When the STD Test Says “Negative” But Your Body Says “Something’s Wrong”
Quick Answer: Lesbian sex can transmit STDs like chlamydia, HPV, herpes, gonorrhea, and trichomoniasis through skin-to-skin contact, fluids, or toys. Testing is still essential, even if you’ve only had sex with women.
When Sex Education Fails You, Testing Becomes Terrifying
Emily, 27, thought she was safe because she’d only had sex with women since college. When a bump appeared on her vulva and didn’t go away, she chalked it up to shaving. A friend finally convinced her to get tested. It turned out to be genital herpes. Her partner didn’t know she had it either.
This isn’t rare. In fact, a CDC study found that women who have sex with women (WSW) often carry the same STD risk profile as their heterosexual counterparts, but are far less likely to be routinely screened, even at the doctor’s office. That disconnect leaves thousands underdiagnosed or confused about what symptoms to watch for.
It’s not your fault if you’ve felt invisible in this conversation. Sex education rarely includes real guidance for queer women. Protection is marketed toward penis-in-vagina sex. Even intake forms at clinics often don’t ask the right questions. But that doesn’t mean the risks aren’t real, it just means the system isn’t built with you in mind. That’s why self-advocacy matters. And it starts with knowing how STDs can actually spread during lesbian sex.
How STDs Really Spread During Lesbian Sex
Let's be honest: sex between women can be just as close, skin-to-skin, and fluid-sharing as any other kind of sex. The idea that it is "safer" or even "immune" to STDs is not based on science. A lot of people don't know this:
Skin-to-skin contact alone can transmit infections like HPV, herpes, and even syphilis. Oral sex can pass on gonorrhea, herpes, and chlamydia. Shared sex toys, especially without cleaning or condoms, can carry trichomoniasis and HIV between partners. And while rare, microtears during friction-heavy acts like scissoring can open up routes for transmission just like any other genital contact.
In a study published in the journal Sexually Transmitted Diseases, researchers found that among WSW, the prevalence of HPV and herpes was nearly equal to women who have sex with men. It wasn’t who they were with that made the difference, it was whether they got tested, and whether protection was used.
Table 1: Common STDs that can be transmitted through lesbian sex, how they spread, and whether a test exists.
People are also reading: How Long Before Chlamydia Affects Fertility? A Breakdown by Stage
Why Many Queer Women Go Untested, And Why That’s Dangerous
You’re not alone if you’ve never been told to test for STDs as a queer woman. In fact, less than half of sexually active WSW report being tested regularly, even when they have multiple partners. Some of that is due to stigma. A lot of it is due to invisibility in medical spaces.
One woman, Nadia, 35, told us: “I asked my doctor if I needed an STD test, and she literally said, ‘Not unless you start seeing men.’ I was mortified, and I didn’t get tested for another three years.”
When providers assume you’re low-risk based on sexual orientation, it creates a false sense of safety. But infections don’t discriminate. What matters is what kind of contact you’ve had, not who you’ve had it with. And when testing is delayed, silent infections like chlamydia or HPV can progress without symptoms, causing pelvic inflammation, cervical changes, or fertility issues down the line.
Let’s be clear: you deserve testing without judgment. You deserve answers without shame. Whether you’re in a monogamous relationship or exploring something new, testing is care, not confession.
The Testing Gap: What Happens When WLW Aren’t Included
Even major health systems like the CDC and WHO have only recently started improving guidance for WSW (women who have sex with women). Much of the earlier data simply didn’t study queer female populations in depth. As a result, standard guidelines often skip recommendations that apply directly to you, leaving a patchwork of advice that many providers don’t feel confident in interpreting.
That’s where confusion starts. Should you test for gonorrhea if you’ve only had oral sex with women? Yes. Should you test for chlamydia if you’ve never had vaginal intercourse with a man? Also yes. These infections don’t require penis-in-vagina sex to be transmitted, and that’s exactly the kind of myth this article is here to dismantle.
We’ll talk next about exactly which tests to consider, when to test based on your activity, and what to expect if you test positive. But first, let’s get one thing straight: lesbian sex can be beautiful, intimate, loving, rough, romantic, casual, sacred, and still, biologically capable of STD transmission. Pretending otherwise only keeps people sick and scared in silence.
What Tests Matter If You’re Only Having Sex with Women?
