How Soon After Sex Can I Test for Gonorrhea?
Quick Answer: STD test results are usually accurate when timed correctly, but false negatives can happen, especially if you test too early, don’t test for the right infections, or rely on lower-sensitivity methods. If you have symptoms, consider retesting.
Who This Is For (And Why It Matters)
This article is for the people who got tested and still feel stuck in a cycle of second-guessing. Maybe you’re in a new relationship and want peace of mind before you go further. Maybe you’re dealing with symptoms that don’t add up. Maybe you’re afraid of the answer and relieved it came back negative, but also not convinced it’s the truth.
For a lot of us, sex doesn’t come with clarity, it comes with questions. And when testing becomes part of that, it’s not just about biology. It's about trust. Trust in your body. Trust in your partners. Trust in the system that told you you're clean. And when that trust is shaken, it can feel just as stressful as getting a positive result.
This guide breaks down when to trust your STD results, when not to, and what steps to take if your instincts, or your symptoms, tell a different story.

People are also reading: Mouth Sores, White Patches, or Nothing? What Oral HPV Really Looks Like
How STD Tests Actually Work (And Why They Can Miss Things)
Let’s get one thing straight: most modern STD tests are accurate, but not infallible. Whether you’re using a rapid test at home or doing a full panel at a clinic, accuracy depends on several factors: the type of infection, how long it’s been since exposure, what kind of test is used, and whether symptoms are present.
For example, according to CDC guidelines, NAATs (nucleic acid amplification tests) are considered the gold standard for detecting chlamydia and gonorrhea. But even those can give false negatives if you test within a few days of exposure. Antibody-based blood tests for syphilis or HIV take time for the body to mount a detectable response, weeks, sometimes months.
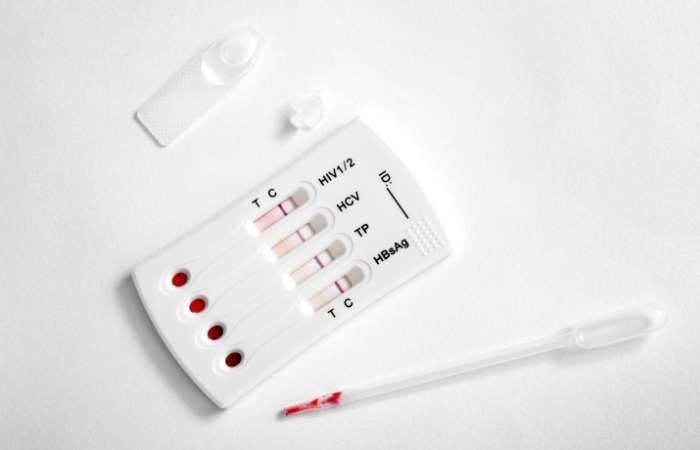
Then there’s the test scope itself. Some panels don’t include Trichomoniasis. Others don’t check for HPV or Mycoplasma genitalium. So even if your results say “negative,” they might not be testing for what’s actually causing your symptoms.
You can order a discreet, broad-spectrum kit through STD Test Kits. It's one way to fill the gap if your last test didn’t check for everything.
Understanding Window Periods (And Why Early Testing Can Backfire)
Here’s where most false negatives happen: timing. The window period is the time between exposure to an STD and when it can reliably show up on a test. If you test during this window, especially within the first few days after a sexual encounter, you might get a “clean” result even though the infection is already incubating in your body.
This doesn’t mean testing early is useless, it just means you might need to retest. And understanding the window period can help you figure out whether your negative result is trustworthy or premature.
Figure 1: Window period ranges by infection. Testing too soon can lead to false reassurance. Retesting after the optimal window improves reliability.
Rapid Tests vs Lab Tests: What the Accuracy Numbers Really Mean
Some people test twice for a reason: not all STD tests are the same. It's okay to still feel unsure if you used a rapid test at home. Rapid tests are made to be quick and easy to use, but that can mean they aren't as sensitive, especially if they are used outside of the ideal window period or when there are no symptoms.
Let's take it apart. Rapid tests look for either antigens or antibodies, depending on the type of infection. These markers need to be present in a detectable amount, which might not happen right away. Tests like NAAT or PCR look for the pathogen's DNA or RNA. These are much more sensitive, especially when it comes to infections like chlamydia, gonorrhea, and trichomoniasis.
Figure 2: STD test accuracy trade-offs. While rapid tests offer convenience, NAATs and PCRs remain the clinical gold standard for detection sensitivity.
“It Came Back Negative… But I Still Don’t Feel Right”
Darius, 29, took a rapid chlamydia test after a weekend with a new partner. The result was negative, but a week later, the discomfort while urinating hadn’t gone away. He retested with a mail-in kit that used a NAAT method, and this time, it was positive.
