How Long After Exposure Can Chlamydia Be Detected?
Quick Answer: The FDA has approved two new oral drugs, zoliflodacin and gepotidacin, for treating gonorrhea, a major shift in combating antibiotic resistance. While this is huge for treatment, it doesn’t replace the need for accurate, timely STD testing, especially through at-home kits that catch infections early and discreetly.
This week, the New York Times and MSN Health reported that the U.S. Food and Drug Administration had approved two new oral antibiotics for gonorrhea, one of the most stubborn and increasingly drug-resistant STDs in the world. This is a big deal, especially if you’ve ever worried about a one-night stand turning into something more serious, or you’ve heard the phrase “super gonorrhea” and felt that knot in your gut. But while new treatments are game-changing, they don’t replace the need to test early, test again if needed, and make sure your partners get checked too. That’s where discreet, at-home testing still plays a critical role, and this article will walk you through how and when to do it.

People are also reading: UTI Symptoms Again? Here's When to Suspect Chlamydia
Who This Guide Is For (And Why It Matters)
If you're reading this, chances are you've either had a recent scare, maybe a condom broke, or you’ve had symptoms that won’t quite go away, or you're just trying to stay on top of your sexual health. Maybe clinics aren’t close. Maybe you’re not ready to tell anyone. Maybe you’re queer, newly exploring, or dealing with shame from an old trauma. This guide is for you.
It’s also for anyone who’s heard the word “resistant” and thought: What if the meds don’t work next time? New FDA-approved options like zoliflodacin and gepotidacin may help close that fear gap. But the only way to get treated is to know you’re infected, and that starts with a test. Whether you’ve got no symptoms or a sore that came out of nowhere, testing from home can be a private, reliable way to get answers without jumping through hoops.
Throughout this guide, we’ll break down what counts as a gonorrhea test, how soon you can test after sex, when to retest if you’ve been treated, what to expect with home kits, and how privacy, shipping, and partner care all come into play.
What Actually Counts as an STD Test?
When we talk about “getting tested,” not all tests are created equal. For gonorrhea, the gold standard is a NAAT (nucleic acid amplification test), also called a PCR. This test looks for the actual genetic material of the bacteria. It’s highly sensitive and can be done on a urine sample, a vaginal or urethral swab, or even from the throat or rectum depending on your exposure.
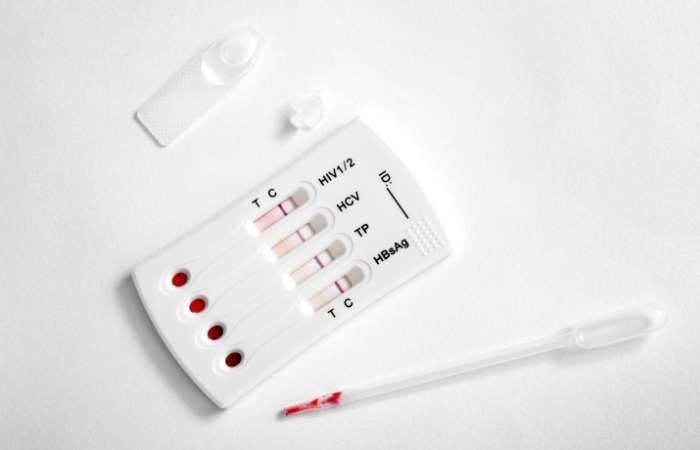
At-home gonorrhea test kits often use the same lab-grade NAAT method. You collect your sample yourself, ship it in, and get results in a secure portal within a few days. Other options include rapid antigen tests, available for some STDs like HIV or syphilis, that give results in minutes from a fingerprick or swab. These are fast but may miss early infections or asymptomatic cases.
If you want fast answers without waiting rooms, STD Test Kits offers confidential, doctor-trusted options.
Window Periods: What to Know for Each STD
Your exposure date matters more than you think. Every STD has a different “window period”, the time between infection and when a test can reliably detect it. Testing too soon can give you a false sense of relief. Testing at the right time helps you catch infections before symptoms appear or before you pass them to someone else. Here's how the timing breaks down across common STDs:
Figure 1. Window periods for common STDs. Testing too early may result in false negatives. Always follow up if symptoms persist or exposure was high-risk.