Let’s break the myth that there’s a “lesbian-only” STD panel. There isn’t. If you’ve had oral, vaginal, or anal sex, or shared toys, with another person, then you’re eligible for the same testing options as anyone else. The difference is in how providers talk to you, or if they bother to offer the right tests at all.
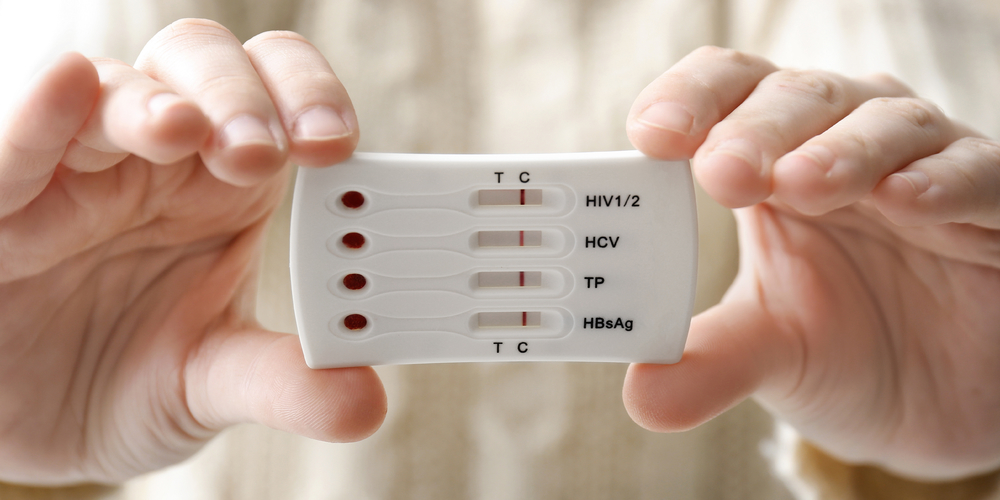
Here’s how it usually works: NAAT (nucleic acid amplification tests) are used to detect chlamydia, gonorrhea, and trichomoniasis. These use urine or vaginal swabs and are considered highly accurate. Blood tests are used for syphilis, herpes (depending on the type), and HIV. HPV testing is done via cervical swab during a Pap smear or specific HPV DNA tests, but most at-home tests don’t include it.
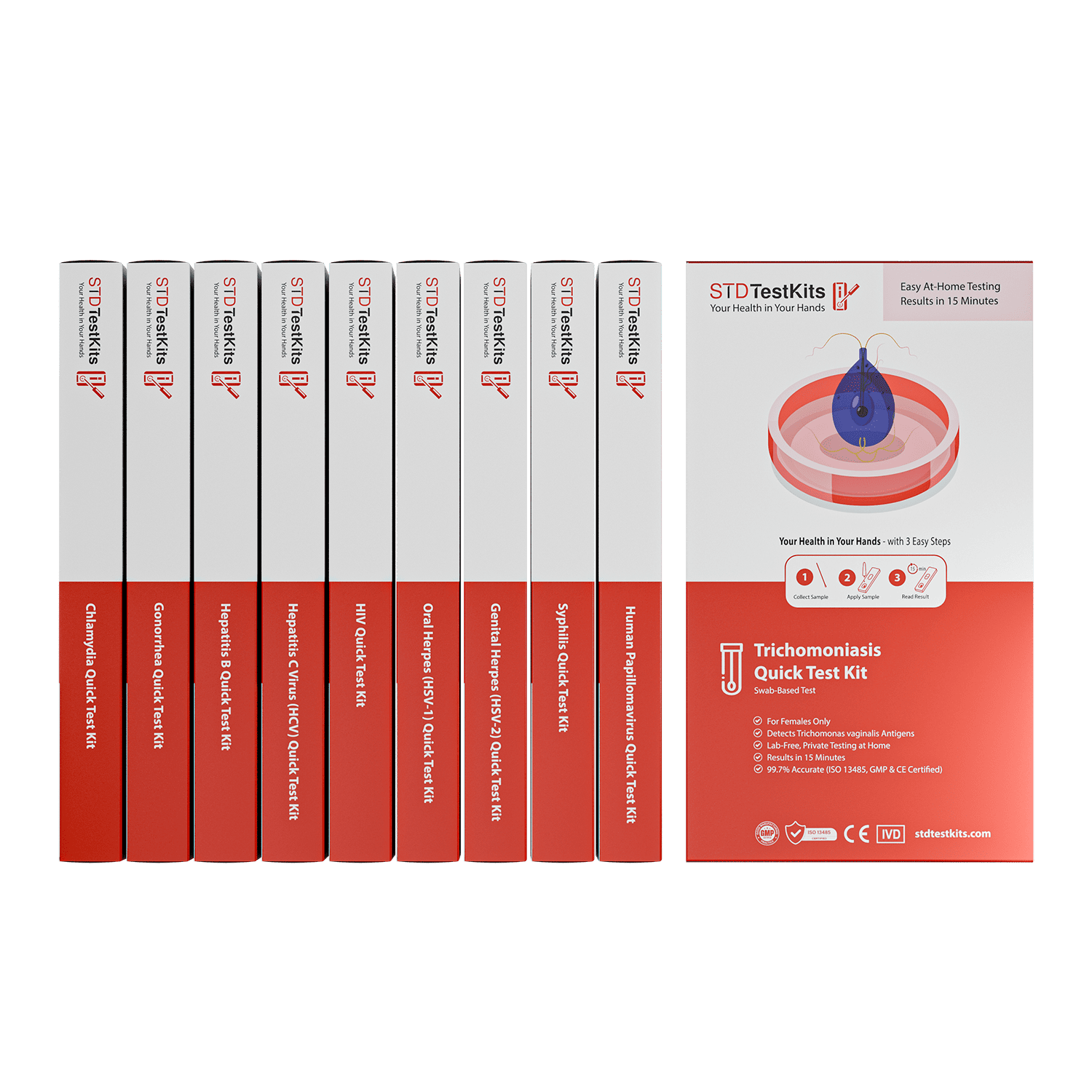
If you’re using an at-home STD test kit, make sure it includes genital and oral exposure testing. Some tests only look for a few infections, missing common exposures in WLW relationships. If you’ve shared sex toys, had oral sex, or had any genital contact, a Combo STD Home Test Kit is a smart place to start.
Table 2: Types of STD tests relevant to queer women, how they work, and if you can access them from home.
Protection Talk: What Actually Works (And What Gets Ignored)
Dental dams are real. So are finger condoms and latex gloves. But let’s be honest: very few people use them. In multiple surveys of queer women under 35, fewer than 10% reported using protection regularly during oral or digital sex. Why? Because they weren’t taught to. And because nobody told them those acts could transmit anything at all.
Adriana, 24, put it this way: “We were safe. I mean… we didn’t use toys. Just hands and mouths. It didn’t even occur to me that you could get chlamydia that way.” But yes, you can. Especially if fingers touch vaginal fluids and then go mouth-to-genitals, or if oral sex is unprotected with someone who carries an oral HSV-1 or HSV-2 infection.
