Think It’s Just Irritation? These Chlamydia Symptoms Say Otherwise
Quick Answer: Yes, you can get chlamydia without vaginal or anal sex. It spreads through oral sex, shared toys, and even genital-to-genital contact. Testing matters, even if you think you played it safe.
Why This Still Happens: The Gap Between Sex-Ed and Real Life
Most teens and young adults have been taught that sex = penetration. But that outdated idea misses how real people hook up. Oral sex, mutual masturbation, rubbing, and experimenting with toys all happen, and chlamydia can spread through any of it. The bacteria lives in bodily fluids, which means skin-to-skin and mouth-to-genital contact are all possible routes.
According to the CDC, chlamydia is one of the most common STDs among people under 25, and most people who have it don’t know it. That includes people with no symptoms and people who’ve never had “real sex.” The risk is real even when the act doesn’t “count” by old-school definitions.

People are also reading: What the New Mpox Cases Say About STI Stigma and Vaccine Access in 2026
Oral Sex Can Spread Chlamydia, Here’s How
Oral sex might feel safer than penetration, but it’s not risk-free. If someone has chlamydia in their genitals, the bacteria can travel to your throat through contact with semen, vaginal fluids, or infected skin. Likewise, if someone has an untreated throat infection, they can pass it to your genitals during oral-to-genital contact.
That’s what happened to Julián. His hookup didn’t seem sick, but oral chlamydia rarely shows symptoms. In some cases, it can feel like strep: a sore throat, mild redness, maybe swollen glands. But often, it’s invisible. And if it goes untreated, it can linger in the throat for weeks or even months, spreading silently.
Studies like this one from PubMed show that oral chlamydia is common in young populations and often missed, especially in people assigned female at birth or those who don't receive throat swabs during testing. That means people who think they’re STI-negative could still be carrying, and passing, the infection.
What About Hands, Toys, and Skin Contact?
It sounds wild, but yes, chlamydia has been documented to pass through shared sex toys, unwashed hands, and skin-to-skin genital rubbing (“dry humping” or outercourse). The odds are lower than with penetrative sex, but if there's genital fluid and contact, there’s risk. Here’s how it breaks down:
Figure 1. Common non-penetrative acts and their chlamydia transmission risks.
“But I’m a Virgin”, Why That Doesn’t Mean You’re Risk-Free
Many people infected with chlamydia still consider themselves virgins. And by some definitions, they are, especially if they haven’t had vaginal or anal sex. But the bacteria doesn’t care about definitions. It only needs contact, fluid, and a pathway to your body. Even one unprotected oral encounter can lead to infection.
This is especially common among LGBTQ+ teens, who often avoid clinics out of fear or shame and who may not be asked about nontraditional sex acts by doctors. A study published in 2018 showed that many young men who have sex with men were infected with chlamydia in the throat or rectum despite reporting no recent penetrative intercourse.
That’s why comprehensive testing matters, and why throat swabs should be part of the conversation if oral sex is on the table. You don’t need to have “real sex” to get a real infection.
How to Know If It’s Oral Chlamydia, or Something Else
Oral chlamydia can feel like a sore throat that just won’t quit. But here’s the problem: it often mimics other conditions, like strep, allergies, or even dry air. That’s why so many people miss it, or assume it’s nothing serious. Unlike genital chlamydia, which can cause discharge or burning, throat infections often stay under the radar.
So how do you tell the difference? You can’t, just by feeling it. Some symptoms that might point toward oral chlamydia include:
Figure 2. Overlapping symptoms of oral chlamydia and other common throat conditions.
Because symptoms overlap so much, the only way to know for sure is to test. That’s where at-home testing comes in, especially when you want privacy, speed, and control. If your sore throat feels “off,” or if you've had oral sex without protection, it’s time to check.
Testing for Chlamydia When You Haven’t Had “Real” Sex
Many people think you can’t get tested unless you’ve had vaginal or anal sex. That’s completely false. Testing isn’t about what you’ve done, it’s about what could have exposed you. If there’s been mouth-genital contact, shared toys, or hands involved, testing is valid.
