The Hidden History of HIV Testing in the U.S., From Fear to Fingerpricks
Quick Answer: Certain STDs, including HPV, Hepatitis B and C, and possibly HIV, can lead to cancer if left untreated. Most of these infections show few or no symptoms before they begin causing cellular damage. Regular testing and vaccination can significantly reduce risk.
HPV and Cancer: The Virus You May Already Have
Let’s start with the most common and the most misunderstood: HPV, or human papillomavirus. Nearly 80% of sexually active people will contract some strain of HPV in their lifetime. Most clear the virus naturally within two years. But some strains, especially HPV types 16 and 18, don’t go away. They dig in. And over time, they can trigger abnormal cell growth that leads to cervical, anal, throat, penile, and vulvar cancers.
Here’s what makes HPV dangerous: it’s usually invisible. You can carry high-risk strains for years without a single symptom. No warts. No discharge. No clue. You might only find out after an abnormal Pap result, a high-risk HPV screening, or worse, after early cancer signs appear.
Nia, 31, found out during a fertility consult. “I’d never missed a Pap, but I’d never had an HPV test either,” she said.
“Suddenly, I’m being told I have precancerous cells, possibly from a strain I got in my early twenties. I had no idea. My boyfriend at the time didn’t either.”
It’s not just women at risk. Men, trans individuals, and nonbinary people can carry, and spread, HPV without symptoms. The virus can infect the throat during oral sex, leading to oropharyngeal cancer years later. It can also affect the anus, especially in men who have sex with men, or anyone with receptive anal exposure.
And while cervical cancer is the most well-known consequence, it’s far from the only one. The rise in HPV-related head and neck cancers, particularly in people under 50, is a warning sign that the virus isn’t confined to the reproductive system.

People are also reading: How Long Before Chlamydia Affects Fertility? A Breakdown by Stage
HPV-Related Cancers: Where and How They Form
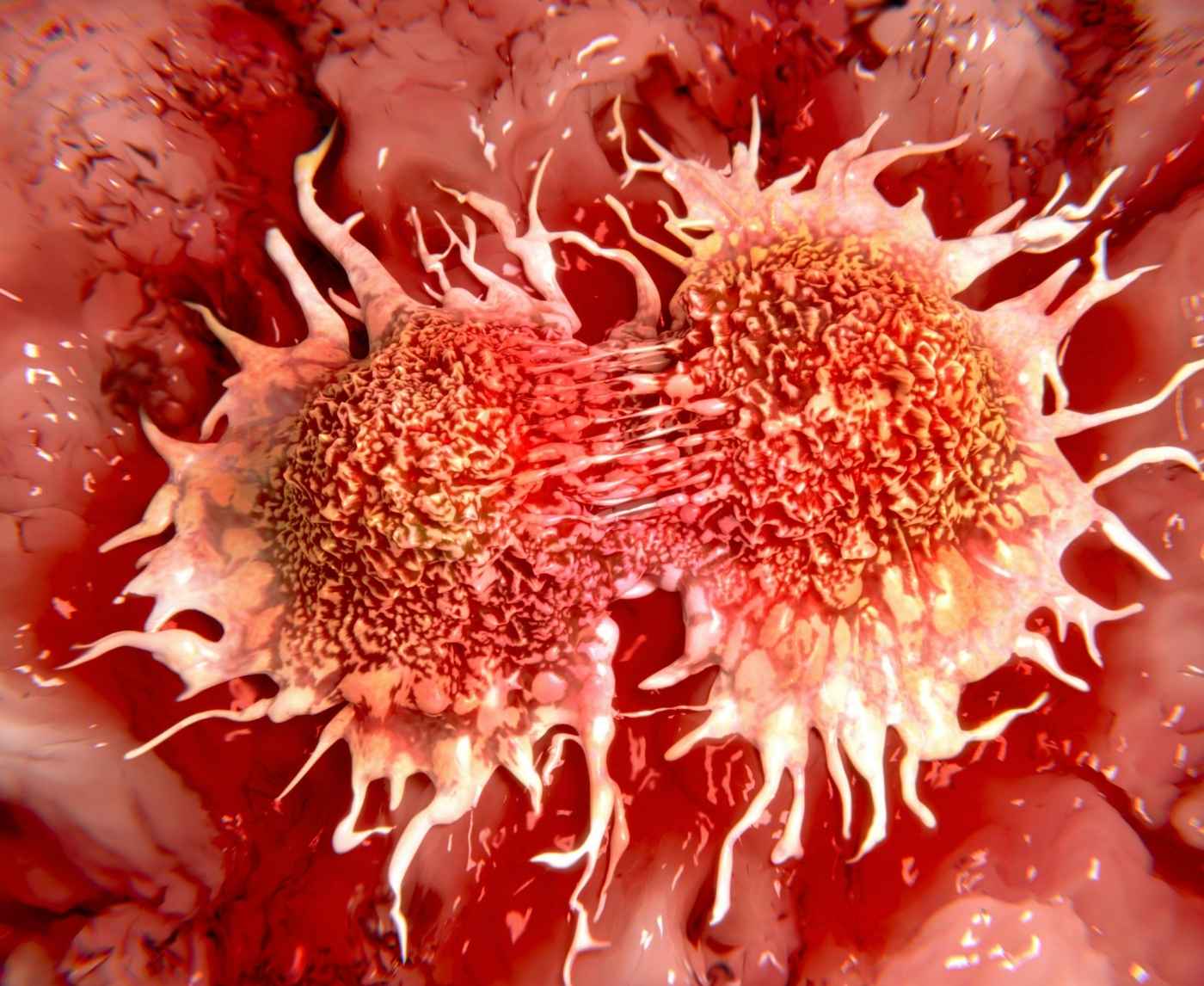
Cancer from HPV doesn’t happen overnight. It begins with cellular changes in the affected tissue, usually in the cervix, anus, or throat. These changes often go undetected unless you’re being screened. Over years, persistent infection can trigger mutations in the cells’ DNA. And that’s when the transformation from virus to cancer begins.
The chart below outlines the primary cancers linked to HPV and how they typically develop:
Table 1: Common cancers linked to persistent HPV infection. Symptoms often appear late, making routine screening and vaccination essential for prevention.
Most of these cancers are preventable, HPV vaccination is highly effective against the most dangerous strains. But millions of adults missed that window, especially if they were over 26 before the vaccine became widely available. And for them, testing and surveillance are the next best defense.
