while traveling through New Orleans. It was a one-night thing. There was oral, there was some light rimming, and they didn’t use a condom. Joel got back home two days later and felt that pit in his stomach. He ordered a test online, overnight shipping, and tested himself on day four. Negative. Then he relaxed.
Three weeks later, Joel started to notice a painless ulcer near his anus. He thought it was a hemorrhoid. By the time he got to a clinic, nearly six weeks post-exposure, the doctor took one look and ordered syphilis serology. Positive. His earlier test hadn’t failed, he’d just used it too soon.
Now contrast that with Aubrey, 33. She’s in a long-term relationship but had an unexpected encounter with an ex during a business trip. The guilt hit fast, and so did the panic. She tested at a clinic six days later, again, negative. But she didn’t feel convinced. So she waited. She retested at five weeks, and that’s when the results came back positive. Aubrey’s story isn’t uncommon. It’s what happens when people try to do the right thing, but don’t have the right information about when tests actually work.
Here’s what these stories tell us: exposure scenarios matter. Whether it was a one-time thing or a recurring partner, oral or vaginal, with or without protection, each detail affects risk, but none eliminate it entirely. And none change the fact that testing too soon is a gamble.
Choosing a Test: Rapid vs Mail-In vs Clinic
All testing isn’t created equal. The method you choose can dramatically affect not just your results, but your peace of mind. What works best depends on what you value most, speed, accuracy, privacy, or emotional clarity. Let’s unpack the differences.
At-home rapid tests give results in minutes. You prick your finger, place a drop of blood on a cassette, wait. For many, this is a lifeline. Privacy, control, no awkward questions. But here’s the catch: the earlier you test, the more likely the result is unreliable. Rapid tests rely on your body producing detectable antibodies, which doesn’t always happen in the first few weeks.
Mail-in kits use lab-grade equipment. You collect your sample, usually blood, and ship it to a certified lab. Turnaround is typically 2 to 5 days. These tests are more sensitive and may detect lower antibody levels than rapid kits, but timing is still everything. Testing in week one or two? Still risky for a false negative.
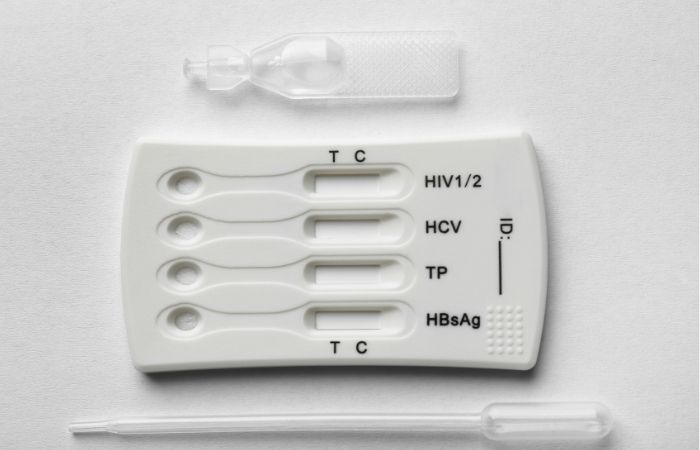
Clinic tests come with professional interpretation. You can get non-treponemal tests like RPR (Rapid Plasma Reagin) or VDRL (Venereal Disease Research Laboratory) that check for active infection, as well as confirmatory treponemal tests. These are highly reliable, once your immune system has had time to respond. But they also come with downsides: scheduling, exposure, judgment, cost. For some, just walking into a clinic feels like a confession. That’s why at-home options are growing in popularity, especially among people managing stigma, privacy, or limited access to care.
Figure 2. Testing methods compared by user needs and infection timeline.
Regardless of method, the golden rule applies: test after your body has had time to respond. If you need to test sooner, for peace of mind, or because you’re symptomatic, just know you may need to test again. And that’s okay.
Peace of Mind vs Premature Reassurance
Let’s be honest. Sometimes people test not because they expect a positive, but because they’re trying to feel better. That’s human. But it can backfire. Testing at five days might calm your nerves temporarily, but it can also lead to risky decisions based on inaccurate results.