Protection can help. But so can conversation. Testing together. Being honest about past exposures without assuming anyone is “clean” by default. The real goal here isn’t to scare anyone into panic, it’s to normalize tools that let us care for each other.
It’s okay if you’ve never used a dental dam. You’re not alone. The more important step is being open to learning what works, how to reduce risk without ruining the moment, and how to test regularly as a form of self-love and partner respect.
When Should You Test After Exposure?
Timing is everything. A common mistake is testing too early, before the infection can be detected. Each STD has a “window period,” the time between exposure and when a test can reliably pick it up. Testing during the window might give you a false negative and a false sense of safety.
If it’s been less than 5 days since a new partner, most tests won’t catch anything yet. Around 7–14 days in, chlamydia and gonorrhea can be detected by NAAT. For syphilis and HIV, you may need 3–6 weeks before antibodies or antigens are high enough to trigger a positive. That’s why many people retest around 30 days even if their early test comes back negative.
Case example: Lara and Jasmine hooked up after a music festival. It was spontaneous, no toys, no barrier protection. Lara tested herself 4 days later “just in case”, it came back negative. But two weeks later she started having unusual discharge. A second test confirmed trichomoniasis. Her first test had been too early. The second one gave her real answers, and relief once she started treatment.
If your head keeps spinning, peace of mind is one test away. A discreet kit like the Combo STD Home Test Kit can help you get clarity, fast. And you can retest again later if needed, on your terms.
Signs You Might Be Ignoring: Silent Infections in Queer Women
Many STDs are asymptomatic, meaning they show no symptoms at all. That’s especially common with chlamydia, HPV, and trichomoniasis. Others, like herpes, can present as tiny fissures that heal fast and don’t look like classic blisters.