Rapid Test vs Lab Test: Pros, Cons, and Tradeoffs
Not all testing happens in clinics anymore, and that’s a good thing. Imagine this: one person is parked outside a hookup’s house, nervously swabbing their throat with a mail-in test kit. Another’s pacing in a motel bathroom, waiting for the result of a rapid fingerstick test. The question isn’t which one is braver, it’s which test fits their needs. Here’s how the different types stack up:
Figure 2. Comparing test methods. Rapid kits are fast and private, while lab kits offer more sensitivity. Clinical testing remains the gold standard for complex or persistent symptoms.
When to Test After Exposure
If you’ve had a possible exposure to gonorrhea, unprotected sex, a broken condom, or even oral sex with a new partner, timing your test is everything. If it’s been less than five days, most tests won’t pick up the infection yet. You can test, but be prepared to retest. Between 7 to 13 days post-exposure, NAAT tests may start to detect infection. After 14 days, accuracy is at its peak.
Case in point: Elijah, 27, took a home urine test just four days after a hookup that left him feeling uneasy. It came back negative. But two weeks later, symptoms showed up, a dull burn during urination and some discharge. A follow-up NAAT confirmed gonorrhea. That early test? Too early. That second one? Right on time.
If you're in that limbo, wondering if it’s too soon, or already too late, know this: you're not alone. Many people test more than once, not because they’re paranoid, but because they understand how timing affects results. If you’re unsure, peace of mind is one discreet test away.
Do You Need to Retest? Here’s How to Know
There are three main reasons to retest: your first test was too early, you’ve been treated but could get reinfected, or you’ve got lingering symptoms. If you tested within a few days of exposure and got a negative result, you should retest around the two-week mark to catch late-detecting infections like gonorrhea, chlamydia, or trichomoniasis.
If you’ve already been treated, the CDC recommends retesting for gonorrhea three months after treatment, even if symptoms are gone and you’ve had no new partners. That’s because reinfection is common, especially if your partner didn’t get treated or you’re still sexually active together.
Scene from real life: Aja, 34, thought she was done with it. She and her ex had both tested, treated, and moved on. But a month later, the symptoms crept back. She retested, positive again. Turned out, he never finished his antibiotics. That retest saved her from another month of pain and confusion.
If any of this sounds familiar, it’s time to act. You can return to STD Test Kits to choose a home option that fits your needs, your timing, and your life.
Privacy, Shipping, and Discreet Support
When you’re already nervous, the last thing you want is a bright red box labeled “STD TEST” sitting in your mailbox. That’s why reputable providers use plain packaging, no logos, no medical labels, no giveaways. Shipping is fast, often within 1–2 business days, and you can choose where it gets sent: home, work, or a pickup location.
Results are private, too. You get a secure login, not a voicemail on your parent’s phone or an awkward call during your lunch break. Many at-home kits also come with support access, live chat, telehealth consults, or doctor guidance if you need help interpreting results or planning treatment.
Whether you're traveling, living rurally, avoiding clinics for personal reasons, or just want peace of mind without judgment, at-home testing gives you control. Because sexual health should never come at the cost of emotional safety.
What If You Test Positive?
First, breathe. A positive result isn’t a moral failure, it’s a medical situation, and it’s more common than you think. According to the CDC, gonorrhea is one of the most frequently reported STDs in the United States, with over 700,000 new cases each year. And now, with FDA-approved oral antibiotics like zoliflodacin and gepotidacin, treatment just became more accessible.
Still, you’ll want to confirm your result, especially if you used a rapid test or tested early. Then it’s time to notify recent partners. Many at-home test providers offer anonymous partner notification tools, and clinics can help with discreet outreach. Treatment is typically a single oral dose or a short course, no hospital, no injections, no judgment.
Picture this: Darrell, 22, got a positive result on a home test. He panicked, thought he’d have to call his last three hookups, face judgment, maybe even lose a relationship. Instead, he accessed a telehealth service that walked him through treatment and gave him options for anonymous texts. The world didn’t end. It just got clearer.
