When to Test for Syphilis After Exposure (And When Not To)
Quick Answer: STD symptoms aren’t always obvious. If you’ve had unprotected sex, noticed new genital symptoms, or just feel off, testing is the only way to know. Some STDs show no signs at all, and early testing means earlier treatment and peace of mind.
Who This Guide Is For (And Why It Matters)
This guide is for the overthinkers. The ones who keep refreshing symptom pages. The ones who feel fine physically but not emotionally. It’s for people who didn’t mean to skip the condom, or thought oral sex was “safe enough,” or who’ve never tested before because no one ever explained how or when or why. Whether you’re in a monogamous relationship, dating casually, living off-grid, or just woke up scared after last night, this is for you.
STD testing isn’t punishment. It’s care. It’s control. It’s saying, “I want to take care of myself and my partners,” even if those partners are temporary or situations were messy. This article will walk you through the real signs it might be time to test, the difference between symptoms and guesswork, and what happens next, without shame, jargon, or fear tactics.
We’ll cover:
- 6 major signs that signal it’s time to test (even if you feel fine)
- What to expect during testing, physically and emotionally
- How long to wait after exposure for accurate results
- Where to get tested, clinic, mail-in, or rapid home tests
You deserve answers. Let’s start with the signs.

People are also reading: How Herpes Creates the Perfect Conditions for HIV to Enter the Body
Sign #1: You Had Unprotected Sex (Even Once)
Aiden, 22, had just moved to Austin. “I didn’t think one night would matter,” he said. “We didn’t use a condom, but I felt fine the next day. Then I found out she’d just gotten treated for chlamydia.” He didn’t feel sick, didn’t have any burning or discharge. But when he got tested two weeks later, he tested positive. “I wouldn’t have known if she hadn’t told me.”
Unprotected sex, vaginal, oral, or anal, means exposure. Even once. Even if you pull out. Even if it was quick. STDs like chlamydia, gonorrhea, and herpes can spread through fluids or skin-to-skin contact, and you can’t tell who has what just by looking.
If you had sex without a barrier method and you don’t know your partner’s testing status, it’s time to test. Especially if they’re new, casual, or non-monogamous, or if you didn’t talk about testing beforehand.
Sign #2: You’ve Noticed New Genital, Anal, or Oral Symptoms
This one sounds obvious, but it’s not. A lot of people think symptoms have to be dramatic, green discharge, severe pain, blistering sores. But early signs of an STD can look like:
- Bumps or pimples near the genitals, anus, or mouth (especially if persistent)
- Itching or tingling in one spot that won’t go away
- Redness, swelling, or a rash (even if it’s not painful)
- Discomfort during sex or when peeing, even without discharge
Herpes can start as a tiny itch or a single clear blister. HPV warts may be so small you barely notice. Chlamydia often causes nothing at all, especially in people with vaginas.
If something looks or feels different down there, especially after a new partner, test. Even if it goes away. Even if it’s just “a little off.”
Sign #3: Your Partner Tested Positive, or You’re Not Sure
It’s a brutal moment: the “hey… I just got tested” text. Maybe they didn’t know. Maybe they were asymptomatic. Maybe it was from before you. Doesn’t matter, you deserve to know your status, too.
If a partner tells you they tested positive for any STD, even if you don’t have symptoms, go get tested. Not later. Not “when I have time.” Some infections, like gonorrhea and trichomoniasis, can pass without symptoms. Others may take days or weeks to show up clearly, but that doesn’t mean you’re not already exposed.
And if you’re with someone new and you don’t know their testing history? That uncertainty alone is a reason to test, especially if condoms weren’t used consistently.
Sign #4: You Feel “Off” After a Sexual Encounter
This one’s harder to explain, but if you know, you know. It’s that gut-punch of anxiety the morning after. Maybe you were drinking. Maybe the vibe wasn’t what you thought. Maybe something felt off during or after the hookup, even if nothing technically “went wrong.”