This is where testing becomes psychological. You might think, “My test was negative, so I’m fine.” But what you really did was test an invisible stage of syphilis. You didn’t confirm absence, you confirmed that you were still too early to tell. And that nuance is easy to miss when you're stressed or scared.
If your head keeps spinning, peace of mind is one test away, but only if it’s the right one, at the right time. You can order a discreet syphilis test kit here, but consider using it after the three-week mark. That’s when results start to mean something.
Still unsure? Start with a combo kit that screens for multiple STDs at once, including syphilis, HIV, chlamydia, and gonorrhea. Sometimes the exposure risk isn’t just one infection, it’s overlapping ones. Comprehensive kits reduce the guesswork.
What If You’re Asymptomatic?
This is the hardest part: most people with syphilis have no symptoms during the early stages. No sore, no rash, no flu-like warning signs. That’s what makes timing the test so critical. You can’t rely on your body to tell you when something’s wrong. By the time symptoms appear, or don't, the infection may have already advanced.
Roughly 15–30% of early syphilis infections are asymptomatic or so mild they go unnoticed. That doesn’t mean they’re harmless. Untreated, syphilis can progress to more serious stages, affecting the brain, heart, and nervous system. The fact that you feel fine isn’t proof you’re in the clear. It’s just more reason to time your test right and repeat it if needed.
People are also reading: The STDs That Can Lead to Cancer
Why Retesting Isn’t Overkill, It’s Smart
Here’s the truth most websites won’t tell you: one syphilis test isn’t always enough. That doesn’t mean the test was bad or that you messed up. It means infection doesn’t follow your calendar. Your body’s timeline matters more than your anxiety’s, and that’s hard to accept when you just want to know you’re safe.
Let’s rewind to Derrick, 41. He tested negative two weeks after a hookup with someone who later mentioned they had “a weird rash.” At first, Derrick brushed it off. He’d tested. He was in the clear. But something didn’t sit right. He retested at six weeks, positive. That second test didn’t contradict the first. It clarified it. His body needed time, and the first test simply couldn’t catch the antibodies yet.
Whether you tested early by accident or by necessity, retesting is how you close the loop. The CDC recommends retesting in any of the following situations:
1. You tested within the first 3 weeks after exposure 2. Your partner tested positive 3. You start developing symptoms 4. You have multiple partners or ongoing exposure 5. You’re pregnant or immunocompromised
And even if none of these apply, here’s the bottom line: if you’re still anxious, you can always test again. It’s not obsessive. It’s responsible.
Figure 3. Syphilis retesting windows based on initial test timing.
This kind of roadmap can help you breathe. Instead of endlessly Googling “how accurate is a syphilis test at 10 days,” you’ll know: test again at six weeks. That clarity is a form of self-care.
What If the Results Don’t Match Your Body?
This is where it gets tricky. You test negative. But you don’t feel okay. Maybe you’re exhausted all the time. Maybe there’s a rash that’s not itchy but it’s definitely weird. Maybe a sore appeared and disappeared so fast you weren’t sure it was even there. This is the space where false reassurance and real infection overlap.
The phrase “syphilis is the great imitator” exists for a reason. Early symptoms mimic everything from shaving irritation to eczema to mild allergies. Some people never get a noticeable sore. Others get one in places they can't see, like inside the mouth, anus, or under the foreskin. If your symptoms feel out of place, and your gut says something’s off, it’s worth retesting.
And let’s not forget the impact of being immunosuppressed. If you’re living with HIV, undergoing chemo, or on immune-modulating meds, your antibody response may take longer. That means your window period stretches. A test that works for someone else at 3 weeks might not work for you until week 6 or later. Retesting isn’t overthinking. It’s personalizing your care.
What About Your Partner(s)?
This part is uncomfortable, but it matters. If someone you were with tests positive, even if you tested negative, you need to act. This isn’t just about exposure math. It’s about bacterial transmission, which doesn’t wait for paperwork. Testing positive doesn’t mean someone “cheated” or did something wrong, it means they need care, and so do you.
