No Symptoms, No Clue, Why Herpes Often Goes Undetected
Quick Answer: Testing positive for herpes while your partner has no symptoms is common. Many people with herpes are asymptomatic or misattribute symptoms. Retesting, communication, and possibly partner testing are the next steps.
This Isn’t Rare, It’s Just Not Talked About
Daniel, 27, got tested before starting PrEP.
“When they told me I had HSV-2, I thought it had to be a mistake. My boyfriend’s never had anything,” he said. “But when he got tested, his IgG came back negative. I was the ‘positive one.’ But…how? We’ve only been with each other.”
What Daniel learned, what many learn after the initial shock, is that herpes isn’t always visible. A person can have the virus for years without ever having a single noticeable sore. Or they might mistake a mild outbreak for a shaving cut, irritation, or a pimple that came and went.
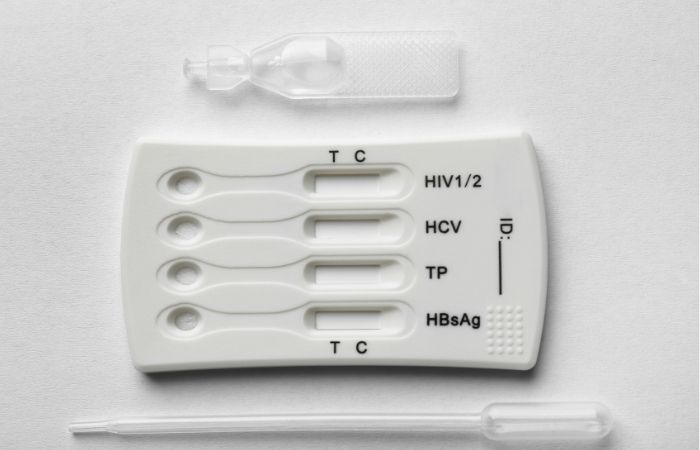
This is why so many people don’t get tested for herpes unless they specifically ask. Routine STD panels often skip herpes unless requested, due to testing limitations and the high rates of asymptomatic infection.
People are also reading: STD or Skin Irritation? What Red Spots on Your Vagina Really Mean
Why You Might Be Positive, and They’re Not
So, why the mismatch? Here are four of the most common reasons:
Table 1. Common reasons for discordant herpes results between partners.
It’s tempting to point fingers, but most of the time, this mismatch is no one’s fault. The virus is sneaky. The tests aren’t perfect. And the emotions? Totally real.
Reading the Results: Are You Sure It’s Accurate?
If you took a rapid test or an IgG blood test and came back positive, you’re probably wondering: is it real? Could it be wrong? Especially if you’ve never had a visible outbreak, it’s natural to doubt the result.
Studies that have been peer-reviewed show that the herpes IgG test isn't perfect. It's good at finding HSV antibodies, but it can give false positives, especially if your index value is close to the cutoff. Experts often suggest a confirmatory test like the Western Blot for values between 1.1 and 3.5. This test is more specific but not always easy to find.
Make sure that the at-home herpes test you use comes from a trusted source. If the results are unclear, you should get clinical testing done. STD Test Kits sells quick, accurate kits for personal screening, but lab tests that confirm the results may still be useful.
Herpes isn’t black-and-white, and neither are the test results. That’s why understanding the limitations is key before jumping to conclusions about who gave what to whom.
What No One Tells You About "Asymptomatic Herpes"
Let’s clear up one of the biggest misconceptions: not having symptoms does not mean not having herpes. In fact, studies show up to 80% of people with HSV-2 don’t know they have it. They may have mild symptoms like itching, tingling, or tiny cracks in the skin that go unnoticed.
This is especially common with genital HSV-1, which is increasingly passed through oral sex. A partner may carry oral herpes since childhood, then transmit it genitally during oral sex without any signs of an active cold sore.
There’s also something called "subclinical shedding", where the virus is active on the skin without causing any sores. During these times, herpes can still be passed to a partner through skin-to-skin contact, even if no symptoms are present. That's why herpes is so common and yet so misunderstood.
“I Swore I Was Clean. Then My Partner Tested Positive.”
Karina, 31, had been in a monogamous relationship for two years when her boyfriend got tested during a routine screening.
“He texted me saying he was HSV-2 positive. I was in shock. I’d never had a single outbreak. I was furious. But when I finally got tested, I was positive too,”
This situation is surprisingly common. Herpes is often passed in the early months of a relationship, sometimes even before exclusivity is established. One partner may have had it from a past relationship, then unknowingly passed it along.