For WLW (women loving women), symptoms can be mistaken for yeast infections, razor burn, or even friction. That leads to self-treatment instead of testing. And it’s understandable, after all, if no one ever explained what to look for, how would you know?
Watch for these subtle signs:
- Genital itching or irritation after oral sex •
- Vaginal discharge that smells metallic or fishy
- Pain during internal stimulation
- Sores that come and go in the same spot
- Unexplained urinary burning without UTI
Don’t brush these off. You don’t have to be paranoid, just tuned in. If you feel “off” and it’s not resolving, trust your body. Testing is private, easy, and gives you answers no article can.
What Happens If You Test Positive?
First things first: testing positive doesn’t make you dirty, reckless, or broken. It makes you human. Most STDs are treatable, some with a single dose of antibiotics, others with long-term management plans that keep you healthy and non-contagious.
But still, that moment when you see the result can hit like a punch. Samira, 31, remembers getting her positive herpes result from an at-home kit. “I sat in my car for twenty minutes. I didn’t even cry, I just felt numb. Then I messaged my last partner and told her I was scared. She replied: ‘Me too. We’ll figure it out.’”
Here’s what happens next. If it’s chlamydia, gonorrhea, or trichomoniasis, your provider or telehealth service can prescribe antibiotics. You’ll likely be told to wait 7 days before any sexual contact and to notify any recent partners. If it’s herpes, you may be offered daily antiviral medication. HPV and HIV follow different care paths, screening, monitoring, or treatment based on viral type and progression.
Many people choose to retest 3–4 weeks after treatment to confirm clearance. And yes, that’s a wise move. But what matters most is moving from panic to plan. You can live a full, healthy, sex-positive life with or after any of these diagnoses.
People are aslo reading: The STDs That Can Lead to Cancer
How to Talk to Your Partner, Without Shame
This is where many people freeze. Telling a partner you tested positive brings up shame, fear, and the terror of being rejected or blamed. But it’s also an act of care. And more often than not, people respond with compassion, especially in queer communities where mutual trust is core.
You don’t need a script, but you do need clarity. Keep it factual. You can say: “I got tested after we were together, and I tested positive for [infection]. I wanted you to know because you might want to get tested too.” You don’t have to explain every past hookup, every timeline. The goal is to share enough so they can protect their own health too.
For some, anonymous partner notification services through health departments or telehealth platforms are helpful. Others choose to text or talk in person. Either way, remember this: you are not confessing a crime. You’re being responsible, loving, and real.
Preventing Reinfection, And What Safer Sex Looks Like for WLW
Let’s say you’re treated and clear. You’re ready to have sex again. What now?
First, finish your treatment completely, even if symptoms clear before the meds are done. Wait the recommended number of days (usually 7) after antibiotics before resuming sex. If your partner was also treated, make sure you both wait, otherwise, reinfection is possible.
Then, talk about what protection looks like in your relationship. Will you use barriers for oral? Will you sanitize toys between partners or use condoms on them? Is routine testing every 3 to 6 months something you’re both open to?
Protection doesn’t have to be awkward. It can look like care. Like pausing to put on a glove before internal touch. Like sharing your last test date over dinner, not as a test of trust, but a sign of it. Like choosing a test kit together the way some couples shop for lingerie: not because something’s wrong, but because connection deserves intentionality.
If you’re not sure where to start, the STD Rapid Test Kits site has options for individual and couple testing, shipped discreetly and fast. It's an easy way to normalize check-ins without a whole doctor's visit.
How Often Should You Test, Even Without Symptoms?
Many infections fly under the radar. That’s why symptom-free testing matters. For queer women who are sexually active with new or multiple partners, a good rhythm is every 6 months. If you’ve had unprotected sex with someone whose status you don’t know, consider retesting at the 4-week and 12-week marks depending on the STD.
Routine screening is especially important for HPV, chlamydia, and herpes. Even if you’ve had a negative test in the past, new exposures can change that, and many infections stay dormant before flaring up or becoming detectable. The only way to truly know your status is to test regularly, not just when symptoms appear.
And remember: testing doesn’t mean you think someone is dirty. It means you respect yourself enough to want answers. And that’s a pretty badass move.
Whether you're navigating hookups, building a new relationship, or just need to calm your anxiety after a risky night, you don’t have to wait and wonder. This at-home combo test kit checks for the most common STDs discreetly and quickly.