And if your result is negative but your gut says otherwise? Retest. Trust yourself. Because when it comes to STDs, knowing is always better than guessing.
People are also reading: Do Gonorrhea Rapid Tests Work? What the Science (and Users) Say
FAQs
1. Can I really get gonorrhea from oral sex?
Yes, throat gonorrhea is real, and it’s sneakier than most people think. You might not feel a thing, or maybe just a sore throat that doesn’t go away. If you’ve given or received oral sex without protection, especially with a new or multiple partners, it’s worth testing. Most clinics don’t even check the throat unless you ask, which is why home swab kits can be a game-changer.
2. How soon after sex can I get tested?
You’ll want to wait at least 7 days after exposure to test for gonorrhea, but 14 is better if you want the most accurate result. Early tests can miss it. If you're already feeling off, burning, discharge, or something just feels wrong, test now, and plan to test again if needed. Timing matters, but so does trusting your gut.
3. Are these new gonorrhea pills available to the public yet?
Not instantly. The FDA approval is the green light, but rollout takes time, think pharmacy stocking, insurance approvals, provider training. Still, this is a massive win. For now, standard treatments still work for most cases, but options like zoliflodacin and gepotidacin are coming, and that’s a big deal for fighting resistance.
4. If there are new treatments, do I still need to get tested?
100%. No test, no treatment. The fancy new antibiotics can’t help if you don’t know you’re infected, and many people with gonorrhea don’t have obvious symptoms. Testing is how we stop the spread, protect partners, and get care when we need it. Think of it as basic hygiene for your sex life.
5. I tested negative, but I still have symptoms. Now what?
It happens. You might’ve tested too early, or the test missed something. Retest after a week or go to a clinic if things are getting worse. Also, not everything that burns is gonorrhea, it could be chlamydia, trich, a UTI, or something non-infectious. That’s why combo test kits exist: bodies are complex.
6. Is it possible to catch gonorrhea again after treatment?
Definitely. That’s not your fault, it’s just how bacteria works. You could get reinfected if your partner wasn’t treated or if you’re exposed again. That’s why retesting after three months is standard advice. If you’re having new partners or condomless sex, more frequent testing is self-care, not paranoia.
7. What makes home STD tests accurate or not?
It’s all in the method and the timing. The best home kits use lab-grade NAAT testing, the same kind used in clinics. Swab right, ship fast, test within the right window, and your results are legit. Just don’t test too soon after exposure and expect a miracle. Testing is science, not magic.
8. Do I really have to tell my partner if I test positive?
We get it, this is the part that makes most people freeze. But honesty here isn’t just ethical, it’s protective. A short, calm heads-up can prevent complications, reinfection, or worse. If you can’t say it directly, there are anonymous text tools that get the job done. Blame the bacteria, not yourself.
9. What if I’m scared to see my results?
Totally normal. That moment before you open the email or check the portal? Pure heart-race territory. But knowledge is power, cliché as that sounds. A positive result doesn’t make you dirty or broken, it makes you informed. And informed people can get treated, protect others, and move on stronger.
10. Are these new drugs the end of drug-resistant gonorrhea?
Not yet, but they’re a huge step. For years, gonorrhea’s been outsmarting antibiotics. These two new options give doctors backup, especially for resistant cases. But bacteria evolve fast. If we want these drugs to keep working, testing and early treatment still matter. No one med saves the world, but every test helps.
You Deserve Answers, Not Assumptions
Whether you're panicking after a hookup or simply being proactive, getting tested, on your terms, can shift fear into power. The FDA’s approval of new gonorrhea treatments is incredible news, but it doesn’t erase the need for timely testing, partner care, and smart follow-ups. Especially if privacy matters to you, or you’ve felt judged in the past, at-home testing offers a quiet kind of strength.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. FDA Approves Two New Oral Treatments for Gonorrhea – NYT
2. MSN Health – New Oral Gonorrhea Treatments Approved
3. Gonorrhea – Diagnosis & Treatment | Mayo Clinic
4. Zoliflodacin Overview | Wikipedia
5. Gepotidacin (Blujepa) Overview | Wikipedia
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: K. Monroe, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.