Blame rarely helps, but testing, talking, and understanding what herpes really is? That changes everything.
What to Do After a Herpes Diagnosis
It can feel like a punch in the gut to find out you have herpes. You might want to hide, or you might want to do a lot of research. Both responses are normal. But here's the most important thing: this virus doesn't define you. It doesn't mean you're in danger, unloved, or going to suffer.
In the first 24 to 72 hours, you should focus on:
Table 2. Initial steps after a herpes diagnosis and why they matter.
You don’t have to figure this out alone, and you don’t have to rush every conversation or decision.
Treatment Basics: What’s Next If You’re Positive
If you’ve tested positive for herpes simplex virus (HSV-1 or HSV-2), the next step may be medication. Antiviral treatments like acyclovir, valacyclovir (Valtrex), or famciclovir can do two things: reduce the severity and duration of outbreaks, and lower the chance of passing herpes to a partner.
If this is your first outbreak, a provider may prescribe a short 7 to 10-day course of antivirals. If you have frequent or painful outbreaks, you may be a candidate for suppressive therapy, daily medication that reduces shedding and flare-ups.
This is where many people get stuck: Do I have to take meds forever? The answer is no, not unless you choose to. Suppressive therapy is optional and depends on your lifestyle, outbreak frequency, and comfort level with risk.
Some couples choose suppressive therapy for one partner and condoms for the other. Others decide to skip daily meds and just treat outbreaks. There’s no one right way, it’s about your body, your relationships, and your peace of mind.
Telling Your Partner: Scripts, Fears, and What Actually Helps
This part might feel scarier than the diagnosis itself: telling your partner you have herpes. But many people are more understanding than you’d expect, especially when you speak with honesty and compassion.
Here’s one way to start the conversation:
“Hey, I got my STI panel back and it was positive for herpes. I was surprised, and I want to share it with you because it matters to both of us. I don’t have all the answers yet, but I’ve been reading and there’s a lot we can do to stay safe together.”
Not sure your partner will understand? Consider anonymous notification tools through public health departments, or telehealth services that help with partner contact. But whenever possible, direct conversations, grounded in calm, science-based facts, lead to the most respectful outcomes.
If you’re not in a committed relationship, that doesn’t mean you don’t deserve compassion. Disclosure is still recommended before sex, but how and when you share is yours to decide. If the person shames you, that’s about them, not about your value or your future.

People are also reading: Is That Toy Safe? What You Risk When Couples Share Sex Toys
Should You Retest? Here's When It Makes Sense
If your result was from a rapid or IgG test and you're still confused, or if your partner's test was negative, you might want to retest in a few weeks. Here’s why:
The window period for herpes antibody development can range from 2 to 12 weeks. If your test was taken during the early stages of infection, your levels might not be detectable yet. On the flip side, false positives can occur with low index values, especially under 3.5 on the IgG scale.
In those cases, confirmatory testing like a Western Blot or a retest in 4 to 6 weeks can provide clarity. Just remember: even without retesting, if you’re experiencing symptoms or were exposed by a partner with herpes, clinical diagnosis is enough to begin treatment.
Need clarity without the clinic visit? This discreet at-home test kit screens for multiple STDs, including herpes, and gives results in minutes, no waiting room, no awkward questions.
Preventing Transmission and Reinfection
Now that you know you’re positive, how do you protect your partner, especially if they’re currently testing negative?
There’s good news. With a few practical steps, you can drastically reduce the chance of passing herpes to someone else:
- Use condoms or dental dams, they don’t eliminate all risk but significantly reduce transmission
- Consider suppressive therapy, daily antivirals lower asymptomatic shedding
- Avoid sex during outbreaks, visible symptoms = higher transmission risk
- Track your patterns, you’ll learn what triggers outbreaks and when to be extra cautious
And yes, it’s entirely possible to have a safe, intimate, loving relationship post-diagnosis. Many do. In fact, herpes is often more emotionally disruptive than physically.
Your diagnosis is not a death sentence for your sex life, it’s an invitation to move forward with more clarity, communication, and confidence.
When the Stigma Hits Harder Than the Symptoms
For many people, the emotional fallout of a herpes diagnosis can be heavier than any physical discomfort. You might feel shame, guilt, rage, confusion, or grief. These feelings don’t mean you’re weak, they mean you’re human.
Herpes lives at the intersection of sex, silence, and shame. And because it’s often misunderstood, the diagnosis can feel socially isolating. But that isolation isn’t inevitable. Support is out there, real, compassionate, shame-free support.
Start here:
- Online support forums: Reddit’s r/Herpes and other community boards are filled with lived experience, humor, and solidarity.
- Therapy: Look for sex-positive, STI-informed therapists. Websites like TherapyDen allow you to filter by those terms.
- Peer stories: Blogs, YouTube channels, and podcasts are increasingly normalizing herpes and STI stigma. Hearing from others can be healing.
And most importantly: you are not less worthy of love, trust, or intimacy. Herpes is a virus, not a moral verdict.
FAQs
1. Can my partner test negative for herpes but still have it?
Absolutely, this happens more often than people realize. They might’ve been infected years ago and never had symptoms. Or they tested too soon, before antibodies had time to develop. Herpes is tricky like that. The virus doesn’t always follow the script, and neither do the tests.
2. What’s the real difference between HSV-1 and HSV-2?
Think of HSV-1 as the overachiever of cold sores, it usually hangs out around the mouth but can also show up genitally (thanks, oral sex). HSV-2 tends to prefer the genitals and is more likely to cause recurrent outbreaks. But both can infect both areas, and both are way more common than people think.
3. Can I pass herpes even if I feel totally fine?
Yep. That’s the frustrating part. Herpes can shed silently, no sores, no tingles, no warning. That’s why protection and suppressive meds can help, even when everything seems “normal.” The goal is managing risk, not living in fear.
4. Is the herpes test always accurate?
Not exactly. IgG tests (the common type) can miss infections early or give false positives if the numbers are low. If your result came back with a value between 1.1 and 3.5, that’s a fuzzy zone. A confirmatory test like the Western Blot is more reliable, but not always easy to get. Timing matters too, test too early, and it might miss the infection.
5. Should I retest if my result felt…iffy?
If your gut says “huh?”, retest. Especially if you’re in that low-positive range or didn’t wait the full window period. A follow-up in a few weeks or a second method can give peace of mind. Just make sure you're comparing apples to apples (i.e., same test type or a confirmatory one).
6. Do I have to take herpes meds forever?
Not unless you want to. Some people only take antivirals when they have outbreaks. Others go on daily suppressive therapy to keep things chill and reduce the risk to partners. It’s your call, and you can always change your mind. Think of it like birth control: your body, your timing, your terms.
7. Can I have herpes and never know it?
Oh, totally. That’s the silent majority. You could go years, or a lifetime, without symptoms and only find out because you got tested for something else. Herpes is sneaky that way. That’s why testing is more about clarity than catching something “new.”
8. How do I even bring this up to future partners?
Gently, honestly, and when you're not in the heat of the moment. Try: “Before we get closer, there’s something I want to share. I have herpes, and I’ve learned a lot about how to keep partners safe.” Most people appreciate the honesty, and if they don’t? That’s a red flag, not a reflection of your worth.
9. Can I still have oral sex if I have genital herpes?
Yes, with some care. Using barriers like condoms or dental dams helps, especially during outbreaks (which you should avoid anyway). Suppressive therapy can lower the risk too. It’s all about informed choices, not eliminating pleasure.
10. What about pregnancy, can I still have a baby?
100%. Just make sure your provider knows you have herpes. They might prescribe antivirals during the last few weeks of pregnancy to prevent transmission during delivery. Vaginal birth is still totally possible for most people with herpes.
You Deserve Answers, Not Assumptions
Testing positive for herpes while your partner has no symptoms can feel like you’re living in a bad dream. But once you understand the science, the stigma starts to lose its grip.
Whether you’ve had symptoms or not, whether your partner is negative or unaware, this moment doesn’t define you. It’s just a fork in the road, and now you have the tools to choose your next step.
Want fast, discreet, at-home testing for you or your partner? This combo test kit screens for multiple STDs and gives results in minutes, with no lab visit required.
You deserve answers. You deserve care. And most of all, you deserve peace of mind.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. American Sexual Health Association – Herpes Resource Center
2. Reddit – r/Herpes Support Community
3. CDC — Herpes (HSV) Treatment Guidelines
5. ASHA — Herpes & Relationships
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to prevent, diagnose, and treat STIs. He combines clinical accuracy with a straightforward, sex-positive approach and is dedicated to making it easier for readers to get to know him, whether they live in a city or off the grid.
Reviewed by: M. Rivera, NP | Last medically reviewed: October 2025