FAQs
1. Can you really get an STD from lesbian sex?
Yes, absolutely. If there's skin-to-skin contact, fluids, toys, mouths, there's risk. You don't need a penis involved for STDs to spread. Herpes, HPV, chlamydia, and trichomoniasis are all passed this way. If you've ever shared toys or gone down on a partner, you're not immune, and you're not alone either.
2. But we didn’t use toys or anything, could I still get something?
Yep. Toys aren’t the only way. Think fingers that go from one vulva to another without washing. Oral sex with someone who has an active (or dormant) herpes infection. Even dry humping without clothes can pass certain STDs if there’s friction and fluids involved. It doesn’t have to be “full” sex to carry risk.
3. Do I really need to test if I feel fine?
Totally understandable to wonder. But here’s the deal: most STDs don’t come with a drumroll. Infections like chlamydia or HPV often have zero symptoms. You could feel great and still be carrying something. Regular testing is like brushing your teeth, it’s not about a crisis, it’s about routine care.
4. How soon after sex should I test?
It depends on the infection. Some tests, like those for chlamydia, can show up in 1–2 weeks. For some, like syphilis or HIV, it takes 3 to 6 weeks. If it’s been a few days since a hookup, hold off just a bit, then test, and maybe test again later. One reader told us she tested negative on day 4, but positive for trich on day 16. Timing matters.
5. Can I get herpes even if my partner didn’t have visible sores?
Unfortunately, yes. Herpes can shed even when there’s no visible outbreak. That’s why people unknowingly pass it on. It’s not about someone hiding something, often, they genuinely don’t know. That’s also why testing (and conversations) matter so much.
6. I’ve only been with women. Do I still need a full STD panel?
100%. STD risk doesn’t care about gender, it cares about behavior. If there’s oral, genital, or toy use, you’re at risk for infections like herpes, HPV, chlamydia, and gonorrhea. Even if you’ve never been with a man, you still deserve comprehensive testing. And yes, many at-home kits are designed for that.
7. Do doctors even take this seriously if I say I’m a lesbian?
Sadly, not always. We’ve heard too many stories of WLW being told they don’t need to test unless they’ve been with men. That’s outdated and wrong. If your doctor brushes you off, you have every right to seek testing on your own. Services like STD Rapid Test Kits exist for exactly this reason, so no one gets left out.
8. What if my partner gets offended when I bring up testing?
Then it’s time for a real conversation. Testing isn’t an accusation, it’s a way of saying, “I care about both of us.” If someone takes that as a threat instead of a shared responsibility, that’s not on you. One reader told us she and her new girlfriend tested together before their first night, it made them closer, not weirder.
9. Can I really test from home without seeing a doctor?
Absolutely. At-home kits today are discreet, accurate, and medically backed. They’re not sketchy supermarket gimmicks. You collect the sample yourself (urine, swab, or fingerstick), and get results privately. It’s safe, fast, and puts you in charge. No waiting rooms, no awkward small talk with reception.
10. If I tested negative, why am I still having symptoms?
Great question, and super common. It could be timing (too early), the type of test, or something else entirely like a yeast infection or BV. If your symptoms don’t go away, get a retest or talk to a provider. Don’t gaslight yourself just because the first test came back clean. Your body’s trying to tell you something, listen in.
You Deserve Answers, Not Assumptions
If you’ve read this far, you already know that silence won’t keep you safe. Queer women deserve sex ed that’s honest, testing that’s inclusive, and healthcare that doesn’t pretend you don’t exist. You shouldn’t have to guess whether that itch means something. You shouldn’t have to explain your identity just to be taken seriously.
Your sexual health is real, valid, and worth protecting. Don’t wait until you’re panicking or symptoms appear. Make testing a regular part of how you care for your body, and how you show care to others. You’re not overreacting. You’re being proactive.
Don’t wait and wonder, get the clarity you deserve. This home test kit checks for the most common STDs quickly and without drawing attention to itself.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. Women Who Have Sex with Women - STI Risk and Counseling
2. About HPV – How It Spreads and What to Know
3. Sexually Transmitted Infections – Overview and Modes of Transmission
4. Sexually transmitted infections among women who have sex with women
5. Sexually Transmitted Diseases: Symptoms & Causes
6. Sexually transmitted infections and female reproductive health: Review on HSV and HPV among women
7. Sexually Transmitted Infections Among Women Who Have Sex with Women
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Anika Holmes, MPH | Last medically reviewed: November 2025
This article is for information only and should not be used as medical advice.