One reader described it like this: “I kept replaying everything. He didn’t finish inside me, but there was no condom. I felt sick with worry, even though my body felt normal.”
Trust that feeling. STD symptoms don’t always appear right away. But emotional symptoms, panic, regret, a racing mind, often show up fast. Getting tested can give you a concrete answer to balance out that spiral. And if exposure did happen, you’re catching it early, which matters for both treatment and peace of mind.
Sign #5: You’ve Had a New Partner (Even If It Was “Safe”)
It doesn’t have to be unprotected to be risky. Skin-to-skin STDs like herpes and HPV can spread even with condom use. Oral sex can transmit gonorrhea, syphilis, and more. And most people with STDs don’t know they have them, because they don’t feel anything.
If you’ve had any kind of sexual contact with a new person, especially someone whose testing history is unclear, testing is smart. It’s not about blaming them. It’s about knowing what your body’s been exposed to so you can make informed choices for your future partners, too.
This is especially important if you’ve started a new relationship and want to stop using condoms. A baseline test for both of you is the most caring thing you can do.
Sign #6: You’ve Never Been Tested (Or Not in a Long Time)
Let’s be real: a lot of people have never had an STD test. Or they think their annual physical “covered it.” Spoiler: most regular checkups don’t include STD panels unless you specifically ask.
If you’ve had any sexual contact and it’s been more than a year, or never, it’s time. Especially if:
- You’ve had more than one partner
- Your partner has other partners
- You’re under 25 (screening is recommended more often)
Testing isn’t just for when something feels wrong. It’s part of basic sexual health. The CDC recommends routine testing for STDs based on age, risk, and activity. If you’ve never asked, now’s the time to start.
Timing Matters: When to Test After Exposure
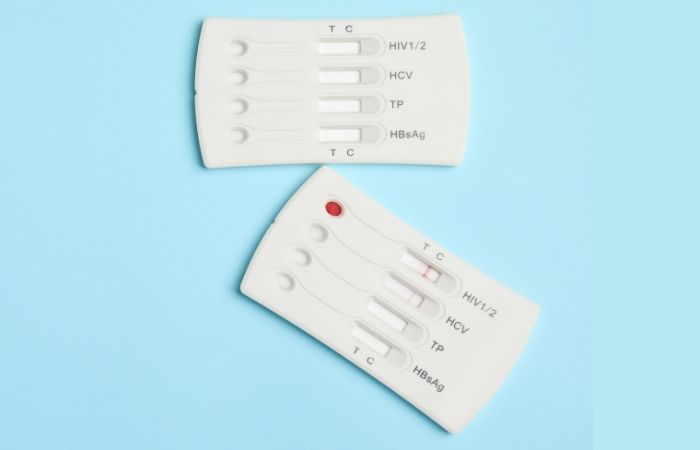
You might feel like testing immediately, like, today, but not all STDs show up right away. That’s where window periods come in. A window period is the time between exposure and when a test can reliably detect infection. Testing too early can lead to false negatives, even if you’re already infected.
Here’s what typical window periods look like for common STDs:
Figure 1. STD test window periods. Wait long enough for reliable results, early tests may need to be repeated.
It’s okay to test early for peace of mind, but know you may need a follow-up test to confirm. Some test kits include this info in their instructions, always read carefully.
When Testing Too Early Gives False Comfort
Ty, 28, had a fling at a music festival. “I felt off afterward, so I ordered a test kit right away,” he said. The result came back negative. But a week later, he had painful urination and a small sore near his groin. A second test confirmed gonorrhea. “I’d tested too early. I thought I was safe, and I wasn’t.”
Don’t beat yourself up if this happens to you. The urge to get answers is normal. But remember: testing is about timing as much as exposure. If you test within a few days of a risky encounter, mark your calendar and plan a retest at the ideal window.
If your head keeps spinning, peace of mind is one test away. Whether it’s a bump or a vibe, you deserve to know what’s going on with your body.