“I almost didn’t retest. I kept telling myself I was just overthinking it. But something told me to try again. Thank God I did.”
Stories like this are common. False negatives don’t mean the test is broken, they usually mean the timing or test type didn’t match the infection’s progression. And if your body is still talking to you, you should listen.
There are other explanations too. Not all symptoms are STD-related. Irritation from condoms, bacterial vaginosis, allergic reactions to lube, or even stress-induced inflammation can mimic STD symptoms. But the only way to know for sure is to rule out the most likely causes, which means retesting smart, not just repeating the same method.
People are also reading: Can You Get Reinfected If Your Partner Isn’t Treated? Yes.
What Tests Don’t Always Cover (And What They Miss)
Most people think a “full panel” means they’re being tested for everything. But unless you’re reading the fine print, you might be missing out on key infections. Many standard panels exclude:
- Trichomoniasis – A common but often overlooked infection
- HPV – Not included unless you're doing a cervical swab or anal test
- Mycoplasma genitalium – Requires specific NAAT testing
- Oral or rectal infections – Most urine tests don’t catch these
So even if you tested negative for the “big four” (chlamydia, gonorrhea, syphilis, HIV), you could still be carrying or reacting to something not covered in that panel. If you’re testing at home, check the label. If you went to a clinic, ask exactly what was tested. Don’t assume. Ask.
Want to test for multiple STDs with a single kit? This combo test kit covers the most common infections and is ideal for follow-up clarity.
Why Retesting Might Be the Most Honest Thing You Can Do
There’s no shame in not trusting your first result. Retesting isn’t about being paranoid, it’s about protecting your health and the people you care about. In fact, many health professionals recommend routine retesting 3 to 6 months after new sexual partnerships, or 2 to 4 weeks after treatment to confirm clearance.
If you tested negative but still feel symptoms, are within the window period, or discovered your test didn’t cover certain STDs, retesting makes sense. And it’s not just about you, it’s about giving your partners accurate information too.
Explore our at-home testing options for discreet, private, and lab-accurate follow-up testing. Your body deserves to be heard.
When Negative Results Hurt More Than a Diagnosis
For some, a negative test result is a relief. For others, it’s just the beginning of a different kind of stress, the kind that says, “If I’m clean, why do I still feel broken?” The answer isn’t always physical. False negatives can make you question your body, your instincts, even your sanity. And if a healthcare provider brushes you off because “the tests are clear,” it can feel like gaslighting.
This is especially true for people with vaginas, queer folks, and people of color, communities that often face medical dismissal. When your symptoms don’t match your results and no one believes you, that silence can feel heavier than any diagnosis.
Testing is a tool. It’s not a verdict. And if your results don’t explain what you’re going through, you deserve more answers, not more silence.
“I Tested Negative for Everything. It Still Burned When I Peed.”
Nina, 25, tested negative for chlamydia, gonorrhea, and trichomoniasis after experiencing burning during urination and pelvic discomfort. Her doctor told her it was likely a yeast infection or stress. A week later, the pain had worsened. She finally found a provider who ran a test for Mycoplasma genitalium, a bacterial STI that’s not on most standard panels. It came back positive.
“I felt like I was losing my mind. Everyone kept saying it was in my head because the test was negative. But I knew something wasn’t right. I had to fight to get tested for what wasn’t included.”
Stories like Nina’s reveal a bigger problem: not all tests are created equal, and not all providers dig deep enough. You are allowed to ask for more. More testing. More explanation. More clarity.
If you've ruled out the basics and still feel symptoms, request or order broader testing. Kits that include trichomoniasis, Mycoplasma genitalium, and oral/rectal swab options can uncover what standard panels miss. Explore a broader combo kit here if you’re retesting or want to be sure.
What If It’s Not an STD?
Negative results don’t always mean you’re imagining things. Sometimes, they mean you’re dealing with something other than an STD, but still very real. The list of conditions that mimic STD symptoms is long, including:
- Bacterial Vaginosis (BV) – causes discharge and odor, not an STD but common post-sex
- Urinary Tract Infections (UTIs) – especially after new partners or rough sex
- Yeast Infections – itching, redness, and thick discharge
- Allergic reactions – to latex, lubes, condoms, or hygiene products
- Hormonal changes – ovulation, menopause, or starting new birth control
Each of these can cause symptoms that feel identical to common STDs. And sometimes, they show up with an STD. That’s why it’s so critical to get a full clinical picture, not just a result page. If your provider dismisses you after a negative test, seek another opinion.