If you’ve already tested once and your partner later tests positive, schedule another test immediately and then again at the six-week mark. That two-step process ensures you’re not relying on a false early negative. And if you’re not in contact with that person anymore, assume the worst-case window: test at 6–12 weeks to cover your bases.
It’s also okay to ask new or current partners to test. You’re allowed to protect your body without feeling paranoid. The rise in syphilis cases globally, especially among people in their 20s and 30s, has made partner testing more common, and less taboo. And when it comes to disclosure? You’re not alone. There are anonymous partner notification services, scripts, and clinics trained to help you through that process.
When Symptoms Appear Late, or Not at All
Let’s say three months pass. No sore. No rash. You’ve convinced yourself you’re fine. But then, at month four, you develop an odd patch of hair loss or a rash that shows up on your palms and soles. That’s classic secondary syphilis. And it doesn’t always arrive on schedule.
Just because you didn’t see early symptoms doesn’t mean you were never infected. That’s why every clinic, every guideline, every expert recommends: don’t trust just one test, especially if it was early. Time is a key diagnostic tool in STDs. And the longer you wait to treat syphilis, the more serious the consequences become.
Untreated, syphilis can lead to complications involving the heart, brain, eyes, and more. Neurosyphilis, which can occur at almost any stage, can cause confusion, vision problems, and memory loss. The goal here is not to scare, it’s to explain why early testing isn’t always better. It’s not about reacting fast. It’s about acting right.
And if you're still not sure what your timeline looks like? Grab a calendar. Mark the day of exposure. Count forward 21 days. That’s your first viable testing point. Count again to 6 weeks. That’s your best one. And if that result still leaves you wondering, test once more at 12 weeks. That's your final check-in. You deserve certainty.
What If You Test Positive?
Take a breath. Seriously. Testing positive for syphilis might feel like your world is spinning, but the truth is, you’ve just taken the first step toward getting better. Syphilis is one of the most treatable STDs out there. Most cases are cured with a single dose of penicillin. You read that right: one shot. And just like that, you’re no longer infectious, and your body starts healing.
The hard part isn’t the medicine, it’s the emotional fallout. Shame, fear, panic, even anger. It’s okay if you feel all of that. But don’t get stuck there. Focus on what you can control: treatment, retesting (if your provider recommends it), and telling anyone who might need to know. If you’re not ready for face-to-face conversations, there are anonymous notification tools that help you share results safely and respectfully.
One reader told us:
“I sat in my car after the result came in. I almost didn’t open the email. But when I saw it, I realized, I can fix this. And I did.”
That’s the energy we want for you. Fear is natural. But action is powerful.
Privacy, Shipping, and Support That Doesn’t Judge
When you’re navigating a possible STD exposure, even walking into a clinic can feel exposing. That’s why many people are turning to at-home testing: not just for convenience, but for emotional protection. No waiting rooms. No awkward conversations. Just a plain envelope, arriving at your door, with everything you need inside.
STD Test Kits ships in discreet packaging, no logos, no product names, and offers both single tests and multi-panel kits. Most orders arrive within 2–3 business days, and many are available with overnight options. When you’re in a spiral of worry, speed matters. But so does sensitivity. That’s why every kit comes with clear instructions and online support if you get stuck.
And if you test positive? No automated scolding. Just straightforward advice, links to treatment resources, and the option to test again if you need peace of mind. Because testing should feel like a step forward, not a scarlet letter.
People are also reading: Everything You’re Afraid to Ask About At-Home STD Tests
FAQs
1. Can I test for syphilis the day after a hookup?
You can, technically, but don’t expect it to tell you much. Most tests won’t catch syphilis that early, because your body hasn’t built up enough of a response yet. Think of it like showing up to a crime scene before the clues even exist. You’ll just get a false sense of security. Better to wait until at least 3 weeks post-exposure if you want results you can trust.
2. What if I tested negative but still feel weird?
Trust your gut, but also trust biology. If you tested within the first two weeks, that result might not mean what you think it does. Syphilis can simmer silently before it shows up on a test. So yeah, you might feel off, and that might be anxiety, or it might be your immune system catching up. Retest at the 6-week mark. That’s where most answers finally come into focus.