In the U.S., Pap smears and HPV co-testing remain the gold standard for cervical screening. But for people with other anatomy, testing options are limited. Oral and anal HPV screenings are not routine, leaving entire populations at risk and unaware.
Hepatitis and Liver Cancer: When STDs Become a Long Game
If HPV is the stealthy virus that hijacks your cells, then Hepatitis B and Hepatitis C are the slow-burners, the chronic STDs that can simmer inside the body for decades before turning lethal. And while not everyone realizes it, both are sexually transmitted. Both can lead to liver cancer. And both often give you no warning signs until your liver function is already compromised.
Dennis, 42, was diagnosed with Hepatitis C during a life insurance medical exam.
“I didn’t drink. I didn’t use drugs. I didn’t feel sick,” he said. “But I’d had unprotected sex in my twenties and a piercing I never got tested after.”
By the time they found it, he already had elevated liver enzymes and signs of scarring, damage that may have started 15 years earlier.
Most people think of hepatitis as something you catch from needles or transfusions, but that’s only part of the story. Hepatitis B is easily transmitted through sex, especially if condoms aren’t used. It’s 50 to 100 times more infectious than HIV. Hepatitis C is less likely to spread through sex, but it’s still possible, especially in men who have sex with men, or if there are open sores or coinfections involved. Once chronic, both viruses set off cycles of inflammation, fibrosis, and cellular mutation. And that’s when liver cancer enters the picture.
How Liver Cancer Develops From Chronic STD Infections
It doesn’t happen quickly. For many people with chronic hepatitis, it takes 10, 20, even 30 years for the virus to trigger cancer. But that’s also what makes it so insidious. You may go decades without any symptoms. No jaundice. No fatigue. Just a virus hiding in your liver, slowly reshaping your future.
The table below shows how the hepatitis-cancer connection typically unfolds over time:
Table 2: The long-term progression from hepatitis to liver cancer. Many people live symptom-free for years before any signs emerge.
In the U.S. alone, around 3 million people are living with chronic Hepatitis C, and most don’t know it. Many were infected decades ago and only find out when applying for insurance, donating blood, or being evaluated for an unrelated condition. The link between untreated hepatitis and hepatocellular carcinoma, the most common form of liver cancer, is now well established. And it’s preventable with early detection.
Unlike HPV, which currently lacks a broad testing protocol for non-cervical cancers, hepatitis B and C can be easily tested with a simple blood panel. And for Hepatitis B, there’s a safe, effective vaccine, one that many adults never received as kids.