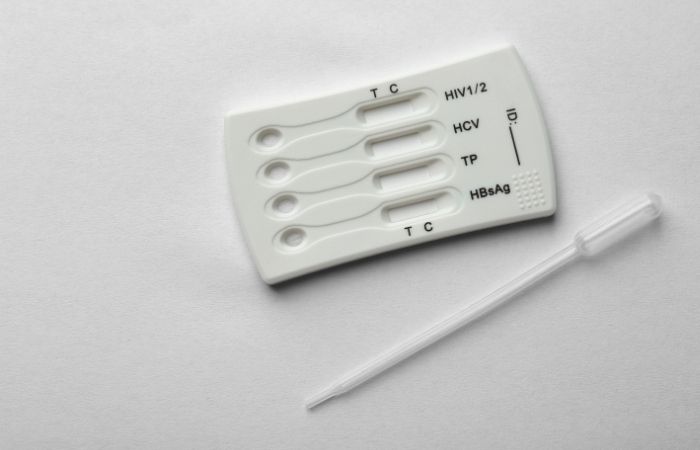
Home test kits can now detect chlamydia through throat, genital, or rectal samples. You don’t need a clinic visit to get answers. Some tests only use urine, which won’t catch oral infections, so if you’re worried about oral sex, make sure your test includes a throat swab.
You can order a private kit online, collect your sample at home, and ship it to a lab. Or, for faster peace of mind, you can use a rapid chlamydia test kit and get results in minutes. Just keep in mind that rapid tests work best for genital chlamydia and may not detect throat cases.
If your head keeps spinning, peace of mind is one test away. This combo test kit screens for chlamydia, gonorrhea, and other common infections, discreetly, affordably, and from wherever you are.
Why Some Doctors Miss It (And What You Can Do)
Many healthcare providers still don’t ask about oral sex, especially when the patient is young or assumed to be heterosexual. That can lead to incomplete testing, urine only, no throat swab, no rectal test, and false negatives. If you weren’t swabbed in the place where the infection lives, the test won’t find it.
That’s why it’s crucial to advocate for yourself. If you’ve had oral sex, say so. If you’re using an at-home kit, choose one that tests the right areas. According to research in the journal “Sexually Transmitted Diseases”, up to 70% of chlamydia infections in the throat can be missed if testing isn’t done at the site of exposure.
Being clear about what kind of contact happened isn’t shameful, it’s smart. Whether you’re 15 or 45, you deserve a test that fits your reality, not your provider’s assumptions.
People are also reading: What to Do After a Positive HPV Pap Smear (No Panic Required)
The Emotional Toll: Shame, Confusion, and Silence
We need to talk about the shame spiral. Many people, especially teens, blame themselves for “messing up,” even when they took precautions. They thought oral was safe. They didn’t think it counted. Now they’re scared, isolated, and unsure what to do.
If that’s you, take a breath. Having chlamydia doesn’t mean you’re dirty, reckless, or broken. It means you’re human, and you had an encounter that carried risk. The good news? Chlamydia is highly treatable, usually with a single dose of antibiotics. What matters most is finding it early and stopping the cycle.
Every time we say “you can’t get STDs without sex,” we isolate the people who got them another way. It’s time to replace silence with clarity, and to support each other in the process.
What Happens If You Leave Chlamydia Untreated?
Let’s be blunt: chlamydia doesn’t always cause symptoms, but it can cause serious damage if left untreated. Whether it's in the throat, genitals, or rectum, the bacteria can silently spread and inflame tissues. Over time, this can lead to complications that aren’t easy to reverse.
In people with a uterus, untreated chlamydia can travel from the cervix to the uterus and fallopian tubes, leading to pelvic inflammatory disease (PID). PID can cause chronic pain, scarring, and even infertility. For people with penises, chlamydia can lead to epididymitis, a painful inflammation of the tubes that carry sperm.
Even in the throat, chlamydia can linger and re-infect partners. It doesn’t just “clear up on its own.” And because people often don’t realize they’re infected, the bacteria can pass from partner to partner, feeding a silent epidemic.
How Long Before Chlamydia Shows Up on a Test?
Chlamydia doesn't show up right away. It has a window period, which is the time between when you are exposed to it and when a test can find it. If you have chlamydia, it usually shows up between 7 and 14 days after you had sex. If you test too soon, you might get a false negative, which makes people feel safe when they shouldn't.
Here’s how the timing breaks down:
Figure 3. Chlamydia detection timeline after oral or genital exposure.
Some quick tests give results right away, but they might not be as accurate as lab-based NAATs (nucleic acid amplification tests). If you get a negative result but still have symptoms or worries, you should test again in 2 to 3 weeks, or sooner if your doctor tells you to.
How to Talk to a Partner (Without the Panic)
Getting diagnosed with an STD can feel overwhelming. But part of protecting yourself, and your partners, is starting that awkward but necessary conversation. The trick is to focus on facts, not blame.
Try something like: “Hey, I wanted to let you know I tested positive for chlamydia. We didn’t have full sex, but we did have oral contact, and I’ve learned that’s enough to transmit it. You might want to get tested too, just to be safe.”
You don’t have to name names, explain everything, or carry shame. You're doing the responsible thing. According to data from the National Institutes of Health, people who get notified by partners are significantly more likely to test and get treated, helping stop the spread.
Some online services even offer anonymous partner notification tools. If you’re not comfortable saying it directly, you can still protect others without outing yourself.
FAQs
1. Wait, can you actually get chlamydia from just oral sex?
Yep. That’s not a myth. If someone has chlamydia in their genitals, giving them oral can transfer it to your throat. And it works both ways, if they have oral chlamydia, they can pass it to your junk. No penetration required.
2. But I’m still a virgin. How could I have an STD?
Totally fair question, and super common. “Virgin” usually means no vaginal or anal sex, but chlamydia doesn’t care about technicalities. If there’s fluid contact (oral, fingers, toys, rubbing), there’s still a chance. It doesn’t make you “not a virgin”, it just means biology did its thing.
3. How would I even know if I had oral chlamydia?
Honestly? You probably wouldn’t. Most people don’t feel a thing. Some get a sore throat that lingers, maybe swollen glands. But it rarely screams “STD.” That’s why it’s called a silent infection. If you’ve had oral contact and something feels off, or even if it doesn’t, testing is the only way to be sure.
4. How soon after hooking up should I test?
Give it at least a week, ideally two. Chlamydia needs time to build up enough to show on a test. Test too early and you might get a false negative, especially if the exposure was recent. If in doubt, test at 14 days, or test early and plan a retest.
5. I took an STD test, but it was just a pee test. Am I good?
Only if the exposure was genital. If you had oral sex and they didn’t swab your throat, that test might’ve missed something. Many clinics skip throat or rectal testing unless you specifically ask, so it’s totally possible to get a false sense of security. You deserve full-scope testing based on what actually happened.
6. Can chlamydia spread from fingers or sex toys?
Yes, and not in a “urban legend” way. If fluids are involved and fingers or toys go from one person to another without washing, the bacteria can tag along. It’s not the most common route, but it happens. Think: fingers that touch vaginal fluid, then go inside another person. Same with toys. Clean between uses and use condoms on toys if sharing.
7. If it’s in my throat, can I give it to someone else?
Definitely. Oral chlamydia can be passed to a partner’s genitals during oral sex. You might not even know it’s there, but if it is, it’s contagious. That’s why some people keep passing it back and forth without realizing what’s going on.
8. Will antibiotics fix it even if it’s in my throat?
Yes. The same meds that treat genital chlamydia usually knock it out everywhere, genitals, rectum, throat. The key is getting the diagnosis in the first place. Once you know it’s there, treatment is straightforward.
9. Do I really have to tell my partner about this?
Hard truth: yeah, you should. It’s not about blame, it’s about protecting them (and you). Think of it like sending a weather warning. You’re not causing the storm, you’re just letting them bring an umbrella. There are even anonymous tools if saying it out loud feels impossible.
10. Is it really worth testing if I feel fine?
Totally. Most people with chlamydia feel nothing at all. No symptoms ≠ no infection. And the longer it sits there, the more likely it is to cause issues, or get passed on. Think of testing as tuning in before the static gets loud. Peace of mind is powerful.
What Treatment Looks Like, and What Comes Next
The good news: chlamydia is curable. Treatment usually involves a short course of antibiotics, often just a single dose of azithromycin or a week of doxycycline. It’s fast, effective, and widely available.
If you test positive, a healthcare provider (or telehealth service) can prescribe meds. After treatment, it’s important to avoid any kind of sexual contact, oral, vaginal, or otherwise, for seven days. That gives the antibiotics time to fully clear the infection and helps prevent re-infection or passing it back and forth between partners.
You’ll also want to retest after about three months, even if you’ve had no new partners. This isn’t about punishment; it’s just smart follow-up. Reinfection is common, especially when partners aren’t treated at the same time.
Ready to take that step? You can return to STD Test Kits to find the best testing option for your situation, fast, discreet, and stigma-free.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Chlamydial Infections: Treatment Guidelines – CDC
3. Chlamydia – Symptoms & Causes (Mayo Clinic)
4. Chlamydia Infections – MedlinePlus
5. Condom Use: An Overview – CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease doctor who specializes in preventing, diagnosing, and treating STIs. He combines clinical accuracy with a straightforward, sex-positive approach and wants to make it easier for people in both cities and rural areas to read his work.
Reviewed by: A. Lin, MPH | Last medically reviewed: January 2026