3. Does syphilis always come with symptoms?
Nope. That’s the trick. A lot of people never get the classic sore, or they miss it because it shows up in places you don’t exactly inspect daily, like inside the mouth, anus, or under foreskin. Others confuse it with a pimple, a cut, or an ingrown hair. So no symptoms doesn’t mean no infection. That’s why testing is so important, even if everything looks “normal.”
4. My partner tested positive but I tested negative. Who's right?
Probably both of you. If you tested before your body had time to react, your test might just be early, not wrong. The smart move? Test again in a few weeks. Infection doesn’t always hit both people the same way at the same time. And if there was any skin-to-skin contact, you’re not off the hook. Retesting keeps things honest.
5. Is it possible to cure syphilis completely?
Yes, thankfully. A single shot of penicillin is all most people need, especially in the early stages. It’s not like herpes or HIV that sticks around. Once treated, it’s gone. But timing is everything. The earlier you catch it, the easier it is to cure before it causes deeper damage. So don’t sit on it hoping it’ll go away. It won’t, but it will respond to treatment.
6. Should I retest even if my first result was negative?
If your first test was within 3 weeks of the encounter? Absolutely, yes. That’s like checking the oven before the cake has risen, it’s premature. Retest at 6–12 weeks for the most reliable answer. And if you’re still worried after that, one last test at the 3-month mark will give you peace of mind.
7. Does syphilis spread through oral sex?
Yes. And not just “maybe” yes, definitely yes. Syphilis sores can appear in or around the mouth, genitals, or anus. And you don’t have to see them for transmission to happen. Even a single unprotected oral encounter can lead to exposure. That’s why mouth-to-genital contact still counts when you’re calculating risk.
8. Can I test for syphilis at home without anyone knowing?
Totally. That’s the whole point of discreet testing. You can order a kit online, test in your bathroom, and get results without ever stepping into a clinic. No waiting rooms. No sideways glances. Just you, your test, and an answer. If privacy’s your priority, this is the move.
9. I’m pregnant. Should I test for syphilis?
Yes, and most OB providers will test you automatically in early pregnancy. But if you had any new exposure or a risky partner, you should test again in the third trimester. Syphilis can pass to the baby during pregnancy, but if caught early, it’s treatable and preventable. No shame here, just protection for both of you.
10. I feel embarrassed even thinking about getting tested. Am I overreacting?
Not even close. You’re reacting like a person who cares about their health, and maybe someone else’s too. There’s nothing embarrassing about wanting answers. In fact, it’s one of the most responsible things you can do. Testing isn’t a confession. It’s a decision. One you control, one that can change everything.
You Deserve Answers, Not Assumptions
If there’s one takeaway from all of this, it’s this: the timing of your syphilis test matters more than the test itself. Testing too early might feel proactive, but it can give you answers that aren’t real. And you deserve real answers.
Whether you’re dealing with silence, symptoms, or suspicion, you don’t have to figure it out alone. At-home tests exist for a reason. So does retesting. So do second opinions. You are not overre
How We Sourced This Article: We combined current guidance from leading public health organizations, peer-reviewed medical research, and real-world patient experiences to make this guide as accurate, honest, and emotionally grounded as possible. In total, over 15 reputable sources informed this article. Below, you’ll find six that were especially useful in answering the most common questions about syphilis testing windows, false negatives, and exposure risk.
Sources
1. CDC Laboratory Recommendations for Syphilis Testing, United States
2. Symptoms and staging of syphilis (PMC article)
3. Treponema – Medical Microbiology (incubation period 10-90 days)
4. Syphilis: Clinical, Epidemiologic, and Biologic Review (PMC)
5. Mayo Clinic — Syphilis: Diagnosis & Treatment
6. A practical approach to the diagnosis and management of STIs (PMC)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Renée Halston, MPH | Last medically reviewed: October 2025
This article is for informational purposes and does not replace medical advice.