Still, hepatitis rarely gets the same public attention as HPV or HIV. It’s often overlooked, stigmatized, or written off as a “lifestyle” infection. But the liver doesn’t care about stigma. It cares about viral load, inflammation, and time. And left unchecked, chronic hepatitis can quietly rob a person of their vitality long before cancer is even diagnosed.
The Symptom Myth: Why Cancer-Causing STDs Often Feel Like Nothing
This is where most people get caught off guard. We’re trained to look for red flags, pain, discharge, sores, swelling. But the STDs that cause cancer are often the quiet ones. HPV, Hepatitis B, and Hepatitis C rarely cause any symptoms early on. That’s not bad luck, it’s biology. These viruses aren’t trying to make you sick right away. They’re designed to linger.
By the time you do feel something? It’s often because cellular damage has already occurred. Cervical cancer, liver cancer, throat cancer, these don’t form overnight. They develop slowly, silently, over years of inflammation and mutation. That’s why early testing is everything. And why the absence of symptoms isn’t a green light to skip your screens.
It’s also why so many diagnoses come with guilt. People assume they must have ignored something. But in reality, they didn’t. These infections are built to hide. And they do it well, until the consequences can no longer be ignored.

People are also reading: How to Read Your At‑Home STD Test (And When to Trust the Result)v
HIV and Cancer: The Risks You Might Not Realize
When people think of HIV, they often think of immune suppression, not cancer. But the two are deeply connected. HIV doesn’t directly cause cancer, but it weakens your immune system’s ability to fight off other viruses that do. And that opens the door to multiple cancer types, especially if HIV goes untreated or is diagnosed late.
Marlon, 38, first tested positive for HIV after a severe chest infection sent him to the ER. He’d skipped testing for years, assuming his risk was low.
“I thought I was safe,” he said. “I used condoms most of the time, I felt fine, I didn’t look sick.”
But by the time he was diagnosed, his CD4 count had dropped below 200. Within the year, he developed Kaposi sarcoma, a rare cancer linked to a virus that healthy immune systems usually suppress.
HIV increases the risk of several cancers, some classified as “AIDS-defining” and others more subtle. Many of these are triggered by viruses like HPV, Epstein-Barr, or HHV-8, which can quietly live in the body until the immune system is too weak to control them. That’s why early HIV treatment (ART) is so essential, not just for health, but for cancer prevention.
Which STDs Are Most Linked to Cancer?
Let's take a step back for a second. You should now understand how STDs can cause different types of cancer depending on the virus, the body part, and the immune system's response. But how do the risks stack up? And which infections are most likely to cause serious problems?
This table shows the most well-studied links between common STDs and types of cancer. Not every infection causes cancer, but it does show where science has found strong links:
Table 3: STD and cancer associations, with relative risks and prevention strategies. Only some of these viruses have vaccines, making testing even more critical.
It’s worth repeating: cancer is never a guaranteed outcome of an STD. But when infections are left unchecked, especially for years, they create the kind of cellular stress and DNA damage that cancer thrives on. The goal isn’t to panic, it’s to test early, treat fast, and stay in control of your health journey.
Don’t Wait for Symptoms, Here’s When to Test
If you’ve had unprotected sex, multiple partners, or even one partner with an unknown status, it’s time to test. Not because something’s definitely wrong, but because so many of these infections feel like nothing until they’ve already done damage. And when it comes to cancer prevention, early is always better than late.
- For HPV: If you’re over 25 and have a cervix, ask about HPV co-testing with your next Pap. If you don’t have a cervix but have had oral or anal exposure, talk to your provider about whether screening is possible based on your risk.
- For hepatitis: One-time testing is recommended for most adults, especially if you were born between 1945–1965, or have any risk history including sex with someone who has hepatitis. For Hepatitis B, the vaccine is safe, effective, and a powerful cancer-prevention tool.
- For HIV: The CDC recommends at least one lifetime test for all adults, and more frequent testing for anyone with ongoing risk. And remember, an undetectable viral load not only protects you from cancer risks, it protects your partners too.
If you’re unsure where to start, a combo STD test kit can cover the most common infections in one discreet delivery. You don’t need to wait for a scare, a symptom, or someone else to bring it up. Testing is your right. Testing is your power move.
FAQs
1. Can an STD really cause cancer, or is that just internet drama?
It’s real, no drama needed. Some STDs, especially viruses like HPV and hepatitis B/C, can cause cellular changes that slowly lead to cancer over time. Think of it like this: it’s not the STD throwing a punch, it’s setting off a chain reaction in your cells that, years later, can turn serious. Silent doesn’t mean safe.
