When the STD Test Says “Negative” But Your Body Says “Something’s Wrong”
Quick Answer: STD test avoidance is often fueled by fear, stigma, and denial, not facts. Many people avoid testing because they feel ashamed, believe they "don’t look sick," or are scared of what a positive result could mean. But waiting doesn't erase the risk, it often makes things worse.
When Silence Feels Safer Than Testing
STD testing requires confronting a possibility that many people aren't emotionally prepared for. In moments of uncertainty, denial becomes a defense mechanism. It’s easier to assume you’re “probably okay” than to face what a test might confirm. For many, embarrassment outweighs logic.
Take Ravi, for instance. He’s in his early thirties, recently started seeing someone new, and has noticed a faint burning sensation after urinating. He tells himself it’s dehydration. Or maybe stress. He’d rather hydrate and wait than go to a clinic where someone might judge his sex life. He avoids the test because the thought of a diagnosis, and the imagined shame tied to it, is too overwhelming.
This is what psychologists call "motivated reasoning." We make sense of unclear situations in a way that makes us look good. STD testing threatens that image by making us feel “dirty,” “irresponsible,” or “at risk.” In truth, none of those labels are accurate, but stigma makes them feel real.
The Denial Spiral: How Delay Turns to Damage
What begins as embarrassment can spiral into long-term denial. A slight symptom is ignored. A hookup is minimized. Weeks go by. Then months. Often, people in denial don’t even realize how much time has passed, they’ve convinced themselves there’s nothing wrong.
This delay creates a silent risk, especially with STDs like chlamydia and gonorrhea, which can cause serious complications like infertility or chronic pain if left untreated. Because these infections are frequently asymptomatic, people may wait until a partner discloses a diagnosis, or until symptoms get severe, before they seek care.
In a CDC study, over 70% of women and more than 50% of men with chlamydia reported no symptoms at all. That means most cases go undetected unless people test proactively. But proactive testing requires one thing: facing the possibility of a result you don’t want to see.
Table 1. Many STDs produce no symptoms at first, which increases the likelihood of delayed testing, and long-term health risks.

People are also reading: Think You Have HIV? Why Testing Too Early Can Backfire
It’s Not Just Embarrassment, It’s Identity
Testing isn’t just a medical act, it’s a symbolic one. To test for an STD is to acknowledge that you might have one. And that’s where many people freeze. Because culturally, we’ve been taught that STDs are “dirty,” immoral, or shameful. So testing feels like an admission.
Jessica, 24, shared that she avoided testing for months after a condom broke during a hookup with someone she barely knew. “I kept thinking, ‘If I go get tested, that means I’m the kind of person who gets STDs.’ It wasn’t just fear, it felt like I was confessing something.”
This internalized stigma is powerful. It tells us that even though we did something human, had sex, we should feel bad about it. That if we were “careful enough,” we wouldn’t be in this situation. But STDs don’t care about judgment. They transmit through biology, not morality. And denying them doesn’t prevent them, it just delays care.
Denial vs. Delay: What’s the Emotional Difference?
Not everyone who delays testing is in denial. Sometimes it's about the logistics: a full schedule, not enough clinics nearby, or worries about the cost. But avoiding feelings often seems like being practical.
Let’s say Malik tells himself, “I’ll wait until next month, when things calm down.” But deep down, the thought of a positive test scares him. He isn’t ready to talk to a partner. He isn’t ready to see it written down. That’s not scheduling, that’s shielding. Denial is not only deceiving others; it is also a means of safeguarding oneself from uncomfortable realities.
In psychology, this process is called avoidance coping. It's common, especially when the possible outcomes seem too emotionally charged to deal with. But it comes at a cost: every day you delay a test is another day you may unknowingly expose someone else, or worsen your own health outcomes.
The Role of Gender and Culture in Testing Avoidance
STD denial doesn’t exist in a vacuum. Cultural norms, gender expectations, and how people are taught to think about sex and responsibility all have an effect on it. For many men, for example, there’s an ingrained belief that seeking care, or showing fear, means weakness. So instead of admitting they’re worried, they ignore the signs.