People are also reading: How HPV Can Cause Anal Cancer, And Why Most People Don’t Know
Where (and How) to Get Tested, Without the Awkwardness
Let’s be honest. Walking into a clinic and saying, “Hi, I think I need an STD test” can feel mortifying. The fluorescent lights. The clipboard. The side-eyes you think you’re getting (even if no one’s looking). That’s why more people than ever are choosing at-home testing options, quietly, privately, and on their terms.
You’ve got three main paths to get tested:
Figure 2. STD testing options by privacy, speed, and scenario fit.
If you’re in a rural area, don’t want your insurance to see, or just need to avoid awkward questions, at-home testing is a game-changer. You collect your own sample (urine, finger prick, or swab), follow the simple instructions, and get results fast. Some kits even offer results without mailing anything back.
You can order a Combo STD Home Test Kit to check for the most common infections discreetly, no clinic required. It’s private, fast, and gives you clarity without judgment.
What Testing Feels Like (Emotionally and Physically)
You might be picturing pain. Blood. Awkward moments. But the truth is, most STD tests are quick, simple, and low on discomfort. Here’s what to expect:
- Urine tests: Pee in a cup. That’s it.
- Swabs: Self-swabs are used for throat, vaginal, or rectal testing. Slightly awkward, but not painful.
- Finger pricks: Like a glucose test. Tiny sting, over fast.
- Blood draws: Rare for at-home kits, more common in clinics.
The harder part is emotional: the waiting, the wondering, the “what if” spiral. Especially for first-timers, testing can feel like a moral referendum, but it’s not. It’s a health check. Just like you’d test for strep or COVID or a vitamin deficiency. Testing means you care about your body and your partners. That’s not shameful. That’s powerful.
What If You Test Positive?
Deep breath. A positive result is not the end of the world, or your sex life. Most STDs are treatable, manageable, or both. But first, you need to pause the panic and make a plan.
- Step 1: Check the instructions. Some rapid tests (especially for herpes or syphilis) may require confirmatory lab testing. Don’t assume one result is the full story.
- Step 2: Call a provider, clinic, or telehealth service. You can usually get prescriptions the same day for infections like chlamydia or gonorrhea.
- Step 3: Tell your partners, at least the ones you've had in the last few months. Scripts can help. So can anonymous notification tools. It’s awkward, but it’s the right thing to do.
- Step 4: Retest after treatment (more on this below), and consider full panel screening if you haven’t had one in a while.
Maya, 25, tested positive for trichomoniasis with a rapid kit. “It sucked, but honestly I was grateful to know. My symptoms were subtle, just a weird itch. I would’ve ignored it. Getting treated was fast, and now I always test before new partners.”
Knowledge gives you options. Silence only gives you stress. If something comes back positive, you’re not dirty. You’re informed. And now, you’re taking care of it.
Do You Need to Retest? Here’s How to Know
If you’ve already tested, but you’re still nervous, got treated, or had another exposure, yes, retesting might make sense. Here’s why:
Some STDs, like chlamydia or gonorrhea, can clear after treatment, but remnants of bacterial DNA might linger for a week or more. If you test too soon, you could get a “false positive” that’s really just your body clearing leftovers.
For others, like HIV or herpes, a repeat test might be needed because antibodies take time to develop. A negative test 7 days after exposure might not mean you’re in the clear yet.
General retesting guidance:
- After treatment: Wait 3 weeks to 1 month for clearance confirmation
- After recent exposure: Retest at the full window period (usually 14–90 days depending on STD)
- With new partners or ongoing risk: Test every 3–6 months
Still unsure? Return to STD Test Kits to compare testing options, or talk with a provider. The goal isn’t to test endlessly, it’s to test confidently, at the right time.
Privacy, Shipping, and Support That Doesn’t Judge
You don’t need to walk into a waiting room. No awkward conversations with a pharmacist. No insurance claims if you don’t want them.