2. I had HPV years ago. Should I still be worried now?
Depends. Most people clear HPV naturally, but some high-risk strains like HPV 16 or 18 can hang out for years, no symptoms, no warning, still quietly affecting your cells. If you’ve never had follow-up testing or a Pap smear, now’s a good time. Don’t let the silence fool you. Just because it’s quiet doesn’t mean it’s gone.
3. Does HIV cause cancer, or just make you more vulnerable?
More the second one. HIV doesn’t cause cancer directly, it weakens your immune system. And when your immune defenses drop, other viruses (like HPV or HHV-8) can go rogue and start causing damage that leads to cancer. That’s why getting on HIV treatment early protects more than just your T-cells, it protects your future.
4. Why don’t I feel anything if these infections are so dangerous?
That’s the trick. These are slow operators, not smash-and-grab thieves. HPV and hepatitis aren’t trying to wreck you overnight. They hide. They settle in. They mess with your cells from the inside, quietly. So yeah, you can feel 100% fine while a virus is changing your DNA in the background. Welcome to the wild world of viral stealth.
5. I’m a guy. Do I even need to worry about HPV?
You do. Big time. HPV isn’t just a women’s health issue. It causes anal, throat, and penile cancers in men, and here’s the kicker: there’s no approved routine test for it in guys. Which means prevention and vaccination are your best moves. Don’t let outdated messaging put you at risk.
6. How long does it take for an STD to turn into cancer?
We’re talking years, sometimes decades. HPV-related cancers can take 5 to 15 years to show up. Hepatitis and liver cancer? Try 20 to 30. But the catch is, once you start feeling symptoms, things are often already far along. That’s why testing early, when you feel totally fine, is actually the smart move.
7. Is herpes one of the cancer-causing STDs too?
Not officially. HSV (herpes) isn’t classified as a cancer-causing virus, but there’s some research suggesting it might amplify the risk if you’ve also got HPV. On its own, herpes isn’t known to lead to cancer, but it still deserves attention and regular check-ins.
8. I already got the HPV vaccine, am I bulletproof?
Not quite bulletproof, but you’re wearing some of the best armor out there. The vaccine covers the worst strains, especially the ones most likely to cause cancer. But it doesn’t block every single one. Think of it like a seatbelt, it won’t stop every crash, but it could save your life.
9. Can I get tested for all this from home?
Yes, and it’s way easier than you’d think. A good combo STD test kit can check for HIV, hepatitis, and sometimes HPV, depending on your anatomy. It’s discreet, fast, and skips the awkward waiting room stare-downs. No excuses needed.
10. I haven’t had symptoms, like... ever. Should I still test?
Yes. Especially for the silent ones. The STDs that lead to cancer are usually the ones that play quiet for years. No itching, no discharge, no pain, and still working damage in the background. Testing isn’t about panic. It’s about knowing what’s going on in your body before something else tells you the hard way.
What You Can’t See Can Still Change Everything
The hardest part about cancer-causing STDs is how invisible they are, at first. No fever, no rash, no obvious wound. Just a quiet, molecular shift. A virus slipping into your cells. A bacteria sparking inflammation. The slow unraveling of something that once felt safe, normal, fine. Until one day, it’s not.
But knowing that truth doesn't mean giving in to fear. It means doing what our past selves maybe didn’t have the tools, education, or access to do. It means testing before symptoms. Vaccinating before exposure. Asking questions even when we feel fine. Because most of the people who end up with STD-related cancers didn’t do anything “wrong.” They just didn’t know what was hiding under the surface.
That can change, starting right now. You don’t need to wait for symptoms or wait to feel “ready.” You just need to choose clarity. Choose knowledge. Choose you.
Take back control of your health story today.
How We Sourced This Article: We used more than a dozen expert sources to make this guide. These included peer-reviewed medical journals, national health guidelines, and interviews with patients who have cancer that is related to STDs. We put accuracy, trauma-informed clarity, and relevance at the top of our list.
Sources
1. National Cancer Institute – HPV and Cancer
2. Basic Information about HPV and Cancer | CDC
3. Cancers Caused by HPV | CDC
4. STIs and Cancer | American Sexual Health Association
5. Viruses That Can Lead to Cancer | American Cancer Society
6. HPV and Cancer — National Cancer Institute
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Janelle Tran, PA-C | Last medically reviewed: September 2025
This article is for informational purposes and does not replace medical advice.