Connor, 36, knew he had a sore on his penis. He also knew what it could mean. But for three weeks, he convinced himself it was a skin irritation or a shaving cut. “I couldn’t even say the word herpes out loud,” he later admitted. “I thought, if I don’t test, it’s not real.”
In some cultural communities, discussing sex outside marriage, or acknowledging sexual health risks, is taboo. People who are LGBTQ+ may feel even more shame if they grew up in places where their identities were looked down upon. All of these pressures make people feel like getting tested isn't just about health; it's also about going against their values.
And yet, statistics tell a different story: STDs don’t discriminate. In fact, the CDC reports that half of all new STD infections occur in people aged 15 to 24, many of whom are navigating early adulthood, new relationships, and the weight of cultural expectations all at once.
Scared of the Result? You’re Not Alone
One of the most common reasons people avoid testing has nothing to do with symptoms, and everything to do with fear. What if it’s positive? What will I tell my partner? Will I ever date again? These questions don’t just echo, they scream. And the louder they get, the harder it becomes to take action.
Jasmin, 29, delayed getting tested for HIV for over a year after a risky encounter. “I was convinced a positive test would destroy my life,” she said. “I thought it meant I could never be loved.” Her fear wasn’t rooted in medical facts, it was emotional. But emotions are powerful motivators.
This fear of knowing is rooted in what psychologists call “catastrophic thinking.” Instead of seeing a test as a tool for clarity, people imagine worst-case scenarios: being abandoned, being untreatable, being forever changed. But these fears rarely match reality. Today, most STDs are treatable, and those that aren’t, like herpes or HIV, are manageable with early intervention.
Table 2. Common fears that fuel STD denial, and what the actual facts reveal.
The “No Symptoms = No Problem” Myth
Perhaps the most damaging thought of all: “If I had something, I’d know.” But most STDs don’t scream for attention. They whisper, or stay completely silent. In fact, the absence of symptoms is the rule, not the exception, for many infections.
This myth is especially dangerous because it feels logical. We’ve been trained to associate illness with symptoms: fever, pain, fatigue. But STDs often bypass that logic. For example, HPV in men usually shows no signs at all, yet it can still be passed to partners and, in some cases, cause cancer later in life. Chlamydia can silently damage the reproductive system without causing a single symptom until it’s too late.
When people say, “I’m fine,” what they really mean is, “I feel fine.” But those two things aren’t the same. You can feel completely normal and still carry an infection that harms you, or someone you care about. And this is why routine testing matters. Not because you’re certain something is wrong, but because you know symptoms aren’t a reliable guide.
Think of testing like checking your tire pressure. You don’t wait for a blowout. You do it because you value safety, and because early action prevents damage.
What Testing Actually Looks Like (Spoiler: It’s Not That Bad)
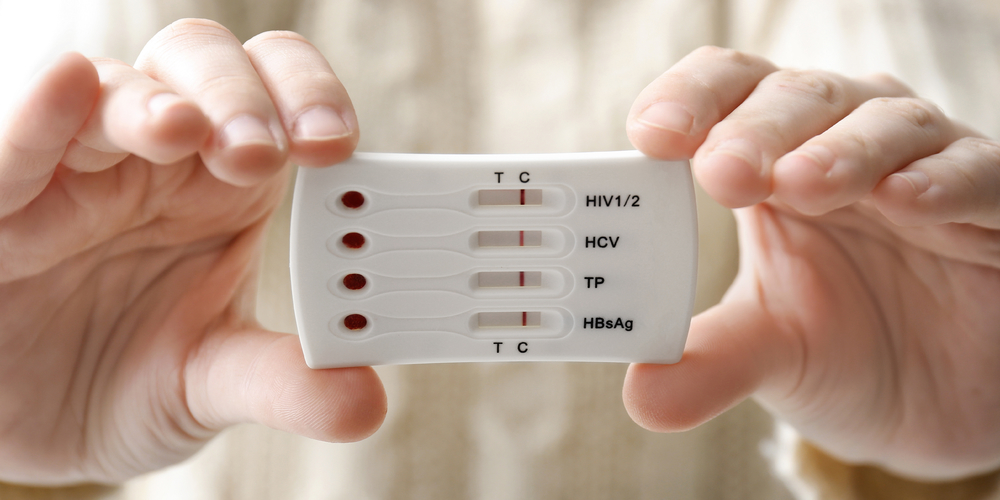
Sometimes denial is powered by imagination. People picture long, awkward conversations. Cold exam rooms. Painful swabs. Judgmental looks. But most modern STD testing, especially at-home kits, is fast, easy, and private.
With a rapid home test, you collect your own sample, often a finger prick or urine sample, and get results in minutes. There’s no need for a clinic visit, no awkward waiting room, and no one else has to know unless you choose to tell them. And with discreet shipping and clear instructions, the process is designed to reduce, not increase, your anxiety.
For those who prefer clinical care, many providers now offer telehealth consultations, mail-in lab tests, and nonjudgmental counseling. Today’s testing landscape is about access and autonomy, not shame and punishment.
Peace of mind doesn’t have to come at the cost of your dignity. If you’re scared, that’s normal. But you can still act. This at-home combo test kit offers fast results for multiple infections, all from your own bathroom, in total privacy.
People are also reading: HIV Rapid Test Errors and Faint Lines: How to Know What’s Real
Case Study: “I Waited Too Long. Here’s What Happened.”
Lucas, 31, had been in a situationship for a few months. Things were casual, unspoken, undefined. He hadn’t been tested since his last relationship ended over a year ago. “I didn’t want to seem suspicious or insecure,” he explained. “So I just... didn’t bring it up.”
When Lucas developed a mild discharge and some burning, he told himself it was a UTI. He bought cranberry pills, drank more water, and waited. Three weeks later, the pain was worse. He finally got tested, turns out, it was gonorrhea. And the worst part? He’d unknowingly passed it to his partner, who had no symptoms at all.
“I thought I was being cool by not freaking out,” he said. “But I was just scared. Scared of what it would mean, what she’d think, what I’d think of myself. I wish I’d tested sooner. It would’ve saved us both.”
Lucas’s story isn’t rare. It’s a perfect example of how emotional discomfort delays practical action. His avoidance wasn’t about access or cost, it was about fear of what testing would say about him.
How Denial Affects Partner Health and Trust
When one person avoids testing, the consequences often extend beyond their own body. Partners are affected, physically and emotionally. Even if there’s no transmission, trust can be eroded if someone finds out they were unknowingly exposed due to a partner’s avoidance.
STD denial can quietly fracture relationships. Not because someone was dishonest about a test result, but because they were never willing to get one. Being afraid of testing is human. But pretending the risk doesn’t exist is where things get dangerous.
If you’re worried about how a partner might react, consider this: most people respond better to honesty than secrecy. A simple, “Hey, I care about you and I think we should both get tested,” isn’t a threat, it’s a gesture of respect. And if they shame you for bringing it up? That’s not on you.
Testing is not just a health move. It’s an intimacy move. It says, “I want us both to be safe. I’m not afraid to know.”
Breaking the Cycle: How to Move Past the Fear
So how do you move from frozen to forward? The first step is naming what you’re feeling. Say it out loud: “I’m scared to get tested.” That’s not weak, it’s real. When you acknowledge the fear, you take away its power. You give yourself room to act anyway.
Next, remind yourself what testing actually means: it means you care about your health. It means you’re willing to face facts, even hard ones. And if you do test positive? That’s information, not condemnation. You’ll have a path forward. You’ll know what to do.
Most people who delay testing later say the same thing: “I wish I’d done it sooner.” Because the truth, even when uncomfortable, is almost always better than the anxiety of not knowing.
If you're still hesitating, ask yourself: would I rather carry worry around for weeks, or spend a few minutes getting answers I can act on? Testing doesn’t just check for STDs, it clears space in your mind and your life. Return to STD Rapid Test Kits and find a test that fits your comfort level, privacy needs, and timing.
FAQs
1. I feel fine. Why should I even bother getting tested?
Totally fair question, and it’s exactly why so many STDs go undetected. The truth? Feeling fine doesn’t always mean you are fine. Infections like chlamydia and HPV often show zero symptoms for months (or ever), but they can still spread to partners or cause complications down the line. Testing isn’t overkill. It’s just smart.
2. Why does even thinking about testing make me panic?
Because it taps into deep stuff, shame, fear, past experiences, maybe even trauma. Getting tested means facing a possibility your brain is actively trying to avoid. But here’s the reframe: testing is an act of courage, not confession. You’re not guilty. You’re just taking care of your body, which is kind of a badass thing to do.
3. What if I find out I have something? I don’t know if I can handle that.
We hear you. No one wants that moment. But the reality is, most STDs are treatable. And even the ones that stick around (like herpes or HIV) are manageable with treatment. Finding out means you can act. Not knowing means you just carry that fear around. You deserve more than fear.
4. Can I get tested without my roommates, partner, or parents finding out?
Yes, yes, and yes. At-home kits come in plain packaging, no logos, and you don’t have to leave your space or talk to a soul. Some even send digital results. You get privacy, control, and peace of mind, without that awkward pharmacy counter vibe.
5. Can I still give someone an STD even if I don't have any signs?
Absolutely, and this is where it gets real. STDs don’t wait for symptoms to start spreading. You can feel 100% fine and still pass something to someone else. Because of this, it's dangerous to rely on "feeling normal" rather than getting tested, particularly if you have multiple partners or a new one.
6. I’m in a monogamous relationship. Do I still need to test?
That depends. If you both got tested before becoming exclusive and haven’t had other partners since, you’re likely in the clear. But if either of you skipped testing (no shame, lots of people do), it’s worth doing now. Monogamy doesn’t protect you retroactively.
7. My partner doesn’t want to test. What do I do?
That’s rough, and also a conversation worth having. Testing isn’t about mistrust. It’s about mutual care. Try framing it like, “I care about us and want us both to feel safe.” If they shut it down entirely? That says more about them than it does about you.
8. How often should I be getting tested, really?
Think of testing like dental cleanings, regular and preventative. Once a year is a good baseline if you’re monogamous or not super active. Every 3–6 months is smart if you’ve got new partners, multiple partners, or you’re just playing it safe. Testing isn’t just reaction, it’s routine care.
9. Are at-home tests actually accurate, or just a gimmick?
Legit question. And here’s the real answer: if you buy from a reputable provider (like us), the accuracy is seriously solid. Most at-home tests use the same tech as clinics. Just follow the instructions, and if anything looks weird or uncertain, you can always confirm with a lab test.
10.Okay, but… is it normal to feel this anxious about testing?
One hundred percent. You’re not weird. You’re not dramatic. Testing touches all the tender spots, shame, identity, health, relationships. But the truth is, people who test aren’t more at risk. They’re just more in control. And that’s something to be proud of.
You Deserve Answers, Not Assumptions
The hardest part isn’t usually the test, it’s getting yourself to take it. But if you’ve read this far, you already care. You're moving forward already. And that deserves recognition, not shame.
STD denial isn’t weakness, it’s fear misdirected. But you can rewrite that story. You can make knowing your truth the bravest thing you do today.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit swiftly and covertly checks for the most prevalent sexually transmitted diseases.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. CDC: Guidelines for STD Prevention and Testing
2. STD Facts from the World Health Organization
3. Getting Tested for STIs | CDC
5. STI Screening Recommendations | CDC
6. Sexually transmitted diseases (STDs) - Diagnosis and treatment | Mayo Clinic
7. Exploring Facilitators and Barriers to STD/STI/HIV Self-Testing | NCBI
8. Relationships Between Perceived STD-Related Stigma and Screening | NCBI
9. Barriers to Asymptomatic Screening and Other STD Services | NCBI
10. Reducing STI Cases: Young People Deserve Better Sexual Health | Guttmacher Institute
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Dr. Lana Bright, PhD, MPH | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.