STD Rapid Test Kits arrive in plain packaging, no logos, no hints, no disclosures. Most kits ship within 1–2 business days and fit discreetly in a mailbox. And if you live in a small town, with nosy neighbors or shared mailrooms, this matters.
Results are yours. No one else sees them unless you choose to share. And if you have questions about how to swab, what the results mean, or what to do next, their site includes guides, FAQs, and real support, not robotic form letters.
FAQs
1. Can I still have an STD if I feel totally fine?
Oh yeah, unfortunately, that’s super common. Some STDs, like chlamydia and HPV, can chill in your system without a single symptom. You won’t feel sick, itchy, or sore. Nothing. That’s why testing isn’t just for when something feels off, it’s for when something happened and you’re just not sure.
2. How soon after sex can I get tested?
Depends on what you’re testing for. A few infections (like gonorrhea) show up on tests in about a week. Others, like herpes or HIV, might take a few weeks or even longer. Best bet? Test at the two-week mark for a solid baseline, and again later if you’re still worried or if it was a risky situation.
3. Is oral sex “safe”? Or do I need to test for that too?
Hate to break it to you, but oral sex isn’t risk-free. You can catch or pass things like gonorrhea, syphilis, and even herpes just from going down on someone. So yes, if that’s part of your sex life, testing still matters. No shame in being thorough.
4. I saw a bump. Is it herpes?
Maybe. But maybe not. Could be an ingrown hair, friction, or even razor burn (yes, that’s a real thing). Herpes sores tend to be painful, fluid-filled, and come in clusters, but not always. If it doesn’t go away, or if it comes back in the same spot, that’s your cue to test.
5. Can I use an at-home test during my period?
You sure can. Most at-home kits are fine to use during your cycle, just double-check the instructions. Vaginal swabs might be slightly messier, but it won’t affect the result. If it helps you sleep at night, test.
6. Do I have to tell my doctor?
Nope. At-home test results are yours and yours alone unless you choose to share them. If something comes back positive and you want treatment, you can bring the result to a provider, or you can get treated via telehealth in many cases.
7. What if I already tested negative, but I’m still freaking out?
That happens a lot, especially if you tested really soon after a scare. Some STDs don’t show up right away, so you might need a follow-up test later. If it’s been 2–3 weeks and you’re still spiraling? Retest. Not because you “have to,” but because peace of mind is priceless.
8. Can I get reinfected after I’ve been treated?
Yep. That’s the frustrating part, treatment doesn’t make you immune. If your partner didn’t get treated too, or if you have unprotected sex again, it can come back. Think of it like strep throat or lice: treat, retest, and maybe update your playbook.
9. Do condoms protect against everything?
Condoms are superheroes, but not invincible ones. They cut risk dramatically for fluid-transmitted STDs like HIV and chlamydia. But stuff like herpes and HPV? Those can still sneak through skin-to-skin contact. So use them, but also test regularly.
10. What’s the easiest way to just… start?
Honestly? Order a kit. That’s it. Rip off the anxiety Band-Aid. You don’t need to explain yourself to a nurse, you don’t need to leave your house.
You Deserve Answers, Not Assumptions
Testing isn’t just for “other people.” It’s for you, if you’ve had sex, worried after a hookup, noticed a change, or just want to take care of yourself better. You don’t need to wait for a rash or discharge or confession. You just need to want clarity.
Whether you’re sure something’s wrong or just sick of wondering, an at-home test can help you stop guessing and start knowing. And knowing is how you take your power back.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources. Every external link in this article was checked to ensure it leads to a reputable destination and opens in a new tab, so you can verify claims without losing your place.
Sources
1. Getting Tested for STIs (CDC)
2. About Sexually Transmitted Infections (CDC)
4. Sexually Transmitted Infections Overview (MedlinePlus/NIH)
5. STD Diagnosis and Testing (Mayo Clinic)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Hannah Ellis, FNP-C | Last medically reviewed: February 2026
This article is for informational purposes and does not replace medical advice.