If Your Partner Tested Negative Too, But You’re Still Unsure
This happens more often than people admit: two partners get tested, both come back negative, and yet one still has symptoms. It can create tension. Suspicion. Even guilt. But biology isn’t moral. Sometimes, one partner’s infection doesn’t show up yet. Or only one test covered the right site (e.g., throat vs genital). Or the strain is dormant in one person but active in another.
Don’t let results alone dictate trust or intimacy. Use them as part of a bigger conversation. Ask: what did you test for? How long after exposure? Was it a rapid test or a lab kit? Did it include throat and rectal swabs if applicable?
If either of you feels unsure, retesting doesn’t mean mistrust. It means care. Choose a comprehensive kit that tests both of you together, and opens the door for clearer, safer communication.
FAQs
1. Can STD tests actually be wrong?
They can. Especially if you test too soon after exposure, or if the test you took wasn’t sensitive enough. Think of it like trying to catch a whisper in a loud room, if the infection hasn’t had time to build up in your system, the test might miss it. That’s not you being dramatic. That’s just how biology works.
2. Why do I still have symptoms if I tested negative?
Because symptoms don’t lie, but tests sometimes miss things. Maybe you tested during the window period. Maybe your test didn’t include the infection you actually have. Or maybe it’s something non-STD like a UTI or yeast imbalance. Bottom line: your body deserves to be believed, not brushed off.
3. Which STD tests are the most accurate?
Lab-based NAATs and PCR tests are the gold standard. If you're testing for chlamydia, gonorrhea, or trichomoniasis, this is what you want. They're the microscopic bloodhounds of the testing world, way better than guessing based on symptoms or hoping a rapid test picks it up in time.
4. Can at-home tests give me a false negative?
Yes, but so can clinic tests if used too early. The key is timing and method. Rapid at-home tests are great for a quick check, but if you’re feeling off or recently exposed, a mail-in lab kit is a smarter play. Especially for infections like HIV or syphilis that need more time to show up.
5. Should I retest even if my partner was negative too?
If something doesn’t feel right, yes. One or both of you might’ve tested too early, or not for the right STDs. And here’s the awkward truth: not all “negative” tests mean the same thing unless you both used the same method, panel, and timing. Retesting doesn’t mean mistrust, it means respect.
6. Do all tests cover the same infections?
Definitely not. Many panels skip trichomoniasis, Mycoplasma genitalium, or oral/rectal infections unless you ask. Some don’t include HPV or herpes unless you already have symptoms. Always check the fine print. The word “comprehensive” doesn’t always mean what it should.
7. What’s the window period, again?
There's a window between the time an infection takes place and when it can be successfully and consistently detected with a test. Think of it as your immune system's loading screen. If you test too early, you could miss it. The exact window differs for each infection and type of test, but for most common STDs, testing 2–3 weeks after exposure will yield more accurate results.
8. I used a condom, why would I still need to test?
Because condoms lower risk, not eliminate it. They don’t cover everything. Skin-to-skin STDs like herpes and HPV can still spread from areas not covered by latex. And condoms can slip or tear. Testing is smart, even when you play it safe.
9. How often should I get tested if I’m sexually active?
If you’ve got new or multiple partners, every 3 to 6 months is a good rule. More often if you’ve had a recent exposure, symptoms, or share sex toys. Testing doesn’t mean you’re risky, it means you’re responsible.
10. Can other conditions feel like an STD?
Absolutely. BV, yeast infections, allergic reactions, even friction from sex toys or rough play can all cause itching, discharge, or irritation. But here’s the kicker: they can also show up at the same time as an STD. That’s why assuming can backfire, testing is the only way to sort it out with confidence.
You Know Your Body. Don’t Let a Slip of Paper Tell You Otherwise
If you’ve made it this far, chances are you’re not just curious, you’re worried. Maybe confused. Maybe frustrated. You did the responsible thing: you got tested. But the truth is, testing isn’t always black and white. And when something still feels off, you deserve clarity, not dismissal.
It's not crazy to want to retest. It is strong. It's not too much to wait for the right time, pick a more accurate method, or choose a wider panel. It's just being careful. For you. For your partners. To make you feel better.
Don't wait and wonder; get the answers you need. This at-home combo test kit checks quickly and discreetly checks for the most common STDs.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. CDC – 2021 Sexually Transmitted Infections Treatment Guidelines
2. Mayo Clinic – STD Testing: What to Expect
3. CDC Sexually Transmitted Infections Treatment Guidelines — 2021
4. HIV Testing — Window Periods and What Tests Measure (CDC)
5. Urine Tests vs. Genital Swabs for STI Detection — UAB Study (2023)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to stop, diagnose, and treat STIs. He combines clinical accuracy with a straightforward, sex-positive approach and is dedicated to making it easier for readers to find what they need, whether they live in a city or off the grid.
Reviewed by: T. Ramos, NP | Last medically reviewed: